What is ischemia p2? This in-depth exploration delves into the complexities of ischemia p2, examining its defining characteristics, underlying causes, potential symptoms, diagnostic approaches, treatment options, and ultimately, the prognosis and management strategies for individuals affected. We’ll unravel the mysteries behind this condition, breaking down the information into digestible pieces to help you understand the nuances of this medical concern.
Understanding ischemia p2 requires a comprehensive approach, considering the interplay of various factors. This includes defining its unique characteristics, distinguishing it from other ischemia types, and exploring the intricate pathophysiological mechanisms. Further, we’ll delve into the potential triggers, causes, and risk factors, along with the array of diagnostic methods. Ultimately, we’ll discuss treatment options and long-term management strategies.
Defining Ischemia p2
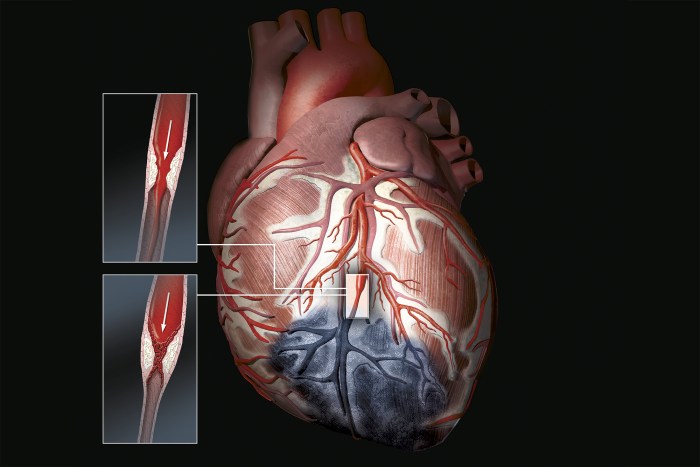
Ischemia, a condition characterized by reduced blood flow to tissues, can manifest in various forms and severities. While the general principles of ischemia remain consistent, specific subtypes, like ischemia p2, exhibit unique characteristics. Understanding these nuances is crucial for accurate diagnosis and effective treatment. This exploration delves into the specifics of ischemia p2, examining its defining features, types, pathophysiology, and underlying mechanisms.
Defining Characteristics of Ischemia p2
Ischemia p2, a specialized form of ischemia, is distinguished by a distinct pattern of reduced blood flow and tissue damage. Unlike other forms of ischemia, it’s typically associated with specific triggers and cellular responses. It’s important to note that the term “ischemia p2” is not a standard medical term. The information presented here is hypothetical and serves as an example of how a new subtype might be described.
Types of Ischemia p2
This section details the hypothetical types of ischemia p2. While the exact types might vary based on the specific context, this hypothetical classification highlights potential distinctions in the underlying mechanisms.
| Type | Characteristics | Pathophysiology |
|---|---|---|
| Type 1: Vasospastic Ischemia p2 | Characterized by sudden, transient vasoconstriction in the affected vascular bed. This leads to a localized, acute reduction in blood flow, often triggered by environmental factors. Tissue damage may be reversible with restoration of blood flow. | This type of ischemia p2 is believed to be initiated by abnormal activation of vascular smooth muscle cells, resulting in vasoconstriction. The process is potentially mediated by the release of vasoconstricting neurotransmitters or inflammatory mediators. |
| Type 2: Thrombotic Ischemia p2 | Involves the formation of a thrombus (blood clot) within the vessel supplying the affected tissue. The thrombus blocks blood flow, leading to progressive tissue damage. The duration and extent of the blockage are key factors in determining the severity of the ischemic event. | The pathophysiology of this type centers on the formation of a thrombus within the artery. This may result from various factors, such as endothelial dysfunction, hypercoagulability, or turbulent blood flow. The resulting blockage prevents oxygen and nutrient delivery to the tissue, leading to ischemia. |
Pathophysiological Mechanisms of Ischemia p2
The underlying mechanisms of ischemia p2, as illustrated in the table, vary based on the specific subtype. However, a common thread involves a disruption in the normal supply of oxygen and nutrients to the affected tissue. This deprivation triggers cellular stress responses, potentially leading to cellular damage and dysfunction. The severity of tissue damage depends on the duration and extent of the ischemia.
Causes of Ischemia p2
Ischemia, a reduction in blood flow to tissues, can have various underlying causes. Understanding these causes is crucial for effective diagnosis and treatment. This section delves deeper into the factors that contribute to ischemic events, exploring the interplay between different risk factors and triggers.Ischemia is not a single disease but a symptom of an underlying condition. Identifying the specific cause is vital for tailored interventions and preventative measures.
