What causes dry eyes all of a sudden? This is a common question, and the answer is often more complex than you might think. Sudden dry eye can stem from a variety of factors, ranging from simple environmental changes to more serious underlying medical conditions. This article delves into the multifaceted causes of this frustrating eye problem, providing a comprehensive overview to help you understand the potential triggers.
From the impact of medications and treatments to the subtle influence of lifestyle choices, we’ll explore the different contributing factors behind sudden dry eye. We’ll examine medical conditions, environmental influences, and even the role of everyday habits in this often-misunderstood issue. This in-depth exploration will provide insights into the mechanisms behind each cause, the associated symptoms, and how to approach diagnosis.
Sudden Dry Eye Causes: Medical Conditions
Sudden onset dry eye can be a symptom of an underlying medical condition, rather than simply environmental factors. Understanding these potential causes is crucial for accurate diagnosis and effective treatment. This section delves into medical conditions that can trigger dry eye, examining the mechanisms, symptoms, and diagnostic approaches.Medical conditions can disrupt the delicate balance of tear production and drainage, leading to the sudden onset of dry eye.
These conditions can affect various body systems, impacting the nerves, glands, and overall health that contribute to tear film stability. Recognizing these conditions is vital for timely intervention and appropriate management.
Endocrine System Conditions
Several endocrine disorders can affect tear production and quality. These conditions often lead to systemic changes that impact the tear film. Diabetes mellitus, for example, can impact the nerves and blood vessels involved in tear production. Thyroid disorders, such as hypothyroidism, can also disrupt the overall body’s metabolic function, potentially leading to decreased tear production.
- Diabetes Mellitus: This condition can damage the nerves and blood vessels throughout the body, including those responsible for tear production. Patients with uncontrolled diabetes may experience a sudden onset of dry eye symptoms as a result of nerve damage. Symptoms might include blurry vision, frequent infections in the eye, and other systemic diabetic complications. Diagnosis involves blood glucose tests, A1C levels, and possibly nerve conduction studies to evaluate nerve damage.
- Hypothyroidism: This condition slows down the body’s metabolic rate. This can impact tear production by reducing the activity of the glands that create tears. Symptoms often include fatigue, weight gain, and cold intolerance. Dry eye may be one of the less obvious signs, and it may be confused with other conditions. Diagnosis is typically done with blood tests, measuring thyroid hormone levels.
Doctors may also evaluate other symptoms and conduct physical examinations.
Neurological Conditions
Certain neurological disorders can impact the nerves that control tear production and drainage. These conditions can interfere with the signal transmission from the brain to the glands responsible for producing tears.
- Multiple Sclerosis (MS): MS is an autoimmune disease that attacks the protective covering of nerves. The damage to these nerves can disrupt the normal signaling pathways, including those involved in tear production. Symptoms of dry eye can vary greatly depending on the location and severity of the nerve damage. Diagnosis typically involves a combination of neurological exams, MRI scans of the brain and spinal cord, and sometimes evoked potential studies to evaluate nerve function.
- Parkinson’s Disease: This progressive neurological disorder affects motor control. The disease process can impact the nerves that control tear production and drainage. Dry eye can be a significant symptom, sometimes overlooked in the early stages. Symptoms typically include tremors, rigidity, and slowness of movement. Diagnosis relies on a comprehensive neurological evaluation, including a physical examination, and potentially imaging studies and blood tests to rule out other conditions.
Autoimmune Conditions
Autoimmune disorders can cause inflammation in various parts of the body, including the tear glands. This inflammation can lead to decreased tear production and dry eye.
- Sjögren’s Syndrome: This autoimmune disorder primarily affects the moisture-producing glands throughout the body, including the tear glands. It’s often associated with dry eyes and a dry mouth. Symptoms can vary from mild to severe. Diagnosis often involves a combination of clinical evaluation, Schirmer’s test (to measure tear production), and blood tests for specific autoantibodies.
