What to expect in the final stages of lung cancer is a crucial topic for those facing this challenging diagnosis. This journey involves navigating a complex web of physical, emotional, and practical considerations. Understanding the progression of symptoms, available treatment options, and the impact on daily life is paramount. This guide will explore the various aspects of this stage, offering insights into palliative care, emotional support, end-of-life choices, and available resources.
The final stages of lung cancer present a unique set of challenges, requiring a multi-faceted approach to care. This guide will cover the spectrum of experiences, from symptom management and treatment options to end-of-life care and support systems. We will delve into the emotional and psychological aspects for both patients and families, emphasizing the importance of quality of life and support networks throughout this challenging time.
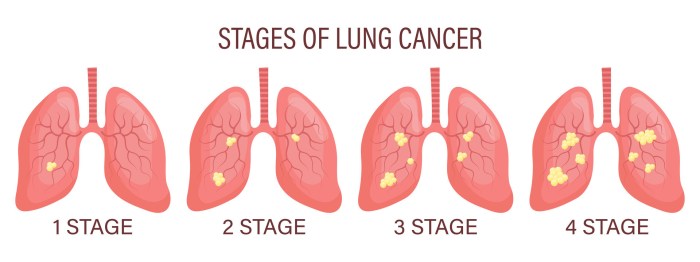
Symptoms and Progression
The final stages of lung cancer are characterized by a progressive decline in health, with symptoms intensifying as the disease advances. Understanding these symptoms is crucial for both patients and caregivers to navigate this challenging period with compassion and informed decision-making. Managing symptoms effectively is vital to maintaining comfort and quality of life.
Respiratory Symptoms
Respiratory symptoms often dominate the final stages of lung cancer. These symptoms stem from the tumor’s impact on the lungs and airways, potentially obstructing airflow and causing significant discomfort. The severity and nature of respiratory symptoms can vary based on the specific type of lung cancer and the extent of its spread. For instance, small cell lung cancer often displays rapid progression, resulting in more acute respiratory distress.
- Shortness of breath (dyspnea) is a common and often distressing symptom. It can range from mild difficulty breathing to severe, labored breathing that necessitates continuous supplemental oxygen. As the disease progresses, the frequency and severity of episodes of dyspnea typically increase, often impacting daily activities.
- Coughing, often with increased mucus production, is another common respiratory symptom. The mucus may be tinged with blood, and the coughing can be persistent and exhausting. The intensity of the cough and the amount of mucus produced tend to worsen over time, potentially interfering with sleep and rest.
- Wheezing, a whistling sound during breathing, can arise from narrowing of the airways. Wheezing can be intermittent or continuous and can indicate a worsening condition. The severity of wheezing may fluctuate but generally progresses to a more persistent state as the disease progresses.
Pain Symptoms
Pain is another significant symptom in the later stages of lung cancer. It can originate from the tumor itself, its spread to surrounding tissues, or from the side effects of treatment. The location and intensity of pain can differ significantly depending on the tumor’s location and the extent of its spread. Bone pain is frequently reported due to the cancer’s potential to metastasize to the skeletal system.
- Bone pain is a prevalent symptom, often originating from the spread of cancer cells to the bones. This pain may be dull or sharp, localized or diffuse, and can range from mild discomfort to severe agony. The pain is often worse at night and may be aggravated by movement or pressure.
- Chest pain, often described as a dull ache or pressure, is frequently associated with lung cancer. This pain may worsen with coughing or deep breathing. The intensity of chest pain can vary, but it tends to increase as the disease progresses.
- Headaches, which may be associated with brain metastasis, are also a potential pain symptom in advanced lung cancer. These headaches can be persistent and intense, impacting quality of life significantly. Headaches may increase in frequency and severity over time.
Fatigue Symptoms
Fatigue is a prevalent symptom in advanced lung cancer, often described as an overwhelming tiredness or lack of energy. It can stem from various factors, including the disease itself, treatment side effects, and the overall decline in the body’s function.
- Extreme fatigue is a hallmark of advanced lung cancer. It’s often debilitating and can severely limit a person’s ability to perform daily tasks. The fatigue tends to increase as the disease progresses, leading to significant functional limitations.
