What is an MCH in a blood test? Mean Corpuscular Hemoglobin (MCH) is a crucial blood parameter reflecting the average amount of hemoglobin within a single red blood cell. Understanding MCH levels is vital for assessing red blood cell health and identifying potential underlying health issues. This comprehensive guide delves into the definition, measurement, interpretation, and clinical significance of MCH, highlighting its role in diagnosing and monitoring various conditions.
MCH is closely linked to other blood parameters like Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin Concentration (MCHC). These measurements, when analyzed together, provide a more complete picture of red blood cell characteristics and function. We’ll explore how these parameters work in tandem to paint a clearer picture of a person’s overall health.
Definition and Significance: What Is An Mch In A Blood Test
Mean Corpuscular Hemoglobin (MCH) is a crucial blood test parameter that provides insights into the average amount of hemoglobin within a single red blood cell. Understanding MCH is vital for assessing the overall health and function of red blood cells, which are responsible for carrying oxygen throughout the body. A comprehensive evaluation of MCH often complements other blood tests, such as Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin Concentration (MCHC), to offer a more complete picture of red blood cell characteristics.MCH, in essence, reflects the average weight of hemoglobin contained within a red blood cell.
A healthy MCH value indicates that the red blood cells are producing and maintaining the appropriate levels of hemoglobin, a protein essential for oxygen transport. Variations from the normal range can suggest underlying health issues or deficiencies, and understanding these variations is essential for proper diagnosis and treatment.
Relationship to Other Blood Parameters
MCH is intrinsically linked to other red blood cell indices, such as MCV and MCHC. MCV measures the average volume of red blood cells, while MCHC reflects the concentration of hemoglobin within those cells. Together, these parameters provide a comprehensive picture of red blood cell morphology and function. For example, a low MCV often accompanies a low MCH, suggesting microcytic anemia, where red blood cells are smaller and contain less hemoglobin.
Conversely, a high MCV often corresponds with a high MCH, indicating macrocytic anemia, where red blood cells are larger and contain more hemoglobin.
Significance of Abnormal MCH Values
Abnormal MCH values can indicate various health conditions. A low MCH, often accompanied by a low MCV, suggests a deficiency in iron, which is crucial for hemoglobin production. This can lead to iron deficiency anemia, characterized by insufficient oxygen delivery to the body’s tissues. On the other hand, a high MCH, typically associated with a high MCV, might point to vitamin B12 or folate deficiencies, which are also crucial for red blood cell production.
These deficiencies can lead to macrocytic anemias, where red blood cells are abnormally large. Other conditions, such as thalassemia, can also manifest with abnormal MCH values.
Comparison of Normal, High, and Low MCH Values
| MCH Value | Potential Implications |
|---|---|
| Normal (within the reference range) | Indicates healthy red blood cell function and hemoglobin production. |
| High | May suggest macrocytic anemia due to vitamin B12 or folate deficiencies, or other conditions like liver disease. A high MCH often accompanies a high MCV. Examples include patients with pernicious anemia, where the body cannot absorb vitamin B12. |
| Low | Often signifies microcytic anemia, potentially caused by iron deficiency. This is frequently accompanied by a low MCV. For instance, individuals with a strict vegetarian diet, or those experiencing significant blood loss, are at risk for iron deficiency and consequent low MCH. |
Measurement and Calculation
Determining the Mean Corpuscular Hemoglobin (MCH) in a blood test is crucial for understanding red blood cell function. It reflects the average amount of hemoglobin contained within a single red blood cell. Accurate measurement and calculation are essential for diagnosing various conditions, ranging from anemia to certain types of hemolytic disorders. Precise methodologies ensure reliable results, allowing for appropriate medical interventions.
Process of Measuring MCH
Measuring MCH involves a multi-step process that starts with a complete blood count (CBC). The CBC provides a variety of hematological parameters, including the total red blood cell count (RBC count) and the total hemoglobin (Hb) content in the blood. These two values are then used in the calculation of MCH. Modern automated hematology analyzers perform these measurements with high precision and speed, reducing manual error.
