What is a thrombotic stroke? It’s a crucial type of stroke caused by a blood clot forming inside a blood vessel in the brain. Unlike other stroke types, this one involves a blockage, rather than bleeding. Understanding the mechanisms, symptoms, and treatment options is key to recognizing and managing this potentially debilitating condition. This detailed exploration delves into the definition, pathophysiology, diagnosis, treatment, prevention, and complications of thrombotic strokes, ensuring you’re well-equipped with knowledge.
Thrombotic strokes are a significant concern in neurology. They often arise from a combination of factors, such as atherosclerosis (hardening of the arteries) and blood clots. Understanding the underlying causes is crucial for developing effective prevention and treatment strategies. Early detection and prompt medical intervention are critical in minimizing the long-term impact of this condition.
Definition and Overview
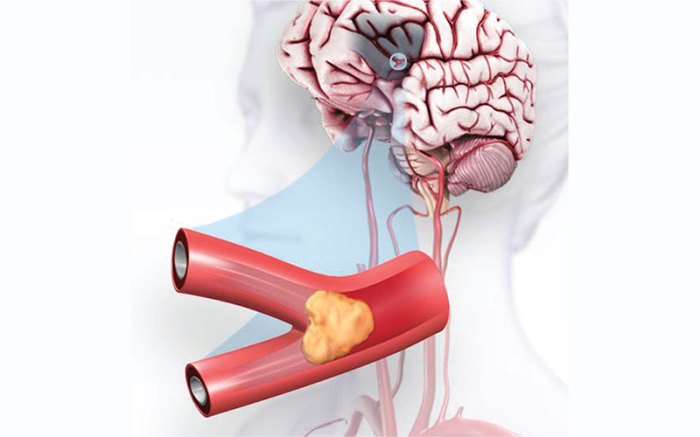
A thrombotic stroke occurs when a blood clot, or thrombus, forms inside a blood vessel in the brain, blocking blood flow to a particular area. This blockage deprives brain cells of oxygen and nutrients, leading to cell death and the characteristic symptoms of a stroke. Understanding the mechanisms behind thrombotic strokes is crucial for early diagnosis and effective treatment.Thrombotic strokes are distinguished from other stroke types, such as hemorrhagic strokes, by the presence of a blood clot obstructing the blood vessel.
Hemorrhagic strokes, on the other hand, are caused by bleeding in the brain. This difference in underlying cause results in distinct symptom profiles and treatment approaches.
A thrombotic stroke happens when a blood clot forms inside a blood vessel in the brain, blocking blood flow. This can lead to various symptoms, and understanding the risk factors is crucial. For example, factors like those associated with macular degeneration, such as high blood pressure and smoking, can increase the likelihood of developing a blood clot. Learning more about these risk factors can help you take proactive steps to maintain good health and potentially reduce your risk of a thrombotic stroke.
Understanding the causes of macular degeneration, as detailed in macular degeneration causes risk factors , can indirectly provide insight into the broader context of vascular health, which is a key component in preventing strokes.
Types of Thrombotic Strokes
Thrombotic strokes can be broadly categorized based on the location and characteristics of the clot. While there isn’t a formal classification into distinct types with rigidly defined criteria, the underlying mechanisms contribute to variations in the stroke’s presentation and impact. For instance, strokes stemming from atherosclerotic plaque buildup in large arteries will often exhibit different symptoms and severity than those caused by smaller blood vessel clots.
The specific vessel affected plays a significant role in determining the region of the brain impacted, thereby influencing the clinical picture.
Risk Factors
Several factors increase the likelihood of developing a thrombotic stroke. These risk factors often overlap with those for other cardiovascular diseases. High blood pressure, high cholesterol, smoking, diabetes, and a history of heart conditions like atrial fibrillation are significant risk factors. Furthermore, a sedentary lifestyle, obesity, and a family history of stroke also contribute to an elevated risk.
Addressing these risk factors through lifestyle modifications and medical interventions is crucial for stroke prevention.