Symptom Progression Table
| Time Elapsed Since Diagnosis (Months) | Symptom Severity | Example Cases |
|---|---|---|
| 0-3 | Mild respiratory symptoms, occasional pain | Patient experiencing mild shortness of breath, infrequent cough |
| 3-6 | Increasing respiratory distress, moderate pain | Patient requiring supplemental oxygen, experiencing more frequent and intense coughing episodes, moderate bone pain |
| 6-12 | Severe respiratory compromise, significant pain | Patient requiring frequent oxygen therapy, experiencing severe dyspnea, significant bone pain and fatigue |
| 12+ | Rapid decline in respiratory function, debilitating pain | Patient requiring continuous oxygen support, experiencing severe dyspnea, widespread debilitating pain and fatigue, potentially requiring palliative care |
Treatment Options and Palliative Care
Facing the final stages of lung cancer requires a compassionate and holistic approach, focusing not just on extending life, but on maximizing comfort and quality of life. Palliative care plays a crucial role in managing symptoms and providing support for both the patient and their loved ones. This approach emphasizes relief from the suffering caused by the disease and its treatment.Effective management of symptoms, like pain, shortness of breath, and fatigue, is paramount in the final stages.
Palliative care specialists work closely with oncologists to tailor a treatment plan that addresses the patient’s specific needs and preferences. This personalized approach ensures that interventions are both effective and well-tolerated.
Facing the final stages of lung cancer can be tough, with symptoms like increasing shortness of breath and pain becoming more prominent. While there’s no magic bullet, maintaining overall well-being is key. Recent research into the impact of gut health on overall wellness, particularly a fascinating sauerkraut gut health study , suggests that supporting a healthy microbiome might offer some comfort during this challenging time.
Ultimately, the best approach is to focus on comfort, and connect with support systems during these final stages.
Available Treatment Options for Symptom Management
Various treatment options are available to alleviate symptoms in the advanced stages of lung cancer. These options often involve a combination of medications, therapies, and supportive care measures. Medications are crucial for managing pain, nausea, and other distressing symptoms. Specific drugs and dosages are carefully adjusted based on individual needs and response.
Palliative Care Approaches
Palliative care encompasses a range of interventions to improve quality of life for patients with serious illnesses. Different palliative care models may emphasize different aspects of patient care, such as symptom management, psychosocial support, or spiritual guidance. Some models prioritize comprehensive care, addressing physical, emotional, and spiritual needs holistically. Others focus more specifically on symptom relief. The choice of model often depends on the patient’s preferences and the resources available.
Pain Management Strategies
Pain management strategies are crucial in the final stages of lung cancer. Initial pain management may involve opioid analgesics, but the dosage and type may need adjustment as the disease progresses and tolerance develops. Non-opioid pain relievers, such as acetaminophen or ibuprofen, can be used in combination with opioids to enhance pain relief and reduce opioid side effects.
Techniques like nerve blocks or interventional procedures may also be considered for specific types of pain.
Facing the final stages of lung cancer can be tough, marked by fatigue and potential discomfort. While focusing on comfort and quality of life is paramount, it’s also important to be aware of other potential health concerns that might arise, such as those related to macular degeneration. Understanding the risk factors for macular degeneration, like age and genetics, can be helpful in navigating potential complications.
For more information on macular degeneration causes and risk factors, check out this helpful resource: macular degeneration causes risk factors. Ultimately, the goal is to manage symptoms and maintain a sense of well-being during this challenging time.
Supportive Care
Supportive care is an essential component of palliative care, providing emotional, psychological, and practical support for patients and their families. Counseling and emotional support can help patients and their families cope with the emotional challenges of the disease and its progression. Spiritual guidance and support can be particularly important in addressing existential concerns and promoting a sense of peace.
Practical support may include assistance with daily living activities, financial planning, or navigating healthcare decisions.