Comparison Table
| Medical Condition | Impact on Tear Production | Typical Symptoms (Beyond Dry Eye) | Diagnostic Tests |
|---|---|---|---|
| Diabetes Mellitus | Decreased tear production due to nerve and vascular damage | Increased thirst, frequent urination, fatigue, blurred vision | Blood glucose tests, A1C, nerve conduction studies |
| Hypothyroidism | Decreased tear production due to metabolic slowdown | Fatigue, weight gain, cold intolerance, constipation | Thyroid hormone levels, physical examination |
| Multiple Sclerosis | Disruption of nerve signals to tear glands | Muscle weakness, numbness, vision problems, fatigue | Neurological exams, MRI scans, evoked potential studies |
| Parkinson’s Disease | Potential impact on tear production due to neurological dysfunction | Tremors, rigidity, slow movement, postural instability | Neurological exams, imaging studies, blood tests |
| Sjögren’s Syndrome | Significant decrease in tear production due to autoimmune inflammation | Dry mouth, fatigue, joint pain, swollen glands | Schirmer’s test, blood tests for autoantibodies, clinical evaluation |
Sudden Dry Eye Causes: What Causes Dry Eyes All Of A Sudden
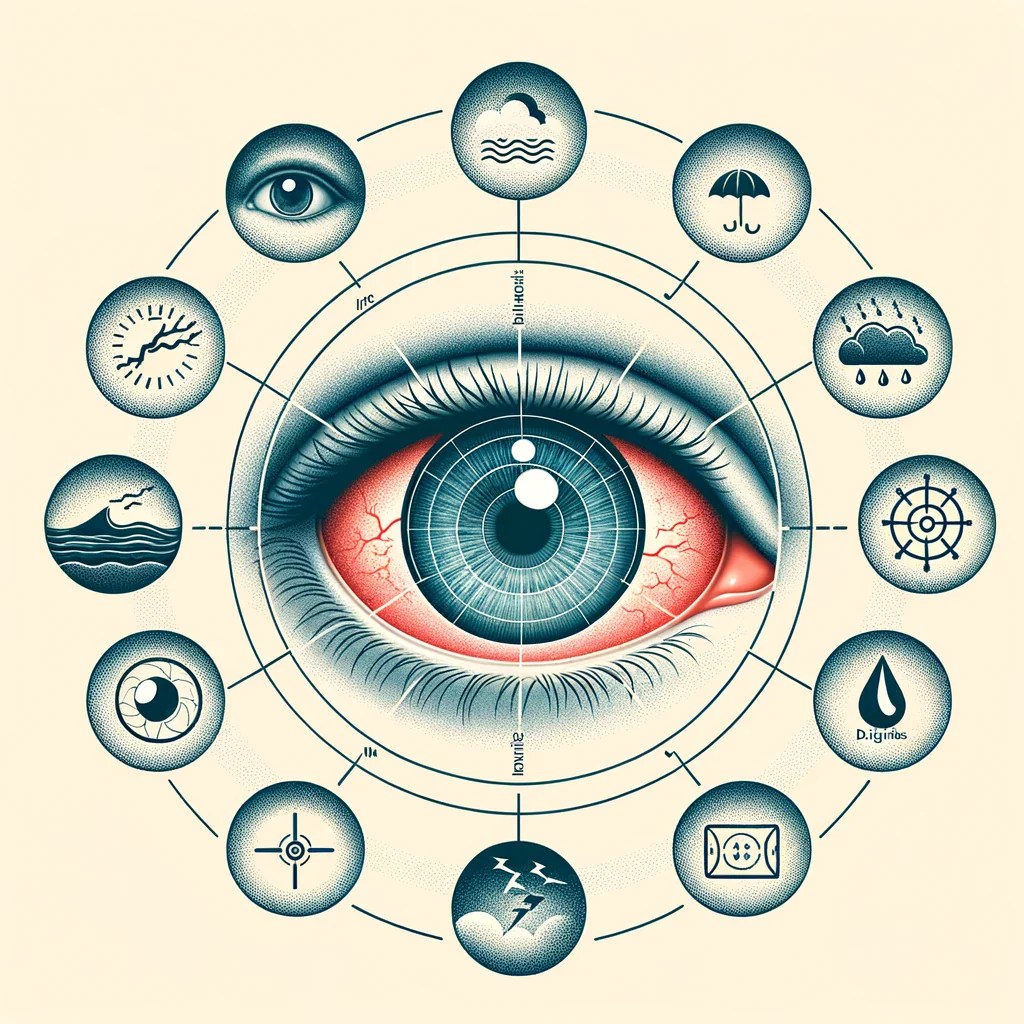
Sudden dry eye can be a frustrating and uncomfortable condition, often arising unexpectedly. While underlying medical conditions are a significant factor, environmental factors can also play a crucial role in triggering or exacerbating this issue. Understanding these triggers can help individuals take proactive steps to manage and prevent dry eye episodes.Environmental factors can significantly influence the delicate balance of the tear film, impacting its ability to effectively lubricate the eye.