Comparison of Thrombotic and Hemorrhagic Strokes
| Feature | Thrombotic Stroke | Hemorrhagic Stroke |
|---|---|---|
| Cause | Blood clot (thrombus) obstructing blood flow | Bleeding in the brain |
| Symptoms | Gradual onset of symptoms, often over hours; symptoms may include weakness, numbness, speech difficulties, vision problems, and headache | Sudden onset of severe headache, often accompanied by vomiting, stiff neck, and loss of consciousness |
| Treatment | Focus on dissolving the clot (thrombolysis) or preventing further clot formation; anticoagulants or antiplatelet medications may be prescribed; management of underlying conditions | Focus on controlling bleeding, managing blood pressure, and preventing further complications; surgery may be necessary in some cases |
Pathophysiology
Understanding the intricate mechanisms behind thrombotic stroke is crucial for effective prevention and treatment. This section delves into the complex interplay of factors that lead to the formation of blood clots within the arteries, ultimately resulting in stroke. We’ll explore the roles of atherosclerosis, inflammation, and blood flow in this process, highlighting the different types of clots involved.
A thrombotic stroke happens when a blood clot forms inside a blood vessel in the brain, blocking blood flow. While the specifics of blood flow and clot formation are important to understand, it’s fascinating to consider how our sleep preferences, like being a hot sleeper versus a cold sleeper, might influence overall health. For example, understanding how your body temperature affects your blood viscosity, and whether you tend to be a hot sleeper vs cold sleeper , could potentially impact your risk factors.
Ultimately, recognizing the factors that contribute to thrombotic strokes is crucial for prevention and management.
Formation of Blood Clots
Blood clots, or thrombi, form when blood components clump together, obstructing blood flow. This process, known as thrombosis, can occur in various parts of the circulatory system, including the arteries supplying the brain. Several factors contribute to this process, including damage to the blood vessel lining, changes in blood flow, and an imbalance in the clotting factors within the blood.
Role of Atherosclerosis
Atherosclerosis plays a significant role in the development of thrombotic stroke. This chronic disease involves the buildup of plaque, composed of cholesterol, fats, and other substances, within the arterial walls. Over time, this plaque hardens and narrows the arteries, reducing blood flow and increasing the risk of clot formation. The plaque itself can rupture, exposing the underlying tissues to the blood, triggering the clotting cascade.
Examples include the common occurrence of stroke in individuals with a history of heart disease and high cholesterol.
Types of Blood Clots and Stroke
Different types of blood clots can contribute to stroke. Atherosclerotic plaques often rupture, leading to the formation of a thrombus (stationary clot) that directly blocks blood flow. This is a common mechanism in thrombotic stroke. Another type is an embolus (a clot that travels from another location). While not a direct component of the
initial* clot formation in thrombotic stroke, emboli can arise from the rupture of a thrombus in another part of the body and travel to the brain, causing a stroke.
Impact of Inflammation, What is a thrombotic stroke
Inflammation in the blood vessel walls is a critical factor in thrombotic stroke. Inflammation damages the endothelium, the inner lining of the arteries. This damage disrupts the normal balance of clotting factors, increasing the risk of thrombus formation. The inflammatory response can be triggered by various factors, including high blood pressure, high cholesterol, and certain infections.
Impact of Blood Flow
Blood flow plays a critical role in clot formation. Slow or stagnant blood flow allows clotting factors to accumulate and interact, increasing the likelihood of clot formation. Reduced blood flow can occur in narrowed arteries due to atherosclerosis, or in situations of decreased cardiac output. In a healthy state, blood flow helps prevent the formation of clots by maintaining a dynamic interaction between blood constituents.
Flowchart of Thrombotic Stroke Development
Step 1: Endothelial damage (e.g., from atherosclerosis) Step 2: Inflammatory response triggered Step 3: Platelet activation and adhesion to damaged site Step 4: Coagulation cascade initiated (formation of fibrin mesh) Step 5: Thrombus formation (blood clot) Step 6: Partial or complete occlusion of artery Step 7: Reduced blood flow to brain tissue Step 8: Ischemia and potential infarction (tissue death) Step 9: Stroke
Symptoms and Diagnosis
Understanding the symptoms and diagnostic methods for thrombotic stroke is crucial for timely intervention and improved patient outcomes.
