Ulcerative colitis causes and risk factors are complex, but understanding them is crucial for those affected and those seeking to learn more. This exploration delves into the potential triggers, from genetic predispositions to environmental influences, immune system dysfunction, and even infections. We’ll examine how these factors may contribute to the development of this chronic inflammatory condition.
From genetics to environmental factors, this blog post will cover a range of potential contributors to ulcerative colitis, including the roles of diet, lifestyle, and geography. We’ll also explore the role of the immune system, infections, and medications in increasing the risk of this inflammatory condition. Finally, we’ll touch on diagnostic procedures and preventive measures to manage potential risks.
Introduction to Ulcerative Colitis

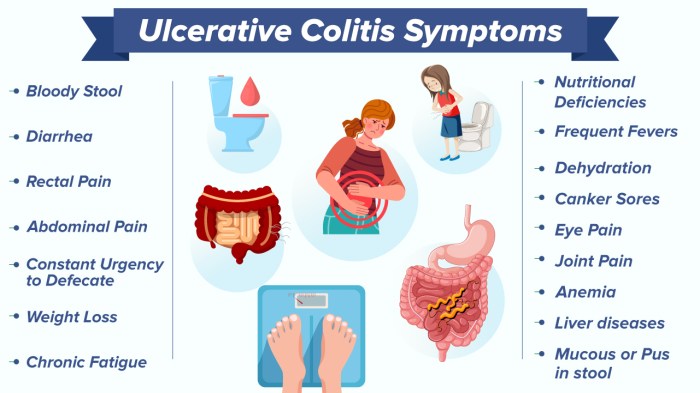
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Characterized by inflammation and ulcers in the lining of the large intestine, it can cause significant discomfort and complications if left untreated. Understanding the various forms and characteristics of ulcerative colitis is crucial for effective diagnosis and management.This condition is often debilitating, impacting a person’s quality of life due to the recurring symptoms and potential long-term consequences.
While the exact cause remains unknown, a combination of genetic predisposition, environmental factors, and immune system dysfunction are thought to contribute to its development.
Types of Ulcerative Colitis
Ulcerative colitis can manifest in different forms, each with varying degrees of severity and location of inflammation. Recognizing these variations is vital for tailored treatment approaches.
| Type | Description | Characteristics |
|---|---|---|
| Pancolitis | Inflammation affecting the entire colon. | Characterized by symptoms throughout the entire large intestine. This is often the most severe form. |
| Left-sided colitis | Inflammation limited to the descending colon, sigmoid colon, and rectum. | Symptoms typically concentrate in the lower part of the colon, with less severe symptoms compared to pancolitis. |
| Proctitis | Inflammation confined to the rectum. | The least severe form, primarily affecting the lower part of the large intestine. Symptoms are typically localized to the rectum. |
| Distal colitis | Inflammation that extends from the rectum to a portion of the colon. | Symptoms are present in the rectum and a portion of the colon. The level of inflammation and symptoms are typically between proctitis and left-sided colitis. |
Prevalence and Demographics
Ulcerative colitis affects individuals of all ages, but it typically presents in young adulthood, often between the ages of 15 and 30. It’s also observed in later life, though less frequently. While the exact prevalence varies geographically, estimates suggest that it affects approximately 1-2% of the global population. The disease shows no clear preference for any particular gender.
Understanding ulcerative colitis involves looking at various causes and risk factors. While the exact reasons are still somewhat a mystery, a connection to certain dietary factors and gut health is suspected. Interestingly, sometimes digestive issues like diarrhea can be related to other conditions, such as kidney stones, as discussed in detail in this helpful article on kidney stones and diarrhea.
Regardless of the underlying cause, it’s essential to keep in mind that ulcerative colitis can manifest in different ways, impacting each individual uniquely, and requiring careful monitoring and treatment.
Genetic Predisposition
Ulcerative colitis, a chronic inflammatory bowel disease, isn’t solely determined by environmental factors. Genetic predisposition plays a significant role in its development, increasing the likelihood of individuals inheriting the susceptibility to the condition. Understanding the genetic underpinnings is crucial for identifying individuals at risk and potentially developing personalized treatment strategies.A complex interplay of genes contributes to the development of ulcerative colitis.
These genes influence the immune system’s response to gut bacteria, the integrity of the intestinal lining, and other crucial processes. While a single gene may not be the sole cause, the cumulative effect of multiple genetic variations can significantly increase the risk.
Genes Associated with Increased Risk
Several genes have been linked to an elevated risk of ulcerative colitis. These genes often regulate immune responses, inflammation, and repair mechanisms within the gut. Variations in these genes can make individuals more susceptible to the inflammatory cascade characteristic of the disease. For example, mutations in genes involved in DNA repair can increase the likelihood of developing the condition.
Genetic Factors in Different Populations
The prevalence and specific genetic risk factors associated with ulcerative colitis can vary among different populations. Research indicates that certain genetic variants may be more common in particular ethnic groups. This variation highlights the complex interplay between genetics and environmental factors in disease development. Studies have shown that the frequency of specific gene variants linked to ulcerative colitis varies considerably between populations.