These instruments utilize optical techniques to measure the physical properties of blood cells, enabling precise quantification of hemoglobin within red blood cells.
Formulas for Calculating MCH
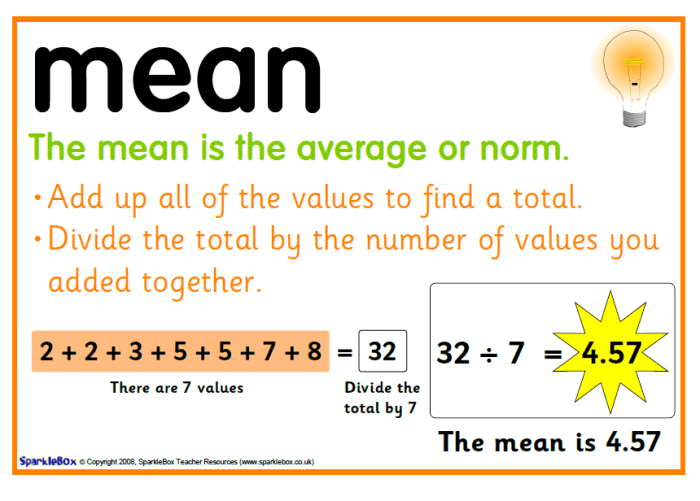
The calculation of MCH relies on a simple formula that relates the total hemoglobin content to the total red blood cell count. The formula is:
MCH = (Total Hemoglobin / Total RBC count) x 10
where:
- MCH represents the Mean Corpuscular Hemoglobin in picograms (pg).
- Total Hemoglobin is measured in grams per deciliter (g/dL).
- Total RBC count is measured in millions per microliter (10 6/µL).
Step-by-Step Procedure for Calculating MCH
- Obtain the results of the complete blood count (CBC) from the blood test. This will provide the values for total hemoglobin and the total red blood cell count.
- Carefully record the numerical values for total hemoglobin and total red blood cell count from the CBC report.
- Substitute the values obtained in step 2 into the formula: MCH = (Total Hemoglobin / Total RBC count) x 10.
- Perform the calculation to determine the MCH value.
- Ensure the correct units are used throughout the calculation to get the MCH in picograms (pg). A critical step is verifying that the units are consistent (e.g., g/dL for hemoglobin and 106/µL for red blood cells).
Comparison of Different Methods
While automated hematology analyzers are the most common and reliable method for measuring MCH, older manual methods, such as spectrophotometry, were previously used. Automated methods offer significantly improved accuracy, precision, and speed compared to manual techniques. They also reduce the potential for human error inherent in manual procedures.
Table Illustrating Calculation of MCH
| Component | Value | Units |
|---|---|---|
| Total Hemoglobin | 15 | g/dL |
| Total RBC count | 5 | 106/µL |
| MCH Calculation | (15 g/dL / 5 106/µL) x 10 | pg |
| MCH Result | 30 | pg |
Interpretation of Results
Understanding your Mean Corpuscular Hemoglobin (MCH) level is crucial for a complete picture of your red blood cell health. It provides insights into the average amount of hemoglobin packed within a single red blood cell. This interpretation, combined with other blood test results, helps healthcare professionals assess potential underlying conditions. Interpreting MCH levels requires considering various factors and potential implications.The MCH result, along with other parameters like Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin Concentration (MCHC), paints a more comprehensive picture of red blood cell characteristics.
These values are intricately linked and help doctors determine if the cells are the appropriate size and contain the right amount of hemoglobin. This interplay is critical in diagnosing various conditions.
Factors Influencing MCH Levels
Several factors can influence MCH levels, affecting the average hemoglobin content per red blood cell. Dietary deficiencies, particularly iron and vitamin B12 deficiencies, can significantly impact hemoglobin production, leading to lower MCH levels. Chronic diseases, such as kidney disease or inflammatory conditions, can also influence MCH levels. Furthermore, certain medications and lifestyle factors can play a role.