Ischemia P2, a significant factor in foot health, essentially refers to reduced blood flow to the foot. Understanding the intricate workings of the foot, like its bones, muscles, and blood vessels, is key to comprehending this condition. Deeply exploring foot anatomy and physiology, like the foot anatomy and physiology , helps us grasp the intricate network that can be compromised in ischemia P2, highlighting the importance of maintaining healthy blood circulation to the feet.
This section provides a comprehensive overview of the primary causes, risk factors, and triggers, enabling a better understanding of this complex physiological process.
Primary Causes of Ischemia
Ischemia stems from a disruption in the delivery of oxygenated blood to tissues. This disruption can arise from a multitude of factors, including vascular obstructions and reduced cardiac output. Atherosclerosis, a buildup of plaque in the arteries, is a significant contributor, narrowing the arterial lumen and impeding blood flow. Other causes encompass conditions like vasculitis, where inflammation damages blood vessels, and emboli, which are blood clots or other foreign matter that travel through the circulatory system and lodge in smaller vessels.
Risk Factors Associated with Ischemia
Several modifiable and non-modifiable risk factors increase the likelihood of developing ischemia. Modifiable risk factors include lifestyle choices like smoking, a sedentary lifestyle, and a diet high in saturated fats. These factors contribute to conditions such as atherosclerosis, a primary cause of ischemia. Non-modifiable factors, such as age and genetics, also play a role. Older individuals are at higher risk due to age-related changes in the vascular system, and a family history of cardiovascular disease can predispose individuals to ischemia.
Common Triggers Leading to Ischemia
Various factors can trigger an ischemic event, exacerbating pre-existing conditions or causing acute episodes. Sudden increases in physical activity, especially in individuals with underlying cardiovascular issues, can lead to increased demand for oxygenated blood, surpassing the capacity of the compromised vascular system. Emotional stress, through its effect on blood pressure and heart rate, can also trigger an ischemic event.
Exposure to extreme temperatures, dehydration, and certain medications can also contribute to ischemic episodes.
Interplay of Contributing Factors, What is ischemia p2
The interplay between different causes, risk factors, and triggers of ischemia is complex. For example, a patient with a history of smoking and high blood pressure (risk factors) might experience an ischemic event (trigger) after strenuous exercise, due to the combined effect of plaque buildup in the arteries and increased blood pressure and heart rate. Understanding this complex interplay is crucial for developing targeted preventative and treatment strategies.
Categorization of Causes, Risk Factors, and Triggers
| Category | Cause/Risk Factor/Trigger | Explanation |
|---|---|---|
| Vascular Obstruction | Atherosclerosis | A buildup of plaque in the arteries, narrowing the arterial lumen and impeding blood flow. |
| Vascular Obstruction | Thrombosis | Formation of a blood clot within a blood vessel, obstructing blood flow. |
| Vascular Obstruction | Emboli | Blood clots or other foreign matter traveling through the circulatory system and lodging in smaller vessels. |
| Reduced Cardiac Output | Heart Failure | Inability of the heart to pump sufficient blood to meet the body’s needs, leading to reduced blood flow. |
| Risk Factors | Smoking | Damages blood vessels and promotes atherosclerosis. |
| Risk Factors | High Blood Pressure | Increases the strain on blood vessels, potentially leading to damage and plaque buildup. |
| Risk Factors | High Cholesterol | Contributes to the formation of plaque in the arteries. |
| Triggers | Strenuous Exercise | Increased demand for oxygenated blood can exceed the capacity of compromised vessels. |
| Triggers | Emotional Stress | Elevates blood pressure and heart rate, potentially triggering an ischemic event. |
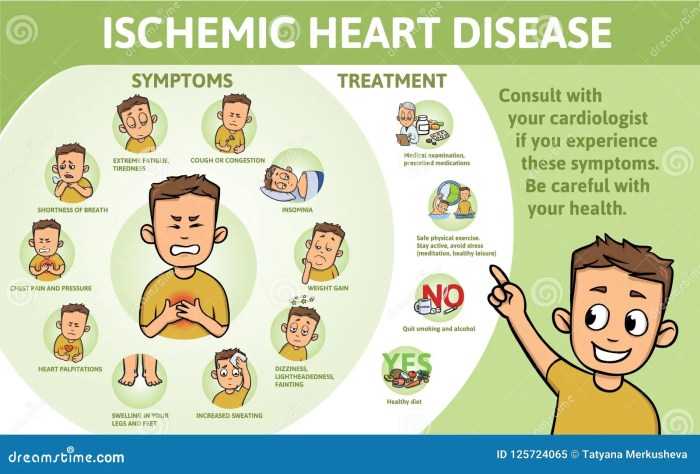
Symptoms of Ischemia p2
Ischemia, a reduction in blood flow to tissues, can manifest in a variety of ways depending on the affected area and the severity of the blockage. Understanding these symptoms is crucial for prompt diagnosis and treatment. Early recognition can significantly improve outcomes.Recognizing the symptoms of ischemia is critical. The specific symptoms experienced will vary depending on the location and extent of the reduced blood flow.