Common Palliative Care Interventions, What to expect in the final stages of lung cancer
| Intervention | Potential Benefits |
|---|---|
| Medications for pain, nausea, and shortness of breath | Reduce suffering, improve comfort, and enhance quality of life. |
| Symptom management strategies | Improve overall well-being, allowing patients to participate in meaningful activities. |
| Counseling and emotional support | Address psychological distress, promote coping mechanisms, and provide a supportive environment for patients and families. |
| Spiritual guidance | Provide comfort, peace, and a sense of purpose during challenging times. |
| Practical support | Assist with daily tasks, financial planning, and other logistical needs. |
Impact on Daily Life and Quality of Life
Facing the final stages of lung cancer can significantly alter daily life, impacting routines and overall well-being. The physical limitations and emotional distress can make everyday tasks challenging, demanding adjustments to maintain comfort and quality of life. This section explores the practical and emotional adjustments necessary for both patients and caregivers during this difficult time.Understanding the shifting needs of a loved one with advanced lung cancer is crucial.
Recognizing the limitations and adjusting routines and environments can greatly improve the patient’s experience and well-being. Caregivers need to be prepared for potential changes in mood, energy levels, and communication, and proactively address these shifts with patience and understanding.
Adapting Daily Routines
Adjusting daily routines is essential to maintain comfort and minimize stress for patients in the final stages of lung cancer. This involves prioritizing activities that provide comfort and relaxation while minimizing those that cause undue fatigue or discomfort. Simple tasks, such as taking short breaks or choosing easier meal options, can significantly improve quality of life.
- Prioritizing Rest and Relaxation: Schedule regular periods of rest throughout the day. Even short naps or quiet time can be beneficial. Create a relaxing atmosphere, using soft lighting, calming music, or aromatherapy. Encourage the patient to engage in activities that promote relaxation, such as listening to music, reading, or gentle stretching.
- Simplifying Tasks: Break down complex tasks into smaller, manageable steps. Use assistive devices if needed to minimize physical effort. For example, using a grabber for reaching items or a raised toilet seat. This approach reduces stress and promotes a sense of accomplishment, even in small tasks.
- Modifying the Home Environment: Ensure the home environment is safe and supportive. Remove tripping hazards, install grab bars in bathrooms, and make sure lighting is adequate to avoid accidents. Consider the patient’s comfort preferences and modify the environment accordingly, such as adding comfortable seating or adjusting room temperature.
Maintaining Quality of Life
Maintaining a sense of normalcy and well-being is important. Focusing on what the patient can still enjoy, whether it’s a favorite book, listening to music, or spending time with loved ones, helps preserve a positive outlook.
- Promoting Social Connections: Encourage meaningful interactions with family and friends. Scheduled visits, phone calls, or video chats can combat feelings of isolation and loneliness. These interactions provide emotional support and connection, vital for maintaining well-being.
- Engaging in Meaningful Activities: Identify activities that bring joy and comfort. This could include hobbies, creative pursuits, or simply spending time in nature. Focusing on these activities can help maintain a sense of purpose and well-being.
- Addressing Emotional Needs: Open communication is key. Allowing the patient to express emotions and concerns is crucial. Seek professional help if needed. Counseling or support groups can provide valuable guidance and emotional support for both the patient and family.
Caregiver Support Strategies
Caregivers play a vital role in supporting patients during this challenging time. Their understanding and support are essential for maintaining the patient’s quality of life.
- Emotional Support: Acknowledge and validate the caregiver’s emotional needs. Providing resources, such as support groups or counseling, can help caregivers cope with the emotional toll of caregiving. Encouraging self-care is crucial to prevent burnout.
- Practical Support: Help with daily tasks, errands, and household chores. Coordinate with other family members or friends to share responsibilities and prevent caregiver fatigue. This ensures that the patient receives the necessary support while preserving the caregiver’s well-being.
- Communication and Understanding: Maintain open communication between the patient, family, and medical team. This shared understanding is crucial for coordinating care and addressing the patient’s evolving needs. Active listening and empathy are essential tools in this process.
Support Systems Comparison
| Support System | Effectiveness | Examples |
|---|---|---|
| Family and Friends | High, especially if close-knit | Regular visits, phone calls, shared responsibilities |
| Hospice Care | High, comprehensive care | Symptom management, emotional support, practical assistance |
| Support Groups | Moderate to High, depending on the group | Shared experiences, emotional support, resources |
| Professional Counseling | High, tailored support | Individual or family therapy, addressing emotional needs |
Emotional and Psychological Considerations
Facing a terminal illness like lung cancer brings a profound emotional and psychological toll on both the patient and their loved ones. This stage requires navigating complex feelings, processing difficult information, and supporting each other through a challenging journey. The focus shifts from treatment goals to ensuring comfort, managing symptoms, and fostering emotional well-being.Understanding and addressing the emotional landscape is crucial for maintaining quality of life and supporting a peaceful transition.