Early recognition of warning signs can significantly impact recovery. Prompt diagnosis allows for the initiation of appropriate treatments, potentially minimizing the long-term effects of the stroke.
Potential Symptoms of Thrombotic Stroke
Recognizing the range of potential symptoms is essential for prompt medical attention. Symptoms can vary greatly in severity and presentation, depending on the location and extent of the blood clot. The abrupt onset of symptoms often distinguishes a thrombotic stroke from other neurological conditions.
- Sudden numbness or weakness, especially on one side of the body.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble speaking or understanding speech.
- Sudden difficulty walking, dizziness, loss of balance, or coordination.
- Sudden severe headache with no known cause.
- Sudden confusion, trouble concentrating, or changes in alertness.
- Sudden loss of consciousness or fainting.
Importance of Recognizing Early Warning Signs
Early recognition of the early warning signs of a thrombotic stroke can significantly improve patient outcomes. Timely intervention is critical to limit the damage caused by the stroke. Recognizing these subtle changes and seeking immediate medical attention can make a difference in preventing permanent disabilities.
Diagnostic Methods for Thrombotic Stroke
Several methods are employed to diagnose thrombotic stroke, combining clinical assessments with advanced imaging techniques. A thorough neurological examination is often the first step, followed by blood tests and imaging studies.
- Complete Medical History: Gathering a comprehensive medical history is crucial for identifying potential risk factors and contributing conditions that might be linked to the stroke.
- Physical Examination: A thorough physical examination, including neurological assessments, helps evaluate the patient’s condition and identify potential stroke-related symptoms.
- Blood Tests: Blood tests can help identify potential underlying conditions or factors that may have contributed to the stroke. Examples include checking blood glucose levels, cholesterol levels, and complete blood counts.
Role of Imaging Techniques
Imaging techniques play a vital role in confirming the diagnosis of thrombotic stroke and identifying the location and extent of the clot. These techniques allow physicians to visualize the brain and identify areas of damage.
- Computed Tomography (CT) Scan: A CT scan is a common initial imaging modality used to rapidly evaluate for acute stroke. It can detect the presence of a stroke but may not immediately identify the specific type of stroke. CT scans are particularly useful in ruling out other conditions, such as hemorrhagic stroke.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of the brain and can detect the presence of a thrombus more precisely than a CT scan. MRI is often used to confirm the diagnosis and assess the extent of brain damage in thrombotic stroke.
Summary of Diagnostic Tests
| Test | Description | Significance |
|---|---|---|
| Complete Medical History | Gathering patient’s past medical conditions and risk factors. | Helps identify potential causes and risk factors for stroke. |
| Physical Examination | Neurological assessment to evaluate stroke symptoms. | Identifies neurological deficits and potential stroke-related signs. |
| Blood Tests | Analysis of blood samples to check for conditions like high blood pressure, diabetes, and high cholesterol. | Helps identify underlying medical conditions contributing to stroke risk. |
| CT Scan | Non-invasive imaging technique to assess brain structures for abnormalities. | Quickly identifies the presence of a stroke and differentiates between ischemic and hemorrhagic stroke. |
| MRI | Detailed imaging of the brain to visualize the extent of damage and identify the location of a thrombus. | Provides more detailed information about the stroke, aiding in the diagnosis and assessing the extent of the injury. |
Treatment and Management
Thrombotic stroke, a serious condition demanding swift and comprehensive medical intervention, requires a multifaceted approach. Early treatment is crucial to minimize the extent of brain damage and improve patient outcomes. The primary goals of treatment are to restore blood flow to the affected area, control potential complications, and facilitate recovery.
Primary Goals of Treatment
The immediate goals of treatment for thrombotic stroke center on minimizing brain damage and improving neurological function. These goals are achieved through a combination of medical interventions and supportive care. Strategies aim to limit the infarct size (the area of brain tissue deprived of oxygen and nutrients) and prevent further damage. Rapid action is paramount, as the longer blood flow is interrupted, the greater the risk of irreversible brain damage.
Role of Medications
Medications play a critical role in treating thrombotic stroke. Thrombolytics, such as alteplase (tPA), are crucial in dissolving blood clots, restoring blood flow, and potentially reducing the extent of brain damage. However, their use is time-sensitive and restricted to patients who meet specific criteria. Antiplatelet agents, like aspirin, help prevent the formation of new clots and reduce the risk of recurrent strokes.