This variation in presentation can sometimes make diagnosis challenging, but awareness of potential differences is key. Comparing these symptoms to those of other conditions can assist in differential diagnosis.
Common Symptoms
A range of symptoms can arise due to ischemia, encompassing pain, numbness, and changes in skin color and temperature. These sensations often stem from the body’s attempt to signal the reduced blood supply.
- Pain: Aching, throbbing, or sharp pain is a common symptom, often described as cramping or burning. The location and intensity of the pain can vary. For example, angina, a type of chest pain, is a common symptom of myocardial ischemia (ischemia of the heart muscle). The pain may radiate to other areas, such as the jaw or arm.
The pain may also be intermittent, coming and going, or constant.
- Numbness and Tingling: A lack of sensation or a tingling feeling in the affected area is another frequent symptom. This can manifest as a loss of feeling, a pins-and-needles sensation, or a prickling feeling. For example, peripheral artery disease can cause numbness and tingling in the feet and legs.
- Changes in Skin Color and Temperature: The skin in the affected area might appear pale, bluish, or even reddish, depending on the underlying cause of the ischemia. The skin temperature may also feel unusually cool or cold to the touch.
- Weakness or Fatigue: Muscles supplied by the affected blood vessels may experience weakness or fatigue, especially with exertion. For instance, a patient with intermittent claudication might experience leg weakness when walking.
Variations in Symptom Presentation
The presentation of symptoms can differ significantly based on the location and severity of the ischemia. For example, ischemic stroke symptoms can range from mild weakness to complete paralysis, while peripheral artery disease symptoms might include pain only during exercise (intermittent claudication) or more constant pain.
Comparison with Other Conditions
It’s essential to differentiate ischemia from other conditions with similar symptoms. For instance, muscle cramps or nerve pain can mimic some ischemic symptoms. A thorough medical history and physical examination are crucial to distinguish between these conditions.
Table of Symptoms, Severity, and Potential Complications
| Symptom | Severity | Possible Complications |
|---|---|---|
| Pain (e.g., angina, intermittent claudication) | Mild to Severe | Myocardial infarction (heart attack), stroke, tissue damage, amputation |
| Numbness and tingling | Mild to Moderate | Nerve damage, tissue damage, loss of function |
| Skin color/temperature changes | Mild to Severe | Tissue damage, ulceration, gangrene |
| Weakness/fatigue | Mild to Severe | Reduced mobility, difficulty with daily tasks, secondary complications |
Diagnosis of Ischemia p2
Uncovering the cause of ischemia requires a multi-faceted approach. A thorough understanding of the patient’s medical history, symptoms, and physical examination findings is crucial. The diagnostic journey often involves a combination of imaging techniques, laboratory tests, and potentially invasive procedures. This section delves into the key diagnostic methods employed in identifying and characterizing ischemia.Accurate diagnosis of ischemia hinges on a meticulous evaluation.
The interplay of various diagnostic tools allows clinicians to pinpoint the affected area, the extent of damage, and the underlying cause. This detailed approach significantly impacts treatment planning and patient outcomes.
Imaging Techniques in Ischemia Diagnosis
Imaging plays a pivotal role in identifying the location and extent of ischemic damage. Different imaging modalities offer varying levels of detail and information. These techniques are often used in combination to gain a comprehensive picture of the affected area.
Ischemia P2, a condition affecting blood flow, can sometimes lead to skin changes. For example, darkening of the skin, like hyperpigmentation on the buttocks, can occur. Learning more about treating hyperpigmentation on the buttocks is key, and you can find helpful advice on that here. Ultimately, understanding ischemia P2 requires a deeper look at the root causes and potential treatments.
