What helps with period cramps? This guide delves into the multifaceted nature of menstrual cramps, exploring everything from the physiological causes and common symptoms to effective relief methods and lifestyle adjustments. We’ll uncover the role of hormones, examine over-the-counter pain relievers, and explore alternative remedies, ultimately empowering you to better understand and manage your menstrual discomfort.
Understanding the root causes of period cramps is crucial. Hormonal fluctuations, stress levels, and underlying conditions all play a significant role in the severity of pain. This comprehensive exploration covers various factors, providing actionable insights and practical solutions to help you navigate these challenging times.
Understanding Period Cramps
Menstrual cramps, or dysmenorrhea, are a common experience for many women. They can range from mild discomfort to debilitating pain, significantly impacting daily life. Understanding the physiological causes, symptoms, and contributing factors can empower individuals to manage these cramps effectively.A deep dive into the science behind period cramps reveals a complex interplay of hormonal fluctuations and muscular contractions within the uterus.
This intricate process often leads to the characteristic pain associated with menstruation. Comprehending these mechanisms can illuminate strategies for alleviating discomfort and enhancing overall well-being.
Physiological Causes of Menstrual Cramps
The uterine lining, the endometrium, sheds during menstruation. This shedding process is accompanied by the release of prostaglandins, naturally occurring fatty acids. High levels of prostaglandins trigger powerful contractions in the uterine muscles. These contractions, while necessary for shedding the uterine lining, can cause intense pain. The process can also be influenced by other factors, such as blood clots or inflammation.
Common Symptoms of Period Cramps
Symptoms vary in intensity and can range from mild to severe. Common symptoms include abdominal pain, cramping, lower back pain, and radiating pain in the thighs. The intensity of these symptoms can vary depending on the individual and the severity of the cramps. Some women experience nausea, vomiting, or even headaches.
Types of Period Cramps and Their Origins
Period cramps can be categorized into two primary types: primary and secondary dysmenorrhea. Primary dysmenorrhea is the most common type and is associated with the normal hormonal fluctuations during menstruation. Secondary dysmenorrhea is linked to underlying medical conditions, such as endometriosis or uterine fibroids. Identifying the type of dysmenorrhea can guide appropriate management strategies.
Role of Hormones in Menstrual Cramps
Hormones play a critical role in regulating the menstrual cycle and influencing the severity of cramps. Prostaglandins, released in response to fluctuating levels of estrogen and progesterone, are key players in the uterine contractions associated with pain. Fluctuations in these hormone levels can trigger or exacerbate menstrual cramps.
Dealing with period cramps can be tough, but thankfully there are lots of things that can help. Heating pads, gentle exercise, and even over-the-counter pain relievers can often make a big difference. While we’re on the topic of discomfort, it’s important to be aware of unusual bodily changes. For instance, if you’re concerned about a potential issue like an STD, understanding what an STD might smell like – like onions, for example – can be a crucial part of early detection.
what std smells like onions is a good resource to learn more. Ultimately, focusing on healthy habits and paying attention to your body can help ease period discomfort.
Factors Contributing to the Severity of Period Cramps
| Factor | Description | Impact on Cramps | Mitigation Strategies |
|---|---|---|---|
| Hormonal Fluctuations | Changes in estrogen and progesterone levels during the menstrual cycle. | High levels of prostaglandins trigger intense uterine contractions, leading to pain. | Over-the-counter pain relievers, hormonal birth control, and lifestyle adjustments. |
| Stress Levels | Elevated levels of stress hormones like cortisol can increase prostaglandin production. | Increased stress can worsen the intensity of cramps and cause related symptoms. | Stress management techniques like yoga, meditation, or spending time in nature. |
| Underlying Conditions | Conditions like endometriosis, uterine fibroids, or pelvic inflammatory disease. | These conditions can cause chronic pain and worsen menstrual cramps. | Consult a healthcare professional for diagnosis and treatment of underlying conditions. |
Over-the-Counter Relief Methods
Dealing with period cramps can be tough, and thankfully, many over-the-counter pain relievers offer effective relief. Understanding the different options and their potential side effects is key to choosing the best approach for your individual needs. This section dives into the various types of over-the-counter pain relievers, their mechanisms of action, and how they compare in terms of effectiveness and potential side effects.Over-the-counter pain relievers are commonly used to manage period cramps, and they work by targeting different pathways in the body.
Choosing the right medication often depends on individual tolerance and the severity of the pain. Some medications are more effective at reducing inflammation, while others primarily focus on pain signals. Knowing the specific active ingredients and their mechanisms of action can help you understand how they work and which might be most suitable for you.