The emotional and psychological impact can manifest in various ways, from anxiety and fear to grief and acceptance. Open communication, empathy, and access to support systems are vital for navigating these complexities.
Emotional Responses to Diagnosis and Prognosis
Patients and families often experience a wide range of emotional responses to a terminal lung cancer diagnosis. These responses are highly personal and vary greatly. Denial, anger, bargaining, depression, and acceptance are common stages of grief and loss that individuals may experience. It’s essential to acknowledge these feelings without judgment, providing a safe space for processing and coping.
Coping Mechanisms and Support Strategies
Developing healthy coping mechanisms is vital for managing the emotional strain. These strategies may include:
- Seeking professional counseling or support groups: These resources can offer valuable guidance and support for navigating the emotional challenges. Support groups provide a space for sharing experiences, gaining insights, and connecting with others facing similar situations. Professional counseling can offer personalized strategies for managing stress and anxiety.
- Maintaining social connections: Maintaining relationships with loved ones, friends, and support networks is critical for emotional well-being. Social interaction and support from a strong network can buffer the impact of the illness and foster a sense of community.
- Engaging in activities that bring joy and comfort: Finding ways to enjoy life, whether through hobbies, creative pursuits, or spending time in nature, can significantly improve mood and well-being. These activities can provide a sense of normalcy and purpose during this challenging time.
Creating a Supportive Environment
A supportive environment plays a pivotal role in promoting emotional well-being. Open communication, active listening, and empathy are essential. Encouraging shared experiences and fostering a sense of connection within the family can provide comfort and strength.
- Honesty and transparency: Being open and honest about the patient’s condition, while maintaining hope and optimism, can foster trust and understanding. Sharing information in a sensitive and compassionate manner is crucial. Open dialogue about fears and anxieties can reduce the burden of uncertainty and isolation.
- Celebrating milestones and moments of joy: Acknowledging and celebrating small victories, moments of peace, and positive experiences can create lasting memories and foster a sense of gratitude. These moments can serve as anchors during challenging times.
- Respecting the patient’s wishes: Respecting the patient’s preferences and decisions regarding end-of-life care is crucial for maintaining dignity and autonomy. Ensuring that the patient’s wishes are understood and honored is paramount.
Addressing Grief and Loss
The experience of grief and loss is a natural response to terminal illness. It’s essential to acknowledge and support both the patient and their family members through this process. Grief counseling and bereavement support can be invaluable in navigating the complexities of loss.
- Allowing for emotional expression: Creating a safe space for emotional expression and allowing individuals to grieve in their own way is essential. Encouraging the sharing of feelings, memories, and stories can help in the healing process.
- Seeking professional guidance: Seeking guidance from grief counselors or therapists can offer valuable support and strategies for navigating the stages of grief. They can help individuals process emotions, develop coping mechanisms, and ultimately find healing.
- Finding meaning and purpose: Finding meaning and purpose in the face of loss can be a source of strength and resilience. Reflection on shared experiences, cherished memories, and the legacy left behind can provide comfort and a sense of closure.
End-of-Life Care and Support
Navigating the final stages of lung cancer can be emotionally challenging for patients and their families. Understanding the various end-of-life care options available and planning ahead can greatly ease this burden. This section explores the crucial aspects of end-of-life care, focusing on support, planning, and the compassionate approach healthcare professionals take.End-of-life care is not simply about prolonging life, but about maximizing comfort, quality of life, and dignity during the final stages of the disease.
It emphasizes the importance of managing symptoms, addressing emotional needs, and supporting the patient and their loved ones through this difficult time.
Advanced Directives and End-of-Life Planning
Advance directives are legal documents that Artikel a patient’s wishes regarding medical treatment if they become incapacitated. These documents ensure that healthcare decisions align with the patient’s values and preferences. Crucially, they provide a framework for care when the patient can no longer communicate their choices. Examples include living wills, durable power of attorney for healthcare, and do-not-resuscitate (DNR) orders.