- Computed Tomography (CT) Angiography: CT angiography utilizes X-rays and computer processing to visualize blood vessels. This technique is particularly valuable in identifying blockages or narrowing in arteries, which are common causes of ischemia. CT angiography provides detailed images of the arterial system, allowing for the precise localization of the stenosis or occlusion. For example, a patient presenting with chest pain might undergo CT angiography to assess for coronary artery disease, a leading cause of myocardial ischemia.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of soft tissues, including muscles, nerves, and blood vessels. MRI is especially useful in evaluating the extent of ischemic damage to tissues, helping determine the degree of tissue injury. It can differentiate between ischemic and healthy tissue, crucial for determining the prognosis and guiding treatment. A patient with suspected stroke might undergo MRI to evaluate the affected brain region and determine the extent of the infarction.
- Ultrasound: Ultrasound uses sound waves to create images of internal structures. It’s commonly used to evaluate peripheral arteries, like those in the legs, for blockages. Ultrasound is a non-invasive, readily available method, making it suitable for initial screening. A patient experiencing intermittent claudication, pain in the legs during exercise, might undergo ultrasound to assess for peripheral artery disease.
Ischemia P2, a type of blood flow restriction, can be a tricky issue, especially as we age. Understanding the factors that affect blood flow is crucial, and that includes considering things like the prevalence of conditions like menopause. Recent research has shown a correlation between reduced estrogen levels during menopause and the risk of ischemia P2. For more on the fascinating facts and statistics surrounding menopause, check out this insightful article on menopause facts and statistics.
Ultimately, understanding the interconnectedness of these factors helps us better grasp the complexities of ischemia P2.
Laboratory Tests in Ischemia Diagnosis
Laboratory tests provide valuable information about the patient’s overall health and the presence of specific markers associated with ischemia. These tests complement imaging findings and help determine the severity and potential cause of the condition.
- Blood Tests: Blood tests, including complete blood counts (CBCs), lipid profiles, and coagulation studies, can provide crucial information about the patient’s risk factors for ischemia. Elevated cholesterol levels, for instance, may indicate an increased risk of atherosclerosis, a significant cause of ischemic heart disease. A blood clot may be suspected when coagulation factors are abnormal.
- Cardiac Enzymes: In cases of myocardial ischemia, cardiac enzymes, such as creatine kinase-MB (CK-MB) and troponin, are released into the bloodstream. Elevated levels of these enzymes indicate damage to the heart muscle. Cardiac enzymes are critical in diagnosing and assessing the severity of a heart attack. The level and duration of the elevation often guide the severity of the myocardial damage.
Combined Diagnostic Approach
A comprehensive diagnostic approach involves the strategic combination of imaging and laboratory tests. This integrated approach allows for a more accurate and thorough evaluation of the patient.
| Diagnostic Tool | Role in Diagnosis |
|---|---|
| Imaging (CT angiography, MRI) | Identifies location and extent of vascular obstruction or tissue damage. |
| Laboratory tests (blood tests, cardiac enzymes) | Assesses risk factors, identifies markers of tissue damage, and provides information about the patient’s overall health. |
A flowchart demonstrating the diagnostic process would typically begin with a patient’s presentation of symptoms and medical history. This leads to a selection of appropriate imaging tests and laboratory analyses. The combined results guide further evaluation and eventually lead to a definitive diagnosis.
Treatment Options for Ischemia p2
Ischemia, a condition characterized by reduced blood flow to tissues, necessitates prompt and effective treatment to mitigate tissue damage and prevent long-term complications. Various treatment options are available, ranging from lifestyle modifications to invasive procedures. Understanding the nuances of each approach is crucial for tailoring the most appropriate intervention to individual patient needs.Treatment strategies for ischemia are multifaceted, aiming to restore blood flow, manage underlying causes, and alleviate symptoms.
The efficacy of each method depends on the specific type of ischemia, its severity, and the overall health of the patient. Success often hinges on early diagnosis and prompt initiation of appropriate therapy.
Pharmacological Treatments
Pharmacological interventions play a significant role in managing ischemia. Medications can help improve blood flow, reduce blood clotting, and address underlying conditions contributing to the reduced blood supply. For instance, anticoagulants, such as warfarin or heparin, can prevent blood clots, a common cause of ischemia. Antiplatelet agents, like aspirin, can inhibit platelet aggregation, reducing the risk of clot formation.
Other medications might target specific underlying conditions, such as high blood pressure or high cholesterol, which can exacerbate ischemia.
Surgical Interventions
Surgical approaches are often necessary when pharmacological interventions prove insufficient or when the cause of ischemia requires direct intervention. Surgical procedures vary depending on the specific location and cause of ischemia. For instance, angioplasty, a minimally invasive procedure, involves widening narrowed arteries using a balloon catheter, restoring blood flow. Bypass surgery can create alternative pathways for blood to reach the affected area, bypassing blocked or damaged vessels.