Common Over-the-Counter Pain Relievers, What helps with period cramps
Various over-the-counter pain relievers are commonly used for period cramps. These include ibuprofen, naproxen, and acetaminophen. Each has its own unique mechanism of action and potential side effects. Understanding these differences can help you make informed decisions about which medication might be best for you.
Comparing Ibuprofen, Naproxen, and Acetaminophen
The table below provides a comparison of ibuprofen, naproxen, and acetaminophen, highlighting their strengths, dosages, and potential side effects. Remember that this is not an exhaustive list and individual experiences may vary. Consult with a healthcare professional if you have concerns about taking any of these medications.
| Medication | Strength | Dosage | Side Effects |
|---|---|---|---|
| Ibuprofen | 200 mg, 400 mg, 600 mg | Take 200-400 mg every 4-6 hours, as needed, up to a maximum of 1200 mg per 24 hours. | Stomach upset, nausea, heartburn, dizziness, headache, and rarely, allergic reactions. Long-term use can increase the risk of kidney problems in individuals with pre-existing conditions. |
| Naproxen | 220 mg, 275 mg, 500 mg | Take 220-500 mg every 6-8 hours, as needed, up to a maximum of 1250 mg per 24 hours. | Stomach upset, nausea, heartburn, dizziness, headache, and rarely, allergic reactions. Like ibuprofen, long-term use can increase the risk of kidney problems in individuals with pre-existing conditions. Naproxen may also have a higher risk of gastrointestinal issues compared to ibuprofen in some individuals. |
| Acetaminophen | 325 mg, 500 mg | Take 325-650 mg every 4-6 hours, as needed, up to a maximum of 4000 mg per 24 hours. | Liver damage is a serious concern if taken in excessive amounts. Stomach upset, nausea, and allergic reactions are also possible side effects. Acetaminophen primarily targets pain signals and is less effective at reducing inflammation compared to ibuprofen or naproxen. |
Lifestyle Modifications
Beyond over-the-counter medications and heat packs, significant relief from period cramps can often be achieved through lifestyle adjustments. These modifications can address underlying factors contributing to discomfort and promote overall well-being. Implementing these changes consistently can lead to a noticeable improvement in menstrual cycle management and overall health.Adopting healthy habits, like regular exercise and stress reduction techniques, can profoundly impact the severity of period cramps.
A balanced diet and adequate hydration play a vital role in supporting your body’s natural processes during menstruation. By incorporating these lifestyle changes, you can effectively manage your menstrual cycle and minimize the impact of cramps on your daily life.
Regular Exercise
Physical activity can significantly reduce menstrual cramps by increasing blood flow and releasing endorphins, natural mood elevators. Regular exercise, even moderate intensity, helps to relax muscles and alleviate tension. This relaxation effect can ease cramping sensations and potentially reduce the severity of pain. Consistent physical activity can also contribute to better overall health and well-being, which further supports menstrual cycle regulation.
Adequate Sleep
Sufficient sleep is essential for hormonal balance and overall bodily function. Lack of sleep can disrupt hormone production, potentially exacerbating menstrual cramps. Aiming for 7-9 hours of quality sleep per night can help regulate hormones, reduce stress, and promote relaxation, all of which contribute to managing menstrual discomfort. Creating a relaxing bedtime routine and establishing a consistent sleep schedule can significantly improve sleep quality.
Stress Management
Chronic stress can affect hormonal balance, impacting the menstrual cycle and potentially increasing the severity of cramps. Stress management techniques, such as yoga, meditation, deep breathing exercises, or spending time in nature, can help reduce stress levels and promote relaxation. Mindfulness practices can help manage stress by focusing on the present moment and reducing anxiety. These practices can positively impact the body’s overall response to menstruation, potentially leading to a decrease in pain perception.
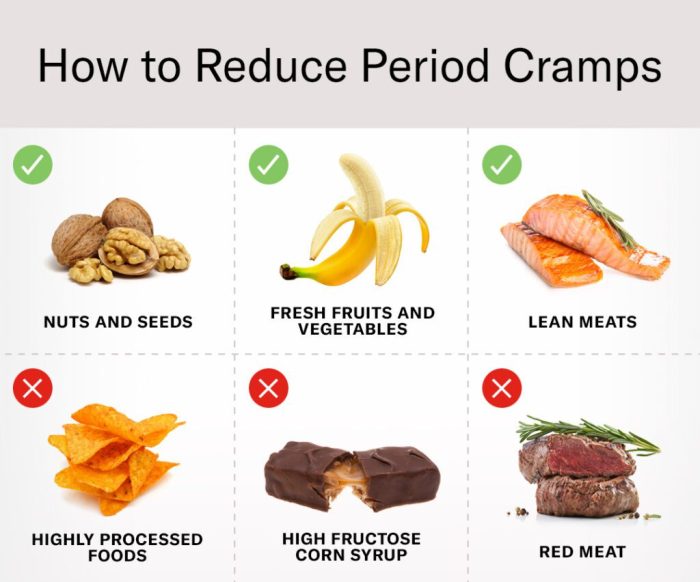
Healthy Diet and Hydration
Maintaining a healthy diet rich in fruits, vegetables, and whole grains, while limiting processed foods, caffeine, and alcohol, can positively influence menstrual cycle health. Proper nutrition supports the body’s natural processes and reduces inflammation. Adequate hydration is crucial for overall bodily functions, including blood flow and muscle relaxation, which can contribute to alleviating cramping. Drinking plenty of water throughout the day can help support the body’s natural processes during menstruation.
