What is an urachal remnant? This in-depth look explores the often-overlooked urachal remnant, a fascinating but sometimes complex aspect of human embryology. We’ll delve into its development, different types, clinical presentations, diagnostic methods, and management options, providing a comprehensive overview of this intriguing medical condition.
From its initial formation during fetal development to its potential impact on a person’s health later in life, understanding the urachal remnant is crucial. This guide clarifies the intricate relationship between the urachus, the remnant, and related conditions, equipping readers with a deeper understanding of this medical entity.
Definition and Anatomy
An urachal remnant is a persistent portion of the urachus, a fetal structure connecting the bladder to the umbilical cord. Normally, the urachus closes and disappears during fetal development, but sometimes remnants of this structure remain. These remnants can vary significantly in size and location, leading to a range of potential clinical presentations. Understanding the normal development of the urachus and the anatomical variations is crucial for accurate diagnosis and appropriate management.The urachus plays a vital role in fetal development.
During gestation, it serves as a pathway for urine to drain from the developing bladder to the amniotic fluid surrounding the fetus. As the fetus matures and the urinary system develops fully, the urachus progressively atrophies and closes, typically by the time of birth. This closure marks the transition from fetal to postnatal urinary function. Failure of complete regression results in an urachal remnant.
Normal Embryological Development of the Urachus
The urachus begins its development early in fetal life. It arises from the apex of the bladder and extends towards the umbilicus, where it is connected to the umbilical cord. This connection is crucial for the excretion of fetal urine into the amniotic fluid. As the fetal urinary system matures, the urachus gradually loses its function and begins to regress, typically by the time of birth.
The process of regression involves the progressive closure and obliteration of the urachal tissue.
Anatomical Location of the Urachus
The urachus is located within the abdominal cavity, extending from the apex of the bladder to the umbilicus. It is positioned anterior to the bladder and the umbilical arteries, passing through the extraperitoneal tissue. Its proximity to various abdominal structures, such as the bladder, ureters, and intestines, is important to consider in the context of potential complications or diagnostic considerations.
Careful consideration of its relation to other structures is vital in surgical planning and interpretation of imaging studies.
Comparison of Normal Urachus and Urachal Remnant
| Feature | Normal Urachus | Urachal Remnant |
|---|---|---|
| Structure | A tubular structure connecting the bladder apex to the umbilicus, typically obliterated by birth. | A persistent portion of the urachus, ranging from a fibrous cord to a cyst or diverticulum. |
| Function | Drains fetal urine to the amniotic fluid. | Generally non-functional, but may cause complications like infection, bleeding, or obstruction. |
| Size | Typically regresses completely. | Can vary in size, from a few millimeters to several centimeters. |
| Clinical Significance | Normal and expected developmental process. | May present with symptoms like pain, palpable mass, or urinary tract infections. |
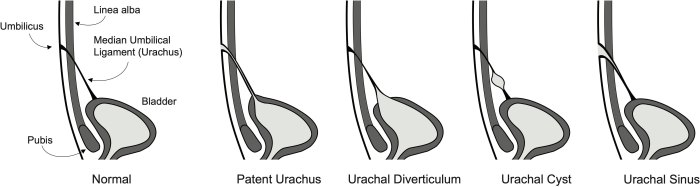
Types of Urachal Remnants
The urachus, a fetal structure connecting the bladder to the umbilical cord, normally closes after birth. However, various remnants of this structure can persist, leading to a range of clinical presentations. Understanding the different types and their characteristics is crucial for accurate diagnosis and appropriate management. These remnants can vary significantly in their size, shape, and location, impacting the potential complications.
Classification Systems for Urachal Remnants
Various classification systems exist to categorize urachal remnants. These systems often consider the extent of the remnant’s connection to the bladder and the presence or absence of associated anomalies. The most common classification systems are based on the anatomical continuity of the remnant and the presence of a patent channel. A patent channel indicates an open pathway, whereas a closed remnant indicates a closed pathway.
Understanding the specific characteristics of each type aids in predicting potential complications.