Changes in temperature, humidity, and air quality can disrupt this balance, leading to dryness. Certain environmental exposures, like prolonged exposure to wind or dry air, can also contribute to the problem.
Environmental Triggers and Their Impact on Tear Film
Environmental conditions can greatly affect the stability and quality of the tear film. Changes in temperature and humidity are particularly influential. Extreme temperatures, whether very hot or very cold, can alter the evaporation rate of tears. Low humidity levels often lead to increased tear evaporation, making the eyes feel dry and irritated. Poor air quality, especially air containing pollutants or irritants, can further disrupt the tear film’s ability to maintain its protective function.
Specific Environmental Exposures and Dry Eye
Certain environmental exposures can directly contribute to or exacerbate dry eye. Prolonged exposure to wind, especially strong or gusty winds, can significantly increase tear evaporation. Dry, indoor environments, such as air-conditioned offices or homes with low humidity, can also contribute to dry eye. Air travel, with its often-dehydrated cabin air, is another common scenario associated with dry eye.
Similarly, exposure to smoke, dust, or other airborne irritants can trigger inflammation and dryness in the eyes.
Impact of Environmental Conditions on Tear Production and Quality
| Environmental Condition | Impact on Tear Production | Impact on Tear Quality |
|---|---|---|
| Low Humidity | Decreased tear production, increased tear evaporation | Reduced tear film stability, thinning of the tear film |
| High Temperature | Increased tear evaporation | Reduced tear film thickness, decreased lubrication |
| Strong Wind | Increased tear evaporation | Reduced tear film stability, increased irritation |
| Dry Indoor Environments | Decreased tear production, increased tear evaporation | Reduced tear film thickness, increased surface tension |
| Air Travel | Decreased tear production, increased tear evaporation | Reduced tear film stability, thinning of the tear film |
| Airborne Irritants (Smoke, Dust) | Increased tear production (reflexive response), possible inflammation | Reduced tear film quality, potential for irritation and damage |
Work Environments and Activities Associated with Increased Dry Eye Risk, What causes dry eyes all of a sudden
Certain work environments and activities are associated with a heightened risk of dry eye. Individuals working in air-conditioned offices, computer programmers, and those in occupations requiring prolonged screen time are particularly susceptible. Workers in dusty or windy environments, such as construction or agricultural settings, are also at a greater risk. Furthermore, individuals who frequently engage in activities like reading, driving, or using digital devices for extended periods are more prone to dry eye symptoms.
This is especially true when these activities occur in low-humidity environments. For example, a software engineer spending eight hours a day staring at a computer screen in a dry, air-conditioned office is at a higher risk of developing dry eye.
Sudden Dry Eye Causes: What Causes Dry Eyes All Of A Sudden

Sudden dry eye can be a frustrating and uncomfortable condition, often appearing seemingly out of nowhere. While many factors can contribute to this issue, a significant portion of cases are linked to medications and treatment protocols. Understanding the connection between specific medications and dry eye is crucial for effective management and prevention.
Medications Associated with Dry Eye
Certain medications can directly impact tear production or tear film stability, leading to dry eye. This can manifest as a sudden onset of dryness or exacerbate existing conditions. Careful consideration of the medications you’re taking is important when dealing with sudden dry eye.
- Antihistamines: These medications, commonly used for allergies, can reduce tear production by decreasing the flow of aqueous fluid in the eye. This effect can be pronounced in some individuals, leading to a rapid onset of dry eye symptoms.
- Decongestants: Similar to antihistamines, decongestants can also diminish tear production by reducing blood flow to the eye. This can be a temporary side effect but can be persistent in certain cases.