Specific Exercises and Stretches
Certain exercises and stretches can target the lower abdomen and pelvic region, easing muscle tension and promoting relaxation. Gentle yoga poses, like child’s pose and seated forward bends, can stretch and relieve tension in the lower back and abdomen. Walking, swimming, or light cardio can also improve blood flow, reducing cramping. These exercises, when performed regularly, can become a part of a healthy routine that supports menstrual well-being.
| Lifestyle Change | Description | Benefits |
|---|---|---|
| Regular Exercise | Engage in at least 30 minutes of moderate-intensity exercise most days of the week. Examples include brisk walking, swimming, or cycling. | Increased blood flow, endorphin release, muscle relaxation, and reduced tension. |
| Adequate Sleep | Aim for 7-9 hours of quality sleep per night. Establish a relaxing bedtime routine and maintain a consistent sleep schedule. | Improved hormonal balance, reduced stress, relaxation, and better regulation of menstrual cycles. |
| Stress Management | Practice stress-reducing techniques such as yoga, meditation, deep breathing exercises, or spending time in nature. | Reduced stress levels, improved relaxation, and a positive impact on the body’s response to menstruation. |
| Healthy Diet and Hydration | Consume a balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, caffeine, and alcohol. Drink plenty of water throughout the day. | Support for natural bodily processes, reduced inflammation, and improved blood flow and muscle relaxation. |
Alternative Remedies and Therapies
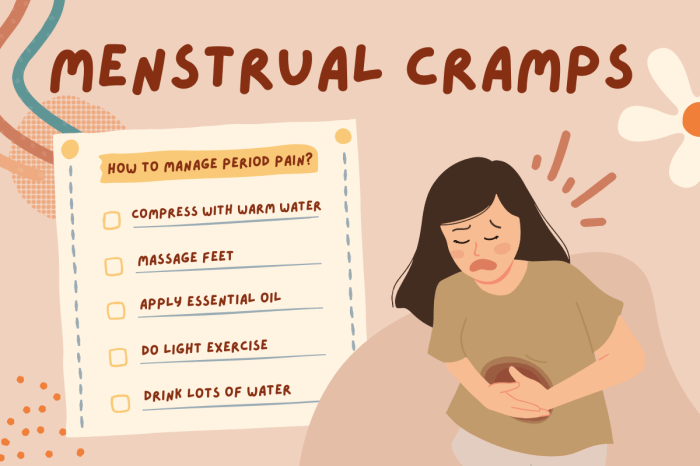
Beyond over-the-counter medications and lifestyle adjustments, various alternative remedies and therapies offer potential relief for period cramps. These methods often focus on addressing the underlying causes of pain and promoting overall well-being, complementing conventional approaches. However, it’s crucial to remember that the effectiveness of these remedies can vary significantly from person to person, and they should not be considered a substitute for medical advice from a healthcare professional.Many alternative therapies aim to reduce muscle tension and inflammation, which are common contributors to menstrual cramps.
Understanding how these methods work can help individuals make informed decisions about incorporating them into their pain management strategies.
Heat Packs
Applying heat to the lower abdomen is a popular and often effective method for easing menstrual cramps. Heat promotes blood flow to the area, relaxing uterine muscles and reducing pain signals. A warm bath, heating pad, or even a hot water bottle can provide soothing relief.
Acupressure
Acupressure involves applying pressure to specific points on the body, believed to stimulate energy flow and alleviate pain. Certain acupressure points, when pressed, may help reduce muscle spasms and promote relaxation. While research on acupressure’s effectiveness for menstrual cramps is ongoing, anecdotal evidence suggests it can provide comfort for some individuals.