So, what exactly is an urachal remnant? It’s basically a leftover bit of tissue from when we were developing in the womb. Think about how much your body changes after significant weight loss, and how that can sometimes leave you with extra skin. Fortunately, there are ways to address this, like the techniques discussed in this helpful article on how to tighten skin after weight loss.
Understanding the process of weight loss and the resulting changes to your skin is crucial to understanding how to best address an urachal remnant. It’s all part of the amazing and sometimes complicated process of human development and health.
Types and Clinical Significance
Urachal remnants can be categorized into several types, each with varying clinical implications. These categories typically involve different degrees of structural continuity between the bladder and the remnant. The extent of the remnant and its associated features determine the potential for complications. These complications range from asymptomatic findings to potentially life-threatening conditions.
Table of Urachal Remnants
| Type | Features | Clinical Significance/Risk Factors |
|---|---|---|
| Patent Urachus | A completely open connection between the bladder and the umbilicus. This is characterized by persistent drainage of urine from the umbilicus. | High risk of recurrent urinary tract infections (UTIs), urinary leakage, and potential complications from infection and inflammation. Often diagnosed in infancy or childhood. |
| Urachal Sinus | A blind-ending tract that opens into the umbilicus. It doesn’t drain urine directly but can be a site for infection. | Lower risk than a patent urachus, but still predisposes to UTIs and local inflammation. Symptoms can vary and may not be present in early stages. |
| Urachal Cyst | A fluid-filled sac formed by a portion of the urachus. The cyst can vary in size and location. | Symptoms may include abdominal pain, mass, or complications from infection. The cyst may grow slowly, but if it ruptures, it can lead to complications. Symptoms are often related to the size and location of the cyst. |
| Urachal Diverticulum | A pouch-like protrusion from the urachus, often located near the bladder. The diverticulum may not always cause symptoms. | Generally associated with a lower risk of complications compared to other types. It might be incidentally detected during imaging studies for unrelated reasons. |
| Closed Urachal Remnant | A remnant of the urachus that is completely closed. This is often asymptomatic. | Rarely presents any clinical significance; however, it can be found incidentally during imaging studies for other conditions. |
Clinical Presentation
Urachal remnants, though often asymptomatic, can manifest in a variety of ways. The clinical presentation depends significantly on the type of remnant and the presence of any associated complications. Understanding these presentations is crucial for accurate diagnosis and appropriate management. Recognizing the symptoms, their potential severity, and their correlation with specific types of remnants aids in guiding the diagnostic process.
Common Clinical Presentations
Urachal remnants can present with a range of symptoms, often mimicking other urinary tract or abdominal conditions. These presentations can vary widely depending on the specific type of remnant, the degree of obstruction, and the presence of infection. Symptoms can appear at any age, from infancy to adulthood. The most common clinical presentations include:
- Abdominal mass: A palpable mass in the lower abdomen, particularly in the midline, is a frequently encountered finding. This mass can vary in size and consistency, depending on the extent of the remnant and the presence of any associated fluid collections.
- Pain: Pain in the lower abdomen is another common presentation, ranging from mild discomfort to severe cramping. The location and intensity of the pain may vary based on the type of remnant and any associated infection or inflammation.
- Urinary tract symptoms: Symptoms such as dysuria (painful urination), frequency, or urgency can be present. These symptoms can be indicative of urinary tract infections, but can also arise from urachal remnants that are obstructing the flow of urine.
- Voiding abnormalities: Incomplete emptying of the bladder or abnormal voiding patterns, such as dribbling or straining, may be present. These are often linked to the obstruction of the urinary tract by the urachal remnant.
Symptoms Associated with Specific Types
The symptoms associated with a particular type of urachal remnant can offer clues for diagnosis. A patent urachus, for example, might present with a continuous flow of urine or discharge from the umbilicus. In contrast, a non-patent urachus that has become obstructed might manifest with a cystic mass or an abscess.