Implications of High MCH Levels
High MCH levels, indicating an above-average amount of hemoglobin per red blood cell, can suggest certain conditions. For instance, a high MCH could be linked to conditions characterized by macrocytic anemia, where red blood cells are larger than normal. This might be related to deficiencies in vitamin B12 or folate. Other possible factors include liver disease or certain types of bone marrow disorders.
It’s essential to note that a high MCH value, in isolation, does not definitively diagnose any condition. Further investigations and a complete medical history are necessary for accurate diagnosis.
Implications of Low MCH Levels
Conversely, low MCH levels suggest that the average amount of hemoglobin within each red blood cell is lower than normal. This is often associated with conditions like iron deficiency anemia, where the body lacks sufficient iron to produce adequate hemoglobin. Conditions such as thalassemia, a genetic blood disorder, can also result in lower MCH levels. In such cases, the red blood cells might not be able to carry enough oxygen efficiently.
Again, a low MCH value warrants further investigation to pinpoint the root cause.
Ever wondered about that MCH thing in your blood test results? It’s a measure of the average size of the red blood cells. Now, while that might seem pretty straightforward, understanding conditions like solitary pulmonary nodules can be a bit more complex. These are small, round growths in the lungs, and learning more about them can be really helpful for overall health, especially when interpreting your blood test results in conjunction with a doctor’s analysis.
What are solitary pulmonary nodules can be a factor to consider in interpreting your MCH levels, so understanding both aspects is crucial. Ultimately, though, your MCH is just one piece of the puzzle in understanding your overall health.
Potential Causes for Abnormal MCH Values
Several factors can contribute to abnormal MCH values. Iron deficiency, as mentioned earlier, is a common cause of low MCH levels. Conditions like thalassemia, a genetic disorder affecting hemoglobin production, can also result in abnormally low MCH levels. On the other hand, deficiencies in vitamin B12 or folate can lead to macrocytic anemia, potentially resulting in elevated MCH levels.
Chronic diseases, certain medications, and lifestyle choices can also influence MCH values.
Conditions Associated with Elevated or Decreased MCH
- Elevated MCH: Conditions like megaloblastic anemia (due to vitamin B12 or folate deficiency), liver disease, and certain bone marrow disorders can cause elevated MCH levels. Patients with these conditions may exhibit larger red blood cells containing more hemoglobin than average.
- Decreased MCH: Iron deficiency anemia is a prevalent cause of decreased MCH levels. In this condition, the body’s inability to produce sufficient hemoglobin results in smaller red blood cells with lower hemoglobin content. Other conditions like thalassemia, a genetic blood disorder affecting hemoglobin production, can also cause lower MCH levels.
It’s crucial to understand that the interpretation of MCH values should always be considered in conjunction with other blood test results and a complete medical evaluation. The information presented here is not a substitute for professional medical advice.
Clinical Applications
The Mean Corpuscular Hemoglobin (MCH) isn’t just a number; it’s a crucial piece of the puzzle in understanding a patient’s overall health. Knowing the average amount of hemoglobin within a red blood cell provides valuable insights into the type and severity of various conditions, from simple iron deficiencies to more complex blood disorders. It’s a vital tool in the diagnostic arsenal, helping clinicians determine the appropriate course of treatment and monitor its effectiveness.
Diagnosing Anemia
MCH plays a significant role in diagnosing anemia, a condition characterized by a deficiency of red blood cells or hemoglobin. Lower-than-normal MCH values often indicate a type of anemia where the red blood cells are smaller and contain less hemoglobin. This is frequently seen in iron deficiency anemia, where the body lacks the iron needed to produce sufficient hemoglobin.
Conversely, higher-than-normal MCH values can suggest other types of anemia, like megaloblastic anemia, where the red blood cells are larger and contain more hemoglobin. This difference in cell size and hemoglobin content is a key indicator that clinicians use to differentiate between various types of anemia. For example, a patient with microcytic anemia (small red blood cells) will likely show a low MCH, while a patient with macrocytic anemia (large red blood cells) will exhibit a high MCH.