- Diuretics: These medications, often used to treat high blood pressure, can lead to dehydration throughout the body, including the eyes. Reduced tear production is a potential side effect, especially with prolonged use.
- Antidepressants: Some types of antidepressants, particularly those affecting the nervous system, have been reported to contribute to dry eye. The exact mechanism is still being investigated, but a potential link to decreased tear production exists.
- Anticholinergics: These medications, used to treat various conditions, can impact the glands that produce tears. The reduction in tear production can lead to a significant degree of dryness.
- Certain Eye Drops: While many eye drops are designed to alleviate dry eye, some specific types can have the opposite effect, temporarily increasing dryness. This is especially true of drops containing certain preservatives or high concentrations of active ingredients.
Mechanisms of Action and Comparison
The mechanisms by which different medications affect tear production vary. Antihistamines and decongestants, for instance, often work by reducing the activity of the autonomic nervous system, which can impact the flow of aqueous fluid in the eye. Diuretics, on the other hand, can lead to systemic dehydration, impacting the overall hydration of the eye tissues. Anticholinergics directly affect the glands responsible for tear production.
Treatments and Dry Eye
While treatments are often used to alleviate dry eye, certain approaches can paradoxically increase dryness. For example, some eye drops, particularly those containing high concentrations of preservatives, can disrupt the tear film’s natural balance, leading to temporary or prolonged dryness.
Identifying Temporary Dryness-Inducing Eye Treatments
Some eye drops, while intended to treat dry eye, may temporarily worsen the condition. This is particularly true of certain preservative-containing drops. The preservative components can irritate the eye and disrupt the delicate tear film, causing a temporary increase in dryness. Furthermore, some high-concentration active ingredient drops can have a similar effect, albeit in a different way.
Sudden dry eyes can be a real pain, often linked to environmental factors or even certain medications. Sometimes, a sore throat or tonsillitis can be a contributing factor, and if you’re looking for natural ways to ease that discomfort, checking out some home remedies for tonsillitis might be helpful. home remedies for tonsillitis However, it’s still important to consider other potential causes of dry eyes, like changes in humidity or even a reaction to something you’ve eaten.
So, keep an eye out for those triggers!
Table: Medications Commonly Associated with Dry Eye
| Medication Category | Example Medications | Potential Effect on Dry Eye |
|---|---|---|
| Antihistamines | Fexofenadine, Cetirizine | Potential reduction in tear production |
| Decongestants | Phenylephrine, Pseudoephedrine | Potential reduction in tear production |
| Diuretics | Hydrochlorothiazide, Furosemide | Potential dehydration, leading to dry eye |
| Antidepressants | Selective Serotonin Reuptake Inhibitors (SSRIs) | Potential impact on tear production (varies by medication) |
| Anticholinergics | Atropine, Scopolamine | Significant reduction in tear production |
| Eye Drops (Specific Types) | Drops with high preservative content | Temporary or prolonged increase in dryness |
Sudden Dry Eye Causes: What Causes Dry Eyes All Of A Sudden
Sudden dry eye, characterized by a burning, gritty sensation and discomfort, can be triggered by a variety of factors. While underlying medical conditions are a significant cause, lifestyle choices and habits also play a crucial role in the development and exacerbation of this condition. Understanding these factors can empower individuals to take proactive steps towards managing and preventing dry eye.
Lifestyle Factors Contributing to Sudden Dry Eye
Lifestyle factors, often overlooked, can significantly impact tear production and tear film stability, leading to sudden dry eye episodes. Sleep deprivation, stress, and dietary habits are key culprits. These factors can disrupt the delicate balance required for healthy tear function.
Sleep Deprivation and Dry Eye
Insufficient sleep disrupts the body’s natural processes, including those responsible for tear production. Lack of adequate rest can lead to reduced tear production, resulting in a compromised tear film. This, in turn, makes the eyes more susceptible to dryness. For instance, someone who consistently gets less than 7 hours of sleep per night may experience more frequent and intense dry eye symptoms.
Stress and Dry Eye
Chronic stress can trigger a cascade of physiological responses, including reduced tear production. The body’s stress response system diverts resources away from non-essential functions, including tear production. Prolonged stress can lead to persistent dry eye, requiring management strategies to reduce stress levels. Individuals experiencing high levels of stress, such as those in demanding jobs or facing personal challenges, might find that their eyes are more susceptible to dryness.