Anti-coagulants, like warfarin, are sometimes used to prevent further clot formation. The choice of medication depends on various factors, including the patient’s medical history, the type of stroke, and the time elapsed since the onset of symptoms.
A thrombotic stroke happens when a blood clot forms inside a blood vessel in the brain, blocking blood flow. This can lead to various symptoms, and it’s crucial to understand the underlying causes. One potential factor contributing to these blockages could be an excess of protein in the body, as detailed in this article on signs of too much protein.
Ultimately, recognizing the signs of a thrombotic stroke is vital for prompt treatment and minimizing potential damage.
Importance of Supportive Care
Supportive care is essential in managing a thrombotic stroke. This includes maintaining a stable vital signs, providing adequate hydration, and preventing complications like infections and seizures. Careful monitoring of blood pressure, heart rate, and oxygen levels is crucial to ensure the patient’s overall well-being. Nutritional support and pain management are also important aspects of supportive care.
Role of Rehabilitation
Rehabilitation is critical for stroke recovery, focusing on restoring lost function and improving quality of life. This encompasses physical therapy to regain motor skills, occupational therapy to improve daily living activities, and speech therapy to address communication challenges. The intensity and duration of rehabilitation programs vary depending on the severity of the stroke and the individual’s response to treatment.
Potential Surgical Interventions
In some cases, surgical interventions may be necessary to treat thrombotic stroke. Endovascular thrombectomy, a minimally invasive procedure, can remove large clots from blood vessels in the brain. This technique is particularly useful for patients who are not eligible for thrombolytic therapy or when clots are large or in inaccessible locations. The decision to employ surgical intervention is made on a case-by-case basis, considering factors like the patient’s condition, the location and size of the clot, and the time elapsed since the onset of symptoms.
Treatment Options Table
| Treatment | Description | Effectiveness |
|---|---|---|
| Thrombolytics (e.g., tPA) | Dissolve blood clots to restore blood flow. | Effective if administered within a specific timeframe; can reduce infarct size. |
| Antiplatelet agents (e.g., aspirin) | Prevent further clot formation and reduce risk of recurrent strokes. | Reduces the risk of recurrent events. |
| Anticoagulants (e.g., warfarin) | Prevent further clot formation and reduce risk of recurrent strokes. | May be used in some cases. |
| Endovascular thrombectomy | Removes large clots from blood vessels in the brain. | Effective for large or inaccessible clots; may improve outcomes compared to medication alone. |
| Supportive care | Maintain stable vital signs, prevent complications, provide hydration and nutrition. | Essential for managing overall patient well-being and preventing complications. |
| Rehabilitation | Restore lost function through physical, occupational, and speech therapy. | Crucial for improving quality of life and long-term recovery. |
Prevention

Preventing a thrombotic stroke is crucial for minimizing its devastating impact. By understanding and addressing the risk factors, individuals can significantly reduce their chances of experiencing this debilitating condition. Lifestyle modifications, coupled with appropriate medical interventions, play a vital role in stroke prevention.
A proactive approach to stroke prevention involves identifying and managing risk factors, promoting healthy habits, and utilizing preventative medications. By combining these strategies, individuals can substantially decrease their likelihood of developing a thrombotic stroke.
Lifestyle Modifications
Maintaining a healthy lifestyle is paramount in preventing thrombotic strokes. A balanced diet, regular exercise, and stress management techniques contribute significantly to overall cardiovascular health, reducing the risk of blood clots forming. These modifications can lead to significant improvements in blood pressure, cholesterol levels, and blood sugar control, all of which are key in mitigating stroke risk.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean protein, while limiting saturated and trans fats, sodium, and added sugars, is essential. This helps to maintain healthy cholesterol levels and blood pressure.
- Regular Exercise: Physical activity, such as brisk walking, swimming, or cycling, helps to improve cardiovascular health, regulate blood pressure, and maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Stress Management: Chronic stress can negatively impact blood pressure and contribute to an increased risk of stroke. Employing stress-reducing techniques like meditation, yoga, or deep breathing exercises can significantly improve overall well-being.