- Patent urachus: This type is often associated with a persistent umbilical discharge or a palpable mass. The discharge may be clear, cloudy, or contain blood. This persistent discharge can cause significant discomfort and potentially lead to infections. The mass may be associated with bladder-like distention. It’s worth noting that a patent urachus can present with minimal symptoms.
- Urachal cyst: Patients with a urachal cyst often present with a palpable mass in the lower abdomen. The mass may be tender to palpation and associated with mild pain or discomfort. The cyst may become infected, leading to increased pain and tenderness.
- Urachal sinus: A urachal sinus is characterized by a tract or fistula that connects the umbilicus to the bladder. Symptoms can include intermittent or persistent leakage of urine from the umbilicus, sometimes with an unpleasant odor, indicating potential infection. These symptoms can also be associated with recurrent urinary tract infections.
Potential Complications
Urachal remnants can lead to various complications. These complications can range from mild discomfort to severe conditions requiring surgical intervention. The severity of the complication often depends on the type of remnant, the presence of infection, and the timely intervention.
- Infection: Urachal remnants can become infected, leading to inflammation and pain. Infection may be localized or spread to surrounding tissues.
- Obstruction: Urachal remnants can obstruct the flow of urine, leading to bladder distension and potentially kidney damage.
- Bleeding: In some cases, urachal remnants may be associated with bleeding. This can manifest as hematuria or bleeding from the umbilicus.
- Abscess formation: Infection of the urachal remnant can lead to the formation of an abscess, which requires surgical drainage.
Symptom Correlation Table
| Symptom | Potential Correlation with Type ||——————-|————————————|| Abdominal mass | Patent urachus, urachal cyst, urachal sinus || Pain | Urachal cyst, urachal sinus, infection || Urinary symptoms | Patent urachus, urachal sinus, obstruction || Voiding abnormalities | Patent urachus, obstruction || Umbilical discharge | Patent urachus, urachal sinus |
Diagnostic Methods: What Is An Urachal Remnant
Unraveling the mystery of a urachal remnant often requires a meticulous diagnostic approach. Identifying the presence and nature of the remnant is crucial for proper treatment planning. A combination of imaging techniques provides valuable insights, allowing clinicians to assess the location, size, and potential complications of the remnant. Different imaging modalities offer varying degrees of resolution and information, necessitating careful consideration of each method’s strengths and weaknesses.
Imaging Techniques for Urachal Remnants, What is an urachal remnant
Various imaging techniques play a pivotal role in diagnosing urachal remnants. These methods provide critical anatomical information, helping to differentiate between a benign urachal remnant and other conditions that might mimic its presentation. Understanding the strengths and weaknesses of each technique is essential for accurate diagnosis.
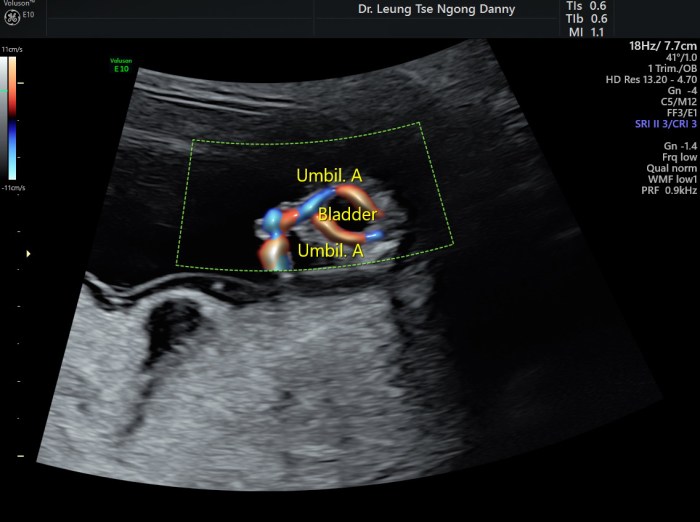
Ultrasound
Ultrasound is a valuable initial imaging modality for assessing urachal remnants. Its non-invasive nature and readily available technology make it a cost-effective and accessible option. Real-time imaging allows for dynamic assessment of the structure, enabling visualization of the remnant’s location, size, and any associated abnormalities.