Having these documents in place can significantly reduce stress and conflict during a challenging time. They empower patients to make informed decisions about their care and ensure their wishes are respected.
Hospice Care Approaches
Hospice care focuses on providing comfort and support to patients with a life expectancy of six months or less. It prioritizes pain and symptom management, emotional support, and spiritual care. Various hospice care approaches exist, each with its unique focus and benefits. Some common approaches include:
- Patient-centered care: This approach prioritizes the patient’s needs, preferences, and values, ensuring that all decisions are made in collaboration with the patient and their family. This approach often incorporates a multidisciplinary team, including nurses, doctors, social workers, and counselors.
- Symptom management: Hospice care experts focus on managing symptoms such as pain, shortness of breath, nausea, and anxiety, employing a variety of methods, including medication, physical therapies, and alternative treatments, to ensure the patient’s comfort.
- Emotional and spiritual support: Hospice care extends beyond physical needs, acknowledging the emotional and spiritual dimensions of the experience. This involves providing support and counseling to the patient and their family, offering resources for grief counseling and spiritual guidance, and helping them find meaning and peace in their final moments.
Role of Healthcare Professionals
Healthcare professionals play a vital role in providing compassionate and holistic end-of-life care. Their expertise in symptom management, communication, and emotional support is crucial for both the patient and their family. Compassionate care involves active listening, empathy, and the ability to address the diverse needs of the patient and their family. Healthcare professionals strive to provide a supportive environment that fosters dignity and respect for the patient’s autonomy.
Facing the final stages of lung cancer can be tough, marked by fluctuating energy levels and often a need for extra nutrients. While navigating these challenging times, it’s also important to consider your daily protein intake. A balanced diet, including the right amount of protein for breakfast, can be crucial for maintaining strength and overall well-being during this period.
For more detailed guidance on how much protein for breakfast, check out this helpful resource: how much protein for breakfast. Ultimately, though, focusing on comfort, support, and making the most of precious moments is key during this phase.
Types of End-of-Life Care Services
| Type of Service | Description |
|---|---|
| Hospice Care | Comprehensive care for individuals with a life expectancy of six months or less, focusing on symptom management, emotional support, and spiritual care. |
| Palliative Care | Specialized medical care that focuses on improving the quality of life for patients with serious illnesses, including lung cancer. It can be provided alongside curative treatments. |
| Grief Counseling | Support for individuals and families experiencing grief and loss, often provided by licensed counselors or therapists. |
| Spiritual Guidance | Support from religious leaders or spiritual advisors to address spiritual needs and concerns. |
| Social Work Services | Assistance with practical issues such as financial aid, legal concerns, and community resources. |
Illustrative Case Studies (No Specific Examples): What To Expect In The Final Stages Of Lung Cancer
Facing the final stages of lung cancer presents unique challenges for patients and their families. Understanding the diverse paths through this journey, including symptom management, palliative care approaches, and emotional support, is crucial for creating a supportive environment. These case studies, while fictional, illustrate common experiences and highlight the importance of personalized care plans.
Case Study 1: Challenges in Symptom Management
This fictional patient, Mr. Hernandez, experienced a rapid decline in his lung cancer. Initially, his symptoms were manageable with medication and therapy. However, as the disease progressed, he developed severe pain, shortness of breath, and nausea. These symptoms significantly impacted his quality of life, making even basic daily tasks challenging.
Mr. Hernandez’s caregivers struggled to find the right balance between medication dosages and potential side effects. His family grappled with the emotional toll of witnessing his suffering and the uncertainty of the future. They felt overwhelmed by the complex medical decisions and the constant need for adjustments to his care plan.
Case Study 2: Successful Palliative Care Interventions
Ms. Chen, a patient with lung cancer, received comprehensive palliative care from the start of her diagnosis. Her care team proactively addressed her pain and discomfort through a multi-pronged approach involving medication, physical therapy, and counseling. Ms. Chen also participated in support groups, which helped her connect with others facing similar challenges and fostered a sense of community.
Her palliative care team focused on maintaining her dignity and autonomy throughout the process, ensuring that she remained an active participant in her care decisions. The family benefited from regular communication and support from the palliative care team, which alleviated their anxiety and allowed them to focus on spending quality time with Ms. Chen.