Controlling Risk Factors
Controlling risk factors is a cornerstone of stroke prevention. Identifying and managing conditions like hypertension (high blood pressure), hyperlipidemia (high cholesterol), diabetes mellitus, and atrial fibrillation (irregular heartbeat) is crucial. Consistent monitoring and adherence to prescribed treatment plans are essential to mitigate the impact of these conditions.
- Hypertension (High Blood Pressure): Maintaining optimal blood pressure levels through medication, lifestyle modifications, and regular checkups is vital. High blood pressure is a significant risk factor for stroke, and consistent control can significantly reduce the likelihood of a thrombotic event.
- Hyperlipidemia (High Cholesterol): Elevated cholesterol levels can contribute to plaque buildup in the arteries, increasing the risk of blood clots. Dietary changes, exercise, and medications can help manage cholesterol levels and reduce the risk of stroke.
- Diabetes Mellitus: Diabetes can damage blood vessels and increase the risk of blood clots. Strict adherence to a diabetes management plan, including diet, exercise, and medication, is crucial for reducing stroke risk.
- Atrial Fibrillation (AFib): AFib is a condition where the heart beats irregularly, increasing the risk of blood clots. Treatment with anticoagulant medications or other interventions is often necessary to manage AFib and prevent stroke.
Preventative Medications
Certain medications can significantly reduce the risk of thrombotic stroke, particularly for individuals with existing risk factors. These medications act to prevent blood clots from forming or to dissolve existing clots.
- Anticoagulants: These medications, such as warfarin and newer oral anticoagulants (NOACs), prevent blood clots from forming by interfering with the clotting process. They are particularly important for individuals with conditions like atrial fibrillation.
- Antiplatelet Agents: These medications, such as aspirin, clopidogrel, and others, help prevent blood clots by inhibiting platelet aggregation. They are often prescribed to individuals with a history of stroke or other cardiovascular events.
Examples of Preventive Measures
Implementing preventative measures can be illustrated by real-life examples. A patient with a history of high blood pressure, who adopts a low-sodium diet, engages in regular exercise, and takes prescribed medications, significantly reduces their risk of stroke.
Lifestyle Changes to Reduce Stroke Risk
- Quit Smoking: Smoking significantly increases the risk of blood clots and damages blood vessels, greatly increasing the risk of stroke. Quitting smoking is one of the most impactful lifestyle changes for stroke prevention.
- Maintain a Healthy Weight: Obesity increases the risk of hypertension, hyperlipidemia, and diabetes, all major risk factors for stroke. Maintaining a healthy weight through diet and exercise is crucial.
- Limit Alcohol Consumption: Excessive alcohol consumption can lead to high blood pressure and other health problems that increase stroke risk. Limiting alcohol intake is an important aspect of stroke prevention.
Preventative Strategies Summary
| Strategy | Description | Impact |
|---|---|---|
| Balanced Diet | Rich in fruits, vegetables, and whole grains, low in saturated and trans fats, sodium, and added sugars. | Improves cardiovascular health, regulates blood pressure, and controls cholesterol levels. |
| Regular Exercise | Aerobic activity for at least 150 minutes per week. | Improves cardiovascular health, regulates blood pressure, and helps maintain a healthy weight. |
| Stress Management | Techniques like meditation, yoga, or deep breathing. | Reduces stress levels, which can impact blood pressure and overall cardiovascular health. |
| Controlling Risk Factors | Monitoring and managing hypertension, hyperlipidemia, diabetes, and AFib. | Reduces the impact of these conditions and lowers stroke risk. |
| Preventative Medications | Anticoagulants and antiplatelet agents. | Prevent blood clots from forming or dissolve existing clots. |
Complications
Thrombotic stroke, while treatable, can leave lasting impacts on a patient’s life. Understanding the potential complications is crucial for both patients and healthcare providers to develop comprehensive management strategies. Addressing these complications often requires a multidisciplinary approach, encompassing medical interventions, rehabilitation, and emotional support.
Potential Physical Complications
Post-stroke complications encompass a wide range of physical issues. These can significantly impact a patient’s ability to perform daily activities and maintain their independence. Recognizing and addressing these complications early on can improve outcomes and quality of life.