For example, certain gene variants may be more prevalent in individuals of European descent compared to those of Asian descent. This disparity underscores the importance of considering population-specific genetic factors when studying and treating ulcerative colitis.
Inheritance Patterns
The inheritance patterns of ulcerative colitis-related genes are complex and not fully understood. A family history of ulcerative colitis significantly increases the risk of developing the condition. However, the inheritance pattern isn’t always straightforward, and a clear-cut “inheritance pattern” is not established. Instead, a combination of genetic and environmental factors likely determines the individual’s susceptibility.
| Gene | Inheritance Pattern | Description |
|---|---|---|
| NOD2 | Autosomal recessive | Plays a critical role in the immune response, influencing how the body interacts with bacteria in the gut. |
| ATG16L1 | Complex | Impacts autophagy, a cellular process involved in waste removal and immune regulation. Variations in this gene can affect the efficiency of autophagy in the gut. |
| IL23R | Autosomal dominant | This gene is part of the immune response system. Variations may lead to an overactive immune response in the gut, contributing to inflammation. |
The table above illustrates some key genes linked to ulcerative colitis, along with their inheritance patterns. It’s crucial to remember that these are only a few examples, and many other genes are likely involved in the complex interplay leading to the disease. Understanding these patterns helps predict the likelihood of individuals inheriting the susceptibility.
Environmental Factors
Beyond genetics, environmental factors play a significant role in the development of ulcerative colitis. Understanding these factors can help us identify potential triggers and modifiable risk factors, potentially leading to better preventative measures. While the exact mechanisms aren’t fully understood, research suggests environmental exposures can influence the immune system’s response and potentially increase susceptibility to the disease.
Dietary Influences
Dietary habits have been linked to ulcerative colitis risk. Certain foods and dietary patterns might trigger inflammation in the gut or affect the gut microbiome, which plays a crucial role in maintaining gut health. This includes the type and amount of fiber consumed, as well as the presence of processed foods and potential food sensitivities. A balanced and varied diet is likely to be beneficial, although precise dietary recommendations are still being researched.
- Fiber Intake: High-fiber diets are often associated with a reduced risk of inflammatory bowel diseases. Soluble fiber can promote a healthier gut microbiome by feeding beneficial bacteria. Conversely, an extremely high-fiber intake might lead to digestive discomfort in some individuals.
- Processed Foods and Additives: The consumption of processed foods and artificial additives might contribute to gut inflammation and potentially exacerbate ulcerative colitis symptoms. A diet rich in whole foods, rather than highly processed options, is generally recommended for overall gut health.
- Food Sensitivities: Certain individuals might have sensitivities to specific foods, leading to inflammation in the gut. Dairy products, gluten, and certain fruits or vegetables are examples of potential triggers that might affect individuals differently.
Lifestyle Factors
Lifestyle choices, such as smoking and stress levels, might influence the risk of developing ulcerative colitis. Stress, in particular, can significantly impact the immune system, potentially contributing to inflammation. While not definitive, maintaining a healthy lifestyle that includes stress management and regular exercise might help mitigate risk factors.
- Smoking: Smoking is linked to a higher risk of developing and worsening ulcerative colitis. Nicotine and other substances in tobacco smoke can induce inflammation in the gut and potentially impair the immune response. Smoking cessation is generally advised for individuals with ulcerative colitis.
- Stress: Chronic stress can significantly impact the immune system and may worsen ulcerative colitis symptoms. Managing stress through relaxation techniques, mindfulness, or exercise could be beneficial for individuals with the condition.
- Exercise: Regular physical activity can promote overall health and potentially have a positive impact on gut health. Moderate-intensity exercise, such as brisk walking or jogging, could be beneficial in managing stress and maintaining a healthy weight.
Geographic Location
Geographic location has been linked to ulcerative colitis prevalence. Variations in environmental exposures, including microbial communities and dietary patterns, might account for these differences. For instance, some regions have higher rates of ulcerative colitis compared to others, highlighting the potential role of environmental factors in disease development.
- Microbial Communities: Variations in microbial communities, particularly in the gut microbiome, might contribute to variations in ulcerative colitis prevalence across different geographic locations. Exposure to diverse microbial communities might influence the development of a balanced and healthy gut microbiome.
- Dietary Patterns: Regional dietary patterns, such as the amount and type of fiber consumed, or the presence of specific food components, might play a role in the prevalence of ulcerative colitis in different areas. Dietary diversity and patterns vary greatly across different regions, impacting the gut microbiome composition.