Dietary Habits and Tear Production
Nutritional deficiencies and imbalances in dietary habits can influence tear production and tear film stability. A diet lacking essential nutrients, such as vitamins A, C, and D, can negatively impact tear health. A diet rich in omega-3 fatty acids, on the other hand, is associated with improved tear film stability. For example, someone following a strict vegan diet might need to supplement with vitamin B12 to maintain adequate tear production.
Excessive Screen Time and Dry Eye
Prolonged use of electronic devices, including computers, tablets, and smartphones, can lead to a condition called digital eye strain, a major contributor to dry eye. Frequent blinking is reduced during extended screen time, allowing the tear film to evaporate more quickly. This can result in a significant increase in dry eye symptoms. Students or professionals spending several hours daily on screens are more prone to dry eye than those who use screens less frequently.
Sudden dry eyes can be a real pain, and sometimes it’s linked to other health issues. For example, if you’re experiencing dizziness when lying down, it could be related to some underlying conditions. This could be a symptom of an underlying condition affecting the inner ear or even the circulatory system. Dizziness when lying down is something you should discuss with a doctor to rule out more serious causes.
So, while dry eyes can sometimes be a simple matter of not producing enough tears, it’s worth considering other factors if they’re persistent or accompanied by other symptoms.
Table: Lifestyle Choices and Dry Eye
| Lifestyle Choice | Potential Relationship with Dry Eye |
|---|---|
| Sleep Deprivation | Reduced tear production, compromised tear film |
| Chronic Stress | Reduced tear production, increased susceptibility to dry eye |
| Nutrient-deficient diet | Impaired tear film stability, reduced tear production |
| Diet rich in omega-3 fatty acids | Improved tear film stability, potentially reduced dry eye |
| Excessive screen time | Reduced blinking rate, tear evaporation, increased dry eye |
Sudden Dry Eye Causes: What Causes Dry Eyes All Of A Sudden
Sudden dry eye can be a frustrating and uncomfortable experience, disrupting daily activities. Understanding the potential causes, especially those related to eyelid and tear gland function, is crucial for effective management. While various factors contribute to this condition, issues with the eyelids and tear glands are significant culprits.Eyelid and tear gland dysfunction can disrupt the delicate balance of the tear film, leading to dry eye.
Proper tear production and distribution rely on a complex interplay between these structures. This section delves into the specific roles of the eyelids and tear glands in maintaining a healthy tear film, examines common eyelid conditions that can disrupt this balance, and explores diagnostic methods used to identify the cause of sudden dry eye.
Eyelid Anatomy and Tear Film Maintenance
The eyelids and tear glands work in concert to produce, distribute, and maintain the tear film, a crucial protective layer for the eye’s surface. The eyelids, acting as a shield, protect the eye from external irritants and help distribute tears across the cornea. The tear glands, situated above the upper eyelid, produce the initial tears that lubricate and nourish the eye’s surface.
Meibomian glands within the eyelids produce lipids that form the oily layer of the tear film, preventing evaporation and maintaining tear film stability.
Sudden dry eyes can be a real pain, and it’s often tricky to pinpoint the exact cause. Sometimes, it’s related to changes in your lifestyle, like stress or lack of sleep. Interestingly, your body mass index (BMI) body mass index bmi might also play a role, as certain health conditions linked to BMI can indirectly affect tear production.
Regardless of the reason, it’s always best to see a doctor to rule out any serious underlying issues.
Eyelid Conditions and Dry Eye
Several eyelid conditions can disrupt tear production and cause dry eye. Blepharitis, an inflammation of the eyelid margins, is a frequent culprit. It can cause redness, scaling, and itching, and can also interfere with the function of the meibomian glands. Meibomian gland dysfunction (MGD) is another significant contributor to dry eye. These glands produce the oily component of the tear film, and dysfunction can lead to an unstable tear film, increasing evaporation and resulting in dry eye symptoms.
Tear Gland Dysfunction and Sudden Dry Eye
The tear glands, or lacrimal glands, play a vital role in producing the aqueous component of the tear film. Sudden dryness could arise from various issues affecting these glands. Conditions like Sjögren’s syndrome, an autoimmune disorder, can significantly impair tear production, leading to sudden and severe dry eye. Certain medications, such as antihistamines or diuretics, can also reduce tear production.