- Neurological Deficits: Beyond the initial stroke symptoms, further neurological impairments can develop. These can include weakness, numbness, paralysis, speech difficulties (aphasia), swallowing problems (dysphagia), and cognitive dysfunction. For example, a patient might experience worsening weakness in their left arm following a thrombotic stroke, requiring physical therapy to regain strength.
- Pressure Sores (Decubitus Ulcers): Immobility and reduced sensation, common after a stroke, can lead to pressure sores. These can be painful and increase the risk of infection. Careful positioning, regular skin checks, and appropriate pressure-reducing devices are vital in preventing these sores.
- Cardiovascular Complications: Stroke patients are at a higher risk of developing heart problems, such as heart failure, arrhythmias, and blood clots. Regular monitoring of heart health is essential for preventing further complications.
- Respiratory Issues: Reduced mobility and muscle weakness can impair breathing function. Individuals may experience difficulty clearing secretions from their lungs, leading to pneumonia. Respiratory therapy and appropriate airway management are critical to prevent respiratory complications.
Long-Term Effects on Quality of Life
Stroke significantly impacts a patient’s quality of life. The extent of this impact depends on the severity of the stroke and the individual’s resilience.
- Emotional Distress: The emotional toll of stroke can be substantial. Patients may experience anxiety, depression, frustration, and grief due to the loss of independence and changes in their lives. Psychotherapy and support groups can play a vital role in managing these emotions.
- Social Isolation: Physical limitations and communication difficulties can lead to social isolation. Patients might withdraw from social activities and feel alienated from their support networks. Encouraging social interaction and providing support groups are crucial in minimizing this impact.
- Economic Burden: The costs associated with stroke care, rehabilitation, and long-term support can place a considerable strain on patients and their families. Financial assistance and support programs can help alleviate this burden.
- Reduced Independence: Many stroke survivors require ongoing assistance with daily activities, impacting their independence. Adaptive equipment and support services can help maintain independence.
Strategies for Managing Post-Stroke Complications
Effective management of post-stroke complications necessitates a proactive approach.
- Early Intervention and Rehabilitation: Prompt initiation of physical, occupational, and speech therapy is crucial for regaining lost function and minimizing long-term impairments. For instance, early speech therapy can help a patient relearn communication skills after aphasia.
- Preventative Measures: Strategies like maintaining good blood pressure, managing cholesterol levels, and controlling diabetes can help prevent further strokes and complications. This proactive approach is vital in managing long-term health issues.
- Adaptive Equipment and Assistive Technology: Adaptive equipment, such as ramps, grab bars, and assistive devices, can improve mobility and independence. Adaptive utensils and communication aids can also help individuals with swallowing or speech difficulties.
Importance of Ongoing Care
Ongoing care is paramount for stroke survivors. This includes regular medical check-ups, follow-up therapy sessions, and psychosocial support. This ongoing support allows for the early detection and management of any emerging issues.
- Regular Medical Monitoring: Ongoing monitoring of vital signs, blood pressure, and blood glucose levels is critical to identify and address any potential complications.
- Patient Education: Educating patients and their families about the stroke and its potential complications is crucial for self-management and early detection.
Potential Long-Term Complications of Thrombotic Stroke
- Neurological impairments (e.g., hemiparesis, aphasia, dysarthria, cognitive deficits)
- Depression and anxiety
- Pressure sores
- Cardiovascular complications (e.g., heart failure, arrhythmias)
- Respiratory complications (e.g., pneumonia)
- Gastrointestinal problems
- Urinary incontinence
- Falls
- Social isolation
- Reduced quality of life
Final Wrap-Up: What Is A Thrombotic Stroke
In conclusion, thrombotic strokes represent a complex interplay of vascular factors and lifestyle choices. Recognizing the risk factors, understanding the diagnostic process, and embracing preventative measures are vital in mitigating the impact of this condition. Effective treatment, including medication and rehabilitation, is essential for optimizing recovery and minimizing long-term complications. This comprehensive overview equips you with the knowledge needed to approach thrombotic strokes with awareness and informed action.