Assessing Blood Disorders
MCH can also be instrumental in evaluating a wider range of blood disorders beyond anemia. Variations in MCH levels can reflect abnormalities in red blood cell production, destruction, or both. For instance, in conditions like thalassemia, a genetic disorder affecting hemoglobin production, MCH levels can be significantly lower than normal, revealing the underlying issue affecting hemoglobin content within the red blood cells.
Similarly, certain chronic diseases and inflammatory conditions can also impact MCH, providing clinicians with additional clues to the overall health picture.
Monitoring Treatment Effectiveness
The MCH’s role doesn’t end with diagnosis; it also plays a crucial part in monitoring the effectiveness of treatment. For example, if a patient is receiving iron supplements for iron deficiency anemia, observing a gradual increase in their MCH over time can demonstrate that the treatment is working as expected. This dynamic tracking of MCH allows clinicians to adjust treatment strategies and ensure optimal patient outcomes.
In situations where treatment isn’t effective, a persistently low MCH might necessitate exploring alternative therapies or further investigations to determine the root cause of the problem.
Ever wondered what an MCH is in a blood test? It basically measures the average size of your red blood cells. Understanding this can be crucial, especially when considering conditions like congenital adrenal hyperplasia, a rare genetic disorder that affects hormone production. Learning more about this condition can help provide valuable context for interpreting your MCH results.
For a detailed overview of congenital adrenal hyperplasia, check out this helpful resource: congenital adrenal hyperplasia overview. Ultimately, a complete understanding of your MCH requires looking at the bigger picture, including potential underlying health issues.
Using MCH with Other Blood Tests
MCH is not a standalone diagnostic tool. Its usefulness is greatly enhanced when combined with other blood tests. Complete blood counts (CBCs), for instance, provide a comprehensive overview of red blood cell indices, including mean corpuscular volume (MCV) and mean corpuscular hemoglobin concentration (MCHC). Analyzing these values together offers a more nuanced understanding of the patient’s condition, potentially revealing subtle patterns or inconsistencies that might be missed with a single test.
Similarly, MCH values are often correlated with other markers of inflammation, nutritional status, and overall health to develop a comprehensive picture of the patient’s condition.
Table of Conditions and Typical MCH Values
| Condition | Typical MCH Value (pg) | Description |
|---|---|---|
| Iron Deficiency Anemia | Low (e.g., <27 pg) | Red blood cells are smaller and contain less hemoglobin. |
| Megaloblastic Anemia | High (e.g., >32 pg) | Red blood cells are larger and contain more hemoglobin. |
| Thalassemia | Low | Genetic disorder affecting hemoglobin production, resulting in reduced hemoglobin content in red blood cells. |
| Hemolytic Anemia | Variable | Red blood cells are destroyed prematurely, potentially leading to both high and low MCH depending on the specific type. |
| Normal | 27-31 pg | Indicates healthy red blood cell function. |
Note: Values may vary depending on the laboratory and the specific methodology used for measurement. This table provides a general guideline, and individual results should be interpreted in the context of the patient’s overall clinical presentation and other laboratory findings.
Visual Representation
Understanding Mean Corpuscular Hemoglobin (MCH) requires a visual approach to grasp its implications. Visual representations allow us to easily see trends, patterns, and comparisons, making complex data more digestible and insightful. These visualizations aid in diagnosing and monitoring conditions related to red blood cell health.
Graph of MCH Levels Over Time
A line graph plotting MCH levels over time can reveal significant insights. The x-axis represents time (e.g., days, weeks, months), and the y-axis represents MCH values (e.g., picograms). A consistently increasing or decreasing trend can signal an underlying issue, such as iron deficiency or a blood disorder. For example, a patient with iron deficiency anemia might show a gradual decline in MCH levels over several weeks if not treated.
Conversely, an improvement in MCH levels over time could indicate effective treatment.
Diagram of Red Blood Cell Structure and MCH
A diagram depicting a red blood cell (erythrocyte) clearly illustrates the location of hemoglobin. The diagram would highlight the cell membrane surrounding the cytoplasm, which contains hemoglobin molecules. The relative concentration of hemoglobin within the red blood cell directly impacts the MCH value. A larger volume of hemoglobin per cell generally results in a higher MCH. Visualizing this relationship helps connect the intracellular components with the overall MCH measurement.