Herbal Teas
Herbal teas, such as chamomile, ginger, and fennel, are frequently used to ease menstrual cramps. These teas are believed to have anti-inflammatory and analgesic properties. Ginger, in particular, has demonstrated potential for reducing pain and inflammation. However, individual responses to herbal remedies can vary. Consult with a healthcare professional before incorporating herbal teas into a pain management plan, especially if you have underlying health conditions or are taking other medications.
Heat packs are a lifesaver for period cramps, and sometimes, a change in diet can help too. But, if you’re wondering why you’re suddenly sweating more than usual, it could be due to various factors, including hormonal changes, stress, or even underlying health conditions. Check out this article on why do i sweat so much to explore potential causes.
Regardless, taking pain relievers like ibuprofen and getting enough rest are key to managing those cramps.
Yoga and Meditation
Yoga and meditation practices can help manage stress and promote relaxation, which are crucial for reducing pain perception during menstruation. Relaxation techniques can also help to reduce muscle tension and promote overall well-being. Incorporating these practices into a routine can contribute to a comprehensive approach to menstrual pain management.
Important Considerations
It is essential to acknowledge that the effectiveness of alternative remedies for period cramps can vary greatly among individuals. While some people find significant relief, others may not experience any noticeable benefits. Furthermore, it’s important to be mindful of potential risks. For example, prolonged use of heat packs may lead to skin irritation. Herbal remedies can interact with medications, so it is crucial to consult with a healthcare professional before using them.
It is also important to note that alternative remedies are not intended to replace conventional medical treatments or professional guidance.
Dealing with period cramps can be tough, but there are ways to manage them! Heat packs and gentle exercise are often helpful. And remember, reducing stress can significantly impact your overall well-being, including your period symptoms. Learning techniques like deep breathing and meditation, or even checking out some helpful resources on how to reduce stress could make a big difference.
Ultimately, finding what works best for you, whether it’s lifestyle changes or over-the-counter pain relief, is key to managing those cramps effectively.
When to Seek Medical Attention
Period cramps, while a common experience, can sometimes signal an underlying issue. Knowing when to seek medical help is crucial for ensuring your well-being and getting the right treatment. Ignoring persistent or severe pain can lead to complications, so understanding the warning signs is essential.Severe cramps that significantly impact your daily life, or those accompanied by other symptoms, warrant a visit to a healthcare professional.
This includes pain that doesn’t respond to over-the-counter medications or lifestyle changes. It’s important to remember that what constitutes “severe” is subjective and depends on your individual experience.
Signs and Symptoms Requiring Medical Attention
Understanding the nuances of period pain is key to recognizing when professional help is needed. Beyond the typical discomfort, certain symptoms should prompt a visit to a doctor. These include:
- Pain that radiates beyond the lower abdomen, such as to the back or thighs.
- Severe pain that prevents you from performing your usual daily activities.
- Pain that increases in severity over time or is significantly worse than previous periods.
- Pain accompanied by fever, nausea, vomiting, or diarrhea.
- Pain associated with heavy bleeding, clots, or unusual discharge.
- Sudden, sharp, or stabbing pain, not just a dull ache.
Underlying Conditions Causing Severe or Persistent Menstrual Cramps
Several medical conditions can contribute to severe or persistent menstrual cramps. Identifying these conditions allows for appropriate treatment and management.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus, leading to inflammation and pain.
- Adenomyosis: A condition where the uterine lining grows into the muscular wall of the uterus, often causing heavier bleeding and intense pain.
- Fibroids: Benign tumors in the uterus that can cause heavy bleeding and cramping.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs, often causing severe pain, fever, and unusual discharge. This is a serious condition that needs prompt medical attention.
- Pelvic Adhesions: Scar tissue that develops in the pelvic region, potentially leading to chronic pain and difficulties with fertility.
Questions to Ask Your Healthcare Provider
Having a clear understanding of your condition is crucial for effective management. Asking your healthcare provider specific questions about your period cramps helps you make informed decisions.
- What could be causing my severe or persistent cramps?
- What diagnostic tests are recommended to determine the underlying cause?
- What treatment options are available, and what are their potential side effects?
- How can I manage my cramps effectively, both short-term and long-term?
- What lifestyle changes might help alleviate my symptoms?
- Are there any potential complications associated with my symptoms, and how can they be prevented?
- How frequently should I follow up for monitoring?
Last Recap: What Helps With Period Cramps
In conclusion, managing period cramps effectively involves a multifaceted approach. From understanding the underlying physiological causes to utilizing over-the-counter pain relief, adopting healthy lifestyle choices, and considering alternative remedies, you now possess a toolkit for managing your menstrual discomfort. Remember, seeking medical attention when necessary is crucial. This guide provides a comprehensive overview to empower you to take control of your well-being.