Furthermore, trauma or surgery affecting the tear glands can disrupt their function and lead to sudden dry eye.
Diagnostic Tests for Eyelid and Tear Gland Function
Several diagnostic tests can help evaluate eyelid and tear gland function in patients experiencing sudden dry eye. These include:
- Lid margin examination: A physical examination of the eyelids to identify signs of inflammation, scaling, or other abnormalities.
- Meibography: A specialized imaging technique that allows visualization of the meibomian gland structures and their secretions. This can help assess the quality and quantity of meibomian oil.
- Tear film break-up time (BUT) test: Measures the stability of the tear film by observing how long it takes for the tear film to break up. A short BUT suggests a less stable tear film.
- Schirmer’s test: A simple test that measures tear production by measuring the amount of tears produced by the tear glands in response to stimulation.
These tests, along with patient history and symptoms, provide valuable information for accurate diagnosis and effective treatment planning.
Comparison of Eyelid Conditions and Tear Film Impact
| Eyelid Condition | Impact on Tear Film | Symptoms |
|---|---|---|
| Blepharitis | Inflammation of the eyelid margins, potentially affecting meibomian gland function, leading to unstable tear film. | Redness, scaling, itching, burning, and foreign body sensation. |
| Meibomian Gland Dysfunction (MGD) | Disruption of meibomian gland function, resulting in inadequate oil production, unstable tear film, and increased evaporation. | Burning, stinging, grittiness, and blurred vision. |
| Sjögren’s Syndrome | Autoimmune disorder impacting tear and saliva production. | Dry eyes, dry mouth, fatigue, and joint pain. |
Sudden Dry Eye Causes: Systemic Conditions
Sudden dry eye isn’t always a localized problem. Sometimes, underlying systemic conditions can disrupt the delicate balance of tear production, leading to uncomfortable and persistent dryness. Understanding these connections is crucial for proper diagnosis and treatment. This section will explore systemic diseases that can impact tear production, explaining their relationship with dry eye and common symptoms.Systemic conditions can profoundly affect tear production, disrupting the delicate mechanisms that maintain a healthy tear film.
These conditions often impact various bodily functions, and the effects on tear production are a consequence of these wider systemic changes.
Systemic Diseases Affecting Tear Production
Many systemic diseases can impact the body’s ability to produce adequate tears, leading to dry eye symptoms. These conditions often affect multiple organ systems, and the impact on tear production is a part of a broader picture of systemic dysfunction.
- Autoimmune Diseases: Autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues, can affect tear production in several ways. Conditions like rheumatoid arthritis, lupus, and Sjögren’s syndrome are particularly relevant. These diseases can cause inflammation in the lacrimal glands, which produce tears. The inflammation can impair the glands’ function, leading to decreased tear production and increased tear evaporation.
Common symptoms of these autoimmune diseases, beyond dry eyes, can include joint pain, fatigue, and skin rashes.
- Diabetes Mellitus: Diabetes, a metabolic disorder characterized by high blood sugar levels, can impact various bodily functions, including tear production. High blood sugar levels can damage blood vessels, affecting the delivery of nutrients to the lacrimal glands. This can lead to reduced tear production and impaired tear quality. Symptoms of diabetes, which might accompany dry eyes, include frequent urination, increased thirst, and blurred vision.
- Thyroid Disorders: Hypothyroidism and hyperthyroidism, disorders affecting the thyroid gland, can also influence tear production. These conditions can affect the overall metabolic rate of the body, potentially impacting the functioning of the lacrimal glands. The changes in metabolic rate can cause altered tear production. Hypothyroidism may present with fatigue, weight gain, and cold intolerance, while hyperthyroidism may cause weight loss, nervousness, and heat intolerance.
- Medications: Certain medications can have a side effect of reducing tear production. Examples include some antihistamines, decongestants, and antidepressants. This is not an exhaustive list, and patients should always consult their doctor about potential medication-related dry eye. If you experience dry eyes while taking a medication, discussing this with your physician is essential to explore possible alternatives or adjustments.