Image Comparing Normal and Abnormal MCH Values
An image showcasing histograms or box plots of MCH values can be highly informative. One histogram would represent normal MCH ranges, with a peak around the average value. A second histogram would show abnormal MCH values, potentially exhibiting a shift towards higher or lower values. This visual comparison would clearly highlight the difference between normal and abnormal MCH levels, aiding in diagnosis.
For instance, a histogram showing a large number of patients with significantly low MCH values might indicate a prevalent iron deficiency anemia.
Correlation Between MCH and Other Blood Parameters
A scatter plot is an ideal visual tool to illustrate the correlation between MCH and other blood parameters. The x-axis could represent MCH values, while the y-axis could represent other relevant parameters like Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin Concentration (MCHC), Red Blood Cell Count (RBC), or Hemoglobin (Hgb). The scatter plot would demonstrate the relationship between MCH and these other parameters.
A strong positive correlation between MCH and MCV might suggest a condition like macrocytic anemia, where cells are larger and contain more hemoglobin.
Flowchart for MCH Calculation
A flowchart visually represents the steps involved in calculating MCH. It would begin with inputting the hemoglobin (Hgb) value and red blood cell count (RBC). The flowchart would then show the calculation of MCH using the formula:
MCH = (Hgb / RBC) x 10.
The output of the calculation would be the MCH value. This clear step-by-step representation simplifies the process.
Comparison with Related Concepts
Understanding mean corpuscular hemoglobin (MCH) is significantly enhanced by comparing it to related blood parameters. These parameters, while seemingly similar, provide different insights into the characteristics of red blood cells. A comprehensive understanding of these relationships is crucial for accurate interpretation of blood test results and diagnosis of various health conditions.MCH, along with mean corpuscular volume (MCV) and mean corpuscular hemoglobin concentration (MCHC), are key indicators of red blood cell morphology.
These measurements provide a snapshot of the size, hemoglobin content, and concentration within red blood cells, contributing to a complete picture of red blood cell health. Distinguishing between these parameters is essential for pinpointing the underlying cause of any observed abnormalities.
Comparison with MCV
MCV reflects the average size of red blood cells. Larger red blood cells typically indicate macrocytic conditions, while smaller ones suggest microcytic conditions. MCH, on the other hand, focuses on the amount of hemoglobin present in the average red blood cell. Clinical interpretation often involves considering both MCV and MCH together. For instance, a patient with both low MCV and low MCH might suggest iron deficiency anemia.
Comparison with MCHC, What is an mch in a blood test
MCHC, representing the average concentration of hemoglobin within red blood cells, differs from MCH in its focus. While MCH considers the absolute amount of hemoglobin, MCHC assesses the concentration. A low MCHC often indicates conditions like iron deficiency anemia, where the amount of hemoglobin per cell is reduced. Conversely, high MCHC may be associated with conditions where red blood cells contain abnormally high hemoglobin concentrations.
Relationship between MCH, Hemoglobin, and Red Blood Cell Count
MCH is directly related to hemoglobin and red blood cell count. A higher red blood cell count, in general, leads to a higher total hemoglobin level. However, MCH is a measure of theaverage* hemoglobin per cell. The relationship between these parameters can provide valuable clues. For example, if a patient has a normal hemoglobin level but a low MCH, it could suggest a problem with the distribution of hemoglobin within the red blood cells.
Ever wondered what an MCH is in a blood test? It measures the average size of your red blood cells’ hemoglobin. Understanding this can be crucial for diagnosing various health conditions. Now, while we’re on the subject of health systems, did you know there are differences between universal coverage and single payer systems? Learning about these different approaches to healthcare can be enlightening, check out this article on the difference between universal coverage and single payer system to explore this further.
Ultimately, a deeper understanding of MCH values helps paint a clearer picture of your overall health, and that is important.