Ultrasound’s primary advantage lies in its ability to distinguish between fluid collections and solid masses, aiding in differentiating urachal remnants from other potential pathologies.
However, ultrasound’s resolution can be limited, especially in cases where the remnant is small or obscured by surrounding structures. Interpreting the findings requires experience and expertise to avoid misdiagnosis.
Computed Tomography (CT)
CT scans offer higher resolution and detailed cross-sectional views of the abdomen and pelvis, which can be particularly useful in identifying the complex anatomy of urachal remnants. Multiplanar reconstructions provide a comprehensive view of the remnant’s position and relationship to surrounding structures, enhancing diagnostic accuracy.
CT scans utilize ionizing radiation, which presents a potential risk of radiation exposure, and are generally more expensive than ultrasound.
The ability to visualize calcifications within the remnant, if present, is a significant advantage of CT. This can be particularly useful in differentiating urachal remnants from other similar conditions.
Magnetic Resonance Imaging (MRI)
MRI provides excellent soft tissue contrast, which is crucial for evaluating the complex anatomy of urachal remnants. It allows for precise visualization of the remnant’s morphology and its relationship to surrounding organs.
MRI is advantageous because it does not use ionizing radiation, making it a safer alternative for repeated examinations or examinations of patients with concerns about radiation exposure.
While MRI provides exceptional soft tissue contrast, it can be more time-consuming and expensive compared to ultrasound and CT. The presence of metal implants or artifacts can sometimes hinder the quality of the images.
Table: Diagnostic Imaging Methods for Urachal Remnants
| Imaging Method | Resolution | Typical Applications |
|---|---|---|
| Ultrasound | Moderate | Initial assessment, evaluating fluid collections, guiding biopsies |
| CT | High | Detailed anatomical assessment, evaluating calcifications, identifying complex anatomy |
| MRI | Excellent | Detailed soft tissue visualization, assessing complex anatomy, evaluating complications |
Management and Treatment
Urachal remnants, though often asymptomatic, can necessitate intervention when complications arise. Management strategies for urachal remnants prioritize addressing the specific issue, ranging from watchful waiting to surgical intervention. The choice of management approach is crucial and hinges on factors like the patient’s age, the extent of the remnant, and the presence of symptoms. Prompt and appropriate management is essential to prevent potential complications and ensure favorable outcomes.Surgical intervention is often the preferred approach for managing symptomatic or complicated urachal remnants.
The aim of surgical treatment is to remove the remnant completely, thereby minimizing the risk of recurrence and complications like infection, fistula formation, or malignancy. Different surgical techniques are employed based on the specific characteristics of the remnant and the surgeon’s expertise.
Surgical Approaches
Surgical removal of urachal remnants is a common procedure. Open surgery, laparoscopy, and minimally invasive techniques are the most frequently used approaches. The selection of the surgical technique depends on various factors, including the location and size of the remnant, the patient’s overall health, and the surgeon’s preference. Open surgery is generally reserved for larger remnants or when there is a significant risk of complications during a minimally invasive procedure.
Surgical Techniques and Recovery Times
Various surgical techniques are used to address urachal remnants, each with its own set of advantages and disadvantages. The recovery time and potential risks vary depending on the chosen approach.
- Open Surgery: This involves a larger incision in the abdomen, providing direct access to the urachal remnant. The recovery period is typically longer, often lasting several weeks. Potential complications include infection, bleeding, and wound healing issues. This method is generally more invasive but allows for complete removal of the remnant and addressing associated abnormalities.
- Laparoscopic Surgery: This minimally invasive technique utilizes small incisions and specialized instruments to remove the remnant. Recovery is generally faster than open surgery, with patients often returning to normal activities within a few weeks. Potential complications include bleeding, infection, and damage to surrounding structures. Laparoscopy is a valuable option for smaller remnants and patients with comorbidities.