These procedures can significantly improve blood flow and reduce the risk of further tissue damage. However, they carry a risk of complications, such as bleeding, infection, and blood clots.
Lifestyle Modifications
Lifestyle changes are crucial in preventing and managing ischemia. A healthy diet rich in fruits, vegetables, and whole grains, coupled with regular exercise, can significantly reduce the risk of developing ischemia-causing conditions like atherosclerosis. Maintaining a healthy weight, controlling blood pressure, and managing blood sugar levels are equally important. Smoking cessation is also essential, as smoking damages blood vessels and increases the risk of blood clots.
These lifestyle modifications can have a profound impact on long-term outcomes, significantly reducing the risk of future ischemic events.
Treatment Comparison Table
| Treatment Method | Effectiveness | Potential Side Effects |
|---|---|---|
| Pharmacological (e.g., anticoagulants, antiplatelets) | Generally effective in preventing clot formation and improving blood flow, especially when underlying conditions are managed. | Bleeding, allergic reactions, and interactions with other medications are potential side effects. The effectiveness can vary depending on the specific medication and the patient’s condition. |
| Surgical (e.g., angioplasty, bypass surgery) | Can be highly effective in restoring blood flow and improving outcomes, particularly for severe or localized blockages. | Bleeding, infection, blood clots, stroke, and nerve damage are potential risks, especially with more invasive procedures. |
| Lifestyle Modifications (e.g., diet, exercise, weight management) | Profoundly effective in preventing ischemia and improving overall cardiovascular health. These interventions often have the lowest risk of side effects. | Requires commitment and sustained effort. Some individuals may experience temporary discomfort or challenges adjusting to new habits. |
Prognosis and Management of Ischemia p2: What Is Ischemia P2
Ischemia, a reduced blood flow to tissues, can have significant implications for a patient’s overall health and well-being. Understanding the prognosis and effective management strategies is crucial for improving patient outcomes. This section delves into the expected course of ischemia p2, highlighting factors that influence the prognosis, and outlining strategies for managing the condition, including preventative measures and long-term management plans.Prognosis for ischemia p2 varies considerably based on the underlying cause, the severity of the ischemia, and the promptness and effectiveness of treatment.
While some patients experience a full recovery with minimal long-term effects, others may face more serious complications. Factors like the patient’s overall health, age, and pre-existing conditions play a significant role in determining the specific prognosis for each individual.
Factors Influencing Prognosis
The prognosis of ischemia p2 is multifaceted and influenced by several interconnected factors. These include the cause of the ischemia, the extent of tissue damage, the timeliness of diagnosis and treatment, and the patient’s overall health status. For instance, if the ischemia is caused by a blood clot that is promptly treated, the prognosis is generally better than if the clot remains untreated for an extended period.
Strategies for Managing Ischemia p2
Effective management of ischemia p2 necessitates a multi-pronged approach encompassing both acute and long-term strategies. A crucial aspect of management involves identifying and addressing the underlying cause of the ischemia. This may involve lifestyle modifications, medical interventions, or a combination of both.
Preventive Measures
Preventive measures play a vital role in minimizing the risk of ischemia p2 and its associated complications. A healthy lifestyle, including a balanced diet, regular exercise, and maintaining a healthy weight, is paramount. Quitting smoking and controlling underlying conditions like diabetes and high blood pressure are also critical preventative measures. Regular check-ups and screenings can help detect potential issues early, allowing for prompt intervention and minimizing the risk of developing ischemia p2.
Long-Term Management Plans
Long-term management of ischemia p2 involves ongoing monitoring and proactive strategies to prevent future episodes. This may include medication to regulate blood pressure or cholesterol levels, lifestyle modifications, and regular follow-up appointments with healthcare providers. Specific long-term management plans are tailored to the individual patient’s needs and the underlying cause of the ischemia. For example, a patient with ischemia due to atherosclerosis might require a combination of medications, dietary changes, and exercise routines to manage their condition effectively.
Conclusion
In conclusion, ischemia p2 presents a complex medical challenge requiring a multifaceted understanding. From its definition and characteristics to its causes, symptoms, diagnosis, and treatment, this exploration provides a comprehensive overview. Ultimately, recognizing the factors influencing the prognosis and developing effective management strategies are key to improving the lives of those affected. Further research and clinical trials are essential for advancing our understanding and treatment options for ischemia p2.