Summary Table
| Parameter | Definition | Clinical Significance |
|---|---|---|
| MCV | Average volume of a red blood cell. | Indicates red blood cell size; macrocytic or microcytic. |
| MCH | Average amount of hemoglobin in a red blood cell. | Indicates hemoglobin content per red blood cell; low MCH may suggest iron deficiency. |
| MCHC | Average concentration of hemoglobin in a red blood cell. | Indicates hemoglobin concentration; low MCHC may suggest iron deficiency. |
MCH is calculated as (Hemoglobin × 10) / Red Blood Cell Count.
The relationship between these parameters is crucial for diagnosing and managing various hematological conditions. Understanding these relationships is critical to formulating an accurate and appropriate treatment plan.
Additional Considerations
Understanding the nuances of Mean Corpuscular Hemoglobin (MCH) goes beyond simply calculating a number. This section delves into the limitations of MCH testing, factors impacting accuracy, and the crucial role of the complete blood count (CBC) in interpretation. We’ll also explore pre-analytical variables and the importance of proper patient preparation and sample collection.
Limitations of MCH Testing
MCH, while a valuable tool, isn’t without its limitations. It provides a snapshot of average hemoglobin content per red blood cell, but doesn’t offer insight into the underlying causes of abnormalities. For instance, a low MCH might indicate iron deficiency, but other conditions could also contribute to the result. A comprehensive assessment, incorporating other CBC parameters and clinical context, is essential for accurate diagnosis.
Factors Affecting MCH Measurement Accuracy
Several factors can influence the accuracy of MCH measurements. Variations in red blood cell size (anisocytosis) and shape (poikilocytosis), often observed in certain anemias, can skew the average. The presence of abnormal red blood cell populations, like spherocytes or elliptocytes, can also lead to inaccurate MCH values. Additionally, technical errors during the blood analysis process, such as improper sample handling or instrument malfunction, can compromise the reliability of the results.
Importance of the Complete Blood Count (CBC) in Interpreting MCH Results
The MCH value alone is insufficient for a comprehensive understanding of a patient’s hematological status. A complete blood count (CBC) provides a broader picture by including other essential parameters like red blood cell count (RBC), hemoglobin (Hgb), hematocrit (Hct), mean corpuscular volume (MCV), and mean corpuscular hemoglobin concentration (MCHC). Analyzing these parameters in conjunction with MCH allows for a more nuanced interpretation, differentiating between various types of anemia and other blood disorders.
Impact of Pre-Analytical Variables
Pre-analytical variables, occurring before the actual laboratory analysis, significantly impact MCH results. Factors like improper fasting, recent blood transfusions, or hemolysis (red blood cell destruction) in the collected sample can skew the MCH reading. For example, a patient who hasn’t fasted adequately might show artificially elevated glucose levels, which, while not directly related to MCH, can be a confounding variable in the broader clinical picture.
Similarly, hemolyzed samples (where red blood cells are broken down) can result in inaccurate hemoglobin measurements, subsequently affecting MCH.
Patient Preparation and Sample Collection Considerations
Proper patient preparation and sample collection are crucial for obtaining reliable MCH results. Patients should be adequately informed about the procedure and any necessary pre-collection instructions, such as fasting or avoiding strenuous activity. The phlebotomist’s technique plays a vital role in preventing hemolysis and ensuring an accurate sample. Using appropriate collection tubes and handling the sample correctly is paramount.
For example, if a patient is taking medications that affect blood clotting, the phlebotomist must be aware of these factors and adjust the collection procedure accordingly. Failure to adhere to these protocols can lead to inaccurate MCH readings and ultimately, delayed or incorrect diagnosis.
End of Discussion
In conclusion, understanding what is an MCH in a blood test provides valuable insights into red blood cell health. MCH levels, along with other blood parameters, are crucial indicators of potential health issues, from anemia to various blood disorders. This comprehensive overview offers a clear understanding of MCH’s significance in diagnosing, monitoring, and ultimately improving patient care. Remember, consulting a healthcare professional is essential for accurate interpretation and diagnosis.