- Robotic Surgery: This advanced technique utilizes robotic arms controlled by a surgeon to perform the procedure. It provides enhanced precision and dexterity, potentially leading to a more precise removal of the remnant. Recovery times are similar to those of laparoscopic surgery, with potential risks also comparable. Robotic surgery is a good choice for complex cases requiring meticulous precision.
Potential Complications
Surgical interventions for urachal remnants, while generally safe, carry the risk of complications. These can range from minor issues like infection or bleeding to more serious complications such as bowel or bladder injury. Careful surgical planning and meticulous execution are crucial to minimize these risks.
Table of Surgical Procedures
| Surgical Procedure | Technique | Recovery Time (approx.) | Potential Risks |
|---|---|---|---|
| Open Surgery | Large abdominal incision to directly access and remove the remnant. | 4-6 weeks | Infection, bleeding, wound complications, bowel/bladder injury |
| Laparoscopic Surgery | Small incisions, specialized instruments, and a camera to visualize and remove the remnant. | 2-4 weeks | Bleeding, infection, injury to surrounding structures, conversion to open surgery |
| Robotic Surgery | Robotic arms controlled by a surgeon provide enhanced precision. | 2-4 weeks | Bleeding, infection, injury to surrounding structures, conversion to open surgery |
Associated Conditions
Urachal remnants, while often benign, can sometimes be linked to other congenital anomalies. Understanding these associations is crucial for accurate diagnosis and appropriate management, as the presence of a urachal remnant might influence the evaluation and treatment of the associated condition. These co-occurrences can present diagnostic challenges, demanding a thorough approach to assess the entire spectrum of potential abnormalities.
Potential Associations with Other Congenital Anomalies
Urachal remnants are frequently encountered alongside other developmental defects. These can range from minor to more significant conditions. The presence of a urachal remnant may not directly cause these other anomalies, but their co-existence highlights the complex interplay of factors influencing embryonic development. For example, a urachal remnant might be present in a patient with a urinary tract malformation, suggesting a possible shared developmental origin.
Risk Factors for Co-occurrence
Identifying risk factors for the co-occurrence of urachal remnants and other congenital anomalies is a complex area of research. While a definitive cause-and-effect relationship isn’t always established, certain factors might increase the probability of such co-occurrences. Genetic predisposition plays a role in many congenital conditions, and the presence of a family history of both urachal anomalies and other congenital malformations warrants a heightened level of suspicion and comprehensive evaluation.
So, what exactly is an urachal remnant? Basically, it’s a leftover bit of tissue from our fetal development. It’s important to understand that the digestive system, while fascinating, isn’t directly involved in this particular anatomical leftover. To truly grasp the complexities of our internal systems, you should definitely check out tour the digestive system for a comprehensive look at how our bodies break down food.
Ultimately, understanding urachal remnants helps us appreciate the intricate processes that shape our bodies from the very beginning.
Environmental factors, such as maternal exposure to certain teratogens during pregnancy, could also contribute. It’s important to note that these are potential factors, and further research is needed to confirm their significance.
Diagnostic Challenges
The presence of a urachal remnant complicates the diagnosis of other congenital anomalies. The clinical presentation of a urachal remnant might mask or mimic the signs and symptoms of the associated condition. For instance, a child with a urachal fistula and a concurrent kidney malformation might present with similar urinary symptoms, making it difficult to pinpoint the specific cause.
This diagnostic complexity necessitates a multidisciplinary approach, involving collaboration between specialists like pediatric urologists, radiologists, and geneticists. Advanced imaging techniques, such as ultrasound, CT scans, and MRI, are often crucial for accurate delineation of both the urachal remnant and any associated anomalies. Careful analysis of the imaging findings, coupled with the patient’s medical history, is essential for a conclusive diagnosis.