- Nutritional Deficiencies: Nutritional deficiencies, particularly in vitamins and minerals, can indirectly impact tear production by affecting overall health and bodily functions. Proper nutrition is vital for healthy tear production, and deficiencies can lead to a decrease in the quality and quantity of tears. A balanced diet is essential for maintaining healthy tear production, and deficiencies in essential nutrients can lead to an overall decline in well-being.
The Impact on the Tear Film
Systemic conditions can affect the tear film in various ways, contributing to dry eye symptoms. The tear film is a complex structure with three layers: the oily outer layer, the watery middle layer, and the mucous inner layer. Disruptions in any of these layers can lead to dryness. For instance, in autoimmune diseases, inflammation can directly damage the lacrimal glands, reducing the production of the watery layer.
In diabetes, high blood sugar levels can cause blood vessel damage, affecting the delivery of nutrients to the tear film components.
Sudden Dry Eye Causes: What Causes Dry Eyes All Of A Sudden
Sudden onset dry eye can be a frustrating and uncomfortable experience. While various factors can contribute to this condition, certain injuries and procedures can disrupt the delicate balance of the tear film, leading to dryness. Understanding these causes can help in preventative measures and appropriate treatment.Eye injuries and surgical procedures can directly or indirectly affect the tear film, leading to dry eye.
The delicate interplay of glands, nerves, and structures in the eye is crucial for maintaining healthy tear production and distribution. Disruptions to this balance can manifest as sudden dryness, making prompt diagnosis and intervention essential.
Eye Injuries and Their Impact on Tear Production
Eye injuries, ranging from minor abrasions to more severe trauma, can disrupt the normal functioning of the tear film. Damage to the ocular surface, including the conjunctiva and cornea, can impair the ability of these structures to produce and distribute tears effectively. The body’s response to injury often involves inflammation, which can further exacerbate the dryness. The inflammation can interfere with the normal functioning of the meibomian glands, leading to decreased oil production, a critical component of the tear film.
Impact of Eye Procedures on Tear Film Stability
Various eye procedures, even seemingly minor ones, can have a significant impact on tear film stability and function. Surgical interventions can damage or alter the delicate structures involved in tear production, distribution, and drainage. These disruptions can manifest as dry eye, sometimes with immediate onset, or gradually over time as the body’s healing process progresses.
Examples of Surgical Procedures Causing Dry Eye
Several eye procedures can contribute to dry eye. For example, cataract surgery, laser refractive surgery (LASIK, PRK, SMILE), and glaucoma procedures can disrupt the delicate balance of the tear film. Post-operative inflammation and changes in the corneal surface can lead to insufficient tear production and altered tear film composition. The use of intraocular lenses (IOLs) in cataract surgery can also influence tear film function.
Mechanisms Linking Injuries and Procedures to Dry Eye
The mechanisms linking injuries and procedures to dry eye are multifaceted. Physical damage to the ocular surface from injuries can lead to inflammation, reduced tear production, and alterations in tear composition. Surgical procedures, through direct manipulation or the introduction of foreign materials, can alter the delicate balance of the tear film components. Furthermore, the body’s immune response to the injury or procedure can further contribute to the development of dry eye.
For instance, the immune response can lead to a disruption in the meibomian gland function, thereby impacting the lipid layer of the tear film.
The Body’s Response to Eye Injuries and Its Effect on Tear Production
The body’s response to eye injuries involves a complex interplay of inflammatory and healing mechanisms. Following an injury, the body activates its inflammatory response to protect the damaged tissue. This inflammatory response can lead to increased vascular permeability, which may temporarily increase tear production, but ultimately can cause edema and discomfort, which in turn can negatively impact tear film production and distribution.
The healing process, while essential for tissue repair, can sometimes involve the temporary alteration of the tear film composition, leading to dryness.
Closure
In conclusion, understanding what causes dry eyes all of a sudden requires a multifaceted approach. It’s not always a simple answer, and the underlying cause can vary greatly. By considering medical conditions, environmental factors, medications, lifestyle choices, and eyelid/tear gland issues, you can gain a clearer picture of the potential triggers. Remember, if you experience persistent or worsening dry eye, consulting an eye care professional is crucial for proper diagnosis and personalized treatment.