Case Study 3: Effective End-of-Life Care Support
Mr. Lee’s end-of-life care involved a strong support network that included his family, medical professionals, and hospice workers. Hospice services provided comfort care, emotional support, and guidance for the family. The team worked closely with Mr. Lee’s family to ensure that his final days were peaceful and dignified.
They addressed the family’s emotional needs through counseling and support groups, helping them navigate the complexities of grief and loss. Mr. Lee’s family felt empowered to make informed decisions about his care and found solace in the compassion and support provided.
Emotional and Psychological Impact on Family Members
The emotional toll on family members during a terminal illness is significant. Grief, anxiety, and guilt are common feelings. Family members may struggle with communication, decision-making, and accepting the reality of the situation. Loss of normalcy, financial concerns, and the need to adjust to a new family dynamic are also potential stressors. Open communication, support from healthcare professionals, and access to counseling services are vital for navigating these challenges.
Table: Approaches to Care and Outcomes
| Case Study | Approach to Care | Outcomes |
|---|---|---|
| Mr. Hernandez | Reactive symptom management, limited access to palliative care | Significant symptom burden, decreased quality of life, family stress |
| Ms. Chen | Proactive palliative care, comprehensive support | Improved quality of life, reduced symptom burden, increased family coping |
| Mr. Lee | Hospice care, comprehensive support for family | Peaceful and dignified end-of-life experience, reduced family stress, emotional support |
Resources and Support Networks
Navigating the final stages of lung cancer can be emotionally and practically challenging, not just for the patient but also for family members and caregivers. This period demands comprehensive support to help everyone cope with the emotional turmoil and practical necessities. Understanding the available resources can significantly ease the burden and enhance the quality of life for everyone involved.Finding the right support network is crucial during this time.
It’s more than just information; it’s about connecting with people who understand the unique challenges faced by those dealing with terminal illness. This section will explore various support systems available to patients, families, and caregivers.
Support Groups and Online Communities
Support groups provide a safe space for sharing experiences, exchanging coping strategies, and receiving emotional support from others facing similar circumstances. These groups offer a sense of community and shared understanding, reducing feelings of isolation and promoting a sense of belonging. Online communities, through forums and social media groups, offer similar benefits, allowing for broader connections and accessibility across geographical boundaries.
They provide a space for open discussion, advice, and encouragement. The collective experience shared in these environments can be invaluable in navigating the complex emotions associated with end-of-life care.
Organizations Offering Support
Numerous organizations are dedicated to providing comprehensive support to those affected by lung cancer. These organizations offer a wide range of services, from emotional counseling to practical assistance with medical bills and daily tasks. They often have trained professionals who can offer expert guidance and support tailored to the specific needs of individuals and families. Examples of such organizations include the American Lung Association, the National Cancer Institute, and various local support groups.
Reputable Websites and Helplines
Accessing reliable information and resources is essential during this difficult time. Reputable websites and helplines offer a wealth of information about lung cancer, treatment options, end-of-life care, and available support services. These resources provide access to detailed information and support in a convenient and accessible format. Furthermore, many websites and helplines offer resources for caregivers and family members, ensuring comprehensive support for all involved.
Table of Support Resources
| Resource | Description | Contact Information |
|---|---|---|
| American Lung Association | Provides information, support groups, and advocacy for lung health. | (800) 586-4872 |
| National Cancer Institute (NCI) | Offers comprehensive information about cancer, including research, treatment, and support services. | (800) 422-6237 |
| [Local Cancer Support Groups] | Offer local support, often providing in-person meetings and emotional support. | Search online for local groups. |
| [Hospice organizations] | Provide comprehensive support and care for individuals facing end-of-life issues, including pain management and emotional support. | Search online for local hospice providers. |
| [Patient advocacy groups] | Represent the interests of lung cancer patients and their families, advocating for improved care and resources. | Search online for patient advocacy groups. |
Final Review
Ultimately, navigating the final stages of lung cancer necessitates a compassionate and holistic approach that prioritizes the patient’s well-being and the needs of their loved ones. This guide provides a comprehensive overview of the various aspects involved, from symptom management and treatment to emotional support and end-of-life care. Remember, you are not alone in this journey, and numerous resources and support networks are available to assist you and your family.