Prevalence and Association Table
| Population Group | Prevalence of Urachal Remnants | Potential Associated Congenital Abnormalities |
|---|---|---|
| Caucasian | Estimated at 1 in 10,000 live births | Urinary tract malformations, vertebral anomalies, cardiac defects |
| Asian | Prevalence data less readily available, but likely similar to Caucasian populations | Urinary tract malformations, limb abnormalities, gastrointestinal issues |
| African | Prevalence data less readily available, but likely similar to Caucasian and Asian populations | Urinary tract malformations, musculoskeletal defects, cardiac defects |
Note: This table provides a general overview. Specific prevalence figures and associations may vary depending on the specific study and population analyzed. Data on prevalence and specific associated anomalies is not readily available in a consistent and comprehensive format across different populations, hence the general statement.
Ever wondered about urachal remnants? Basically, it’s a leftover bit of tissue from your fetal development. It’s not uncommon, and often doesn’t cause any problems, but it’s good to know what to look for. Learning about foot issues like bunionettes, or tailor’s bunions, can help put things in perspective. This article will explain how these bony bumps form and what causes them.
Ultimately, though, urachal remnants are a fascinating reminder of our early development stages.
Prognosis and Long-Term Outcomes
The prognosis for patients with urachal remnants varies significantly, depending on the specific type and extent of the remnant, the presence of complications, and the chosen treatment approach. Understanding the potential long-term outcomes is crucial for informed decision-making, both for patients and healthcare providers. A thorough evaluation of the individual case is essential to accurately predict the long-term impact.The long-term outcomes of urachal remnant management are largely influenced by the success of the treatment in eliminating the potential for complications and preventing recurrence.
Factors such as the completeness of the resection, the patient’s overall health, and the presence of associated anomalies play a crucial role in determining the likelihood of favorable outcomes.
Factors Influencing Long-Term Prognosis
Several factors contribute to the long-term prognosis of patients with urachal remnants. These factors can be categorized into pre-operative, operative, and post-operative factors. Pre-operative factors include the age of the patient, the extent of the urachal remnant, the presence of any associated urinary tract anomalies, and the patient’s general health status. Operative factors include the surgical approach, the completeness of the resection, and the extent of any complications during the procedure.
Post-operative factors include the patient’s compliance with post-operative care, the development of any complications, and the recurrence rate of the remnant.
Long-Term Outcomes of Treatment Options
Different treatment options for urachal remnants can yield varying long-term outcomes. Surgical resection, the most common approach, generally results in a good prognosis when performed completely and correctly. Minimally invasive techniques, like laparoscopic or robotic surgery, are increasingly utilized and show promising outcomes in terms of shorter hospital stays and reduced postoperative pain. However, complete removal of the remnant remains crucial to prevent recurrence.Post-operative complications, such as urinary tract infections or fistula formation, can negatively impact long-term outcomes.
Prompt diagnosis and appropriate management of these complications are essential to prevent long-term complications and improve the patient’s quality of life.
Data Illustrating Long-Term Functional Impact
Comprehensive data on the long-term functional impact of urachal remnants on patients are limited. However, studies consistently demonstrate that complete surgical resection of the remnant, when performed correctly, significantly reduces the risk of long-term complications and recurrence. Follow-up studies of patients who underwent surgical resection often show excellent long-term urinary function and overall health. Patients who experience complications due to incomplete resection or inadequate management of complications often experience recurring issues and reduced quality of life.
Illustrative Cases of Urachal Remnants
Urachal remnants, while often asymptomatic, can sometimes lead to significant health concerns. Understanding the spectrum of presentations, from uncomplicated to complex, is crucial for effective diagnosis and management. The following illustrative cases highlight the diverse clinical manifestations and outcomes associated with urachal remnants.
Case 1: Asymptomatic Urachal Cyst
A 10-year-old boy presented with a palpable, soft, mobile mass in the lower abdomen. Physical examination revealed a small, fluctuant mass near the umbilicus. Imaging studies (ultrasound and CT scan) confirmed the presence of a well-defined, cystic structure communicating with the bladder. The patient remained asymptomatic, with no urinary tract infections or pain. Management involved observation and periodic imaging to monitor the cyst’s size and potential for complications.
The patient’s cyst remained stable over the next 2 years and no further intervention was required.
Case 2: Infected Urachal Sinus
A 2-year-old girl presented with recurrent urinary tract infections (UTIs). Physical examination revealed a small, erythematous sinus opening near the umbilicus. Diagnostic imaging (ultrasound and CT scan) revealed a urachal sinus tract extending from the umbilicus to the bladder. Culture of the sinus discharge confirmed the presence of bacteria, highlighting the potential for infection in these cases.
Management involved surgical excision of the urachal sinus and antibiotics to clear the infection. The patient recovered well and subsequent UTIs were resolved.
Case 3: Urachal Diverticulum with Mass Effect
A 35-year-old woman presented with lower abdominal pain and a progressively enlarging mass near the umbilicus. The patient had a history of recurrent urinary tract infections. Imaging studies (CT scan and MRI) showed a large, complex mass arising from the urachal remnant, extending into the bladder and causing obstruction. The mass compressed the adjacent structures, leading to urinary symptoms.
Surgical resection of the urachal diverticulum with reconstruction of the bladder was performed. Post-operatively, the patient’s symptoms resolved, and urinary function returned to normal.
Summary Table of Illustrative Cases
| Case | Clinical Presentation | Diagnostic Findings | Management | Outcome |
|---|---|---|---|---|
| 1 | Palpable mass, asymptomatic | Well-defined cystic structure, communicating with bladder | Observation, periodic imaging | Stable cyst, no further intervention required |
| 2 | Recurrent UTIs, erythematous sinus | Urachal sinus tract, positive bacterial culture | Surgical excision, antibiotics | Complete resolution of symptoms, no recurrence |
| 3 | Lower abdominal pain, enlarging mass, recurrent UTIs | Large, complex mass, obstruction, mass effect | Surgical resection, bladder reconstruction | Resolution of symptoms, restoration of urinary function |
Prevention and Awareness
Urachal remnants, while often asymptomatic, can lead to significant complications if left undiagnosed. Understanding the factors that might contribute to their development and spreading awareness about this condition can play a vital role in early detection and improved outcomes. This section delves into current knowledge about potential causes and preventive measures, as well as strategies for raising public awareness.The exact causes of urachal remnants remain largely unknown, although certain risk factors may potentially contribute.
Research continues to explore genetic predispositions, environmental influences, and the interplay of various factors that might increase the likelihood of a urachal remnant forming. However, currently, there are no established preventive measures that can definitively reduce the risk of developing a urachal remnant.
Current Understanding of Potential Causes
Research on urachal remnants is ongoing. While the exact causes are not fully understood, potential factors that might contribute to the development of a urachal remnant include, but are not limited to, genetic predispositions, certain environmental exposures during fetal development, and possible interactions between various biological factors. Further research is crucial to fully elucidate the complex mechanisms behind urachal remnant formation.
Strategies for Increasing Public Awareness
Raising public awareness about urachal remnants is essential for early diagnosis and improved outcomes. Medical professionals can play a key role by educating patients and families about the signs, symptoms, and potential complications of this condition. This includes discussing the importance of regular check-ups, particularly in individuals with a family history of urogenital anomalies. Educational materials, including pamphlets and online resources, can also provide valuable information to the general public.
Collaboration with medical organizations and patient advocacy groups can further enhance awareness campaigns.
Current Research Efforts
Researchers are actively investigating the underlying mechanisms behind urachal remnant formation. Studies are focusing on identifying potential genetic markers and environmental factors that may increase the risk of developing this condition. Further exploration into the developmental stages of the urachus and the factors influencing its closure could reveal crucial insights. Improved diagnostic tools and management strategies are also key areas of research to enhance the accuracy of diagnosis and treatment outcomes for patients with urachal remnants.
The goal is to develop more targeted and effective interventions, ultimately improving the lives of those affected.
Final Conclusion
In conclusion, urachal remnants, while often a source of concern, can be effectively managed with appropriate medical intervention. This guide has provided a thorough overview, from the initial stages of development to potential long-term outcomes. By understanding the intricacies of this condition, individuals and healthcare professionals can approach diagnosis, treatment, and prognosis with greater confidence.