Comparison of Environmental Exposures
| Environmental Exposure | Potential Impact on Ulcerative Colitis | Further Research Needed |
|---|---|---|
| High-Fiber Diet | Potential reduction in risk through a healthier gut microbiome. | Investigate specific types and amounts of fiber for optimal benefit. |
| Processed Foods | Potential increase in risk through inflammation and gut dysbiosis. | Examine the impact of specific additives and processing methods. |
| Smoking | Increased risk due to inflammation and immune system dysfunction. | Study the long-term effects of smoking cessation on ulcerative colitis. |
| Chronic Stress | Potential worsening of symptoms due to immune system dysregulation. | Investigate the precise mechanisms linking stress and inflammation. |
| Geographic Location | Variation in prevalence linked to microbial communities and dietary patterns. | Analyze the unique microbial and dietary components of different regions. |
Immune System Dysfunction
The human immune system, a complex network of cells and molecules, plays a crucial role in protecting the body from harmful invaders. However, in ulcerative colitis, this system appears to malfunction, leading to an inappropriate and persistent inflammatory response within the digestive tract. This malfunctioning immune response is a key contributor to the disease’s development and progression.The immune system, in its normal function, distinguishes between harmful invaders and the body’s own tissues.
In ulcerative colitis, this crucial distinction seems to break down. The immune system mistakenly identifies normal components of the gut lining as threats, triggering an inflammatory cascade. This chronic inflammation is the hallmark of the disease, and the nature of the inflammatory response varies depending on the individual.
Immune Cell Involvement in Inflammation
The inflammatory process in ulcerative colitis is characterized by the infiltration of various immune cells into the colon. These cells, each with specific roles, work together to amplify the inflammatory response. The process isn’t a simple one-way street; rather, it’s a complex interplay between different types of cells and signaling molecules.
- Lymphocytes: A critical component of the immune system, lymphocytes, including T cells and B cells, are a central player in the inflammatory response. T cells, particularly T helper cells (Th1 and Th17), release cytokines, signaling molecules that further activate the inflammatory cascade. B cells produce antibodies that can also contribute to the inflammatory response.
- Macrophages: These cells are crucial in clearing cellular debris and pathogens. However, in ulcerative colitis, macrophages become activated and release inflammatory mediators, exacerbating the inflammatory process. This continuous activation and release of inflammatory substances create a cycle that perpetuates the damage to the gut lining.
- Neutrophils: These cells are the first responders to inflammation, rapidly migrating to the affected area. They release enzymes and other substances that contribute to tissue damage, which in turn can exacerbate the inflammatory response. The presence of high numbers of neutrophils in the colon tissue is often indicative of active inflammation in ulcerative colitis.
Mechanisms of Immune System Dysfunction
Several mechanisms are thought to contribute to the immune system’s malfunction in ulcerative colitis.
- Dysregulated Cytokine Production: Cytokines, signaling molecules, play a critical role in regulating the immune response. In ulcerative colitis, there is often an imbalance in cytokine production, with increased levels of pro-inflammatory cytokines like TNF-α and IL-1β. This imbalance contributes to the chronic inflammation seen in the disease.
- Genetic Susceptibility: Certain genetic variations may predispose individuals to an overactive immune response. These genetic predispositions can influence how the immune system reacts to various stimuli within the gut. For example, specific genes associated with immune function are known to increase the risk of developing ulcerative colitis.
- Gut Microbiota Imbalance: The gut microbiota, the collection of microorganisms residing in the gut, plays a role in regulating the immune system. In ulcerative colitis, there is often a disruption in the balance of the gut microbiota. This imbalance can lead to the immune system reacting inappropriately to commensal bacteria, exacerbating inflammation. One example is the presence of certain bacterial species that stimulate an excessive inflammatory response.
Inflammatory Processes in the Gut
The inflammatory processes in ulcerative colitis primarily affect the colon and rectum. These processes result in damage to the colon’s lining, characterized by inflammation, ulceration, and bleeding.
- Inflammation: The inflammatory response is characterized by the accumulation of immune cells and the release of inflammatory mediators. This process leads to the characteristic symptoms of ulcerative colitis, such as abdominal pain, diarrhea, and rectal bleeding.
- Ulceration: The inflammatory process can cause damage to the colon’s lining, leading to the formation of ulcers. These ulcers disrupt the normal structure of the gut and contribute to the symptoms of the disease.
- Bleeding: The ulcerations in the colon can cause bleeding, leading to blood in the stool. This bleeding is a significant symptom that often indicates the severity of the disease.
Infections and Ulcerative Colitis: Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis, a chronic inflammatory bowel disease, is a complex condition with multiple contributing factors. While genetic predisposition and environmental triggers play significant roles, the interplay between the gut’s microbial community and infection is another crucial aspect. Understanding how infections might influence the disease process is essential for developing better preventative and therapeutic strategies.Infections, though not the sole cause, can act as potential triggers or exacerbators of ulcerative colitis.
The intricate relationship between the gut’s microbiome and the immune system makes infections a key consideration. Changes in the balance of beneficial and harmful bacteria can disrupt the gut’s delicate equilibrium, leading to inflammation and disease progression.
Potential Infectious Agents
Several infectious agents have been implicated in the development or exacerbation of ulcerative colitis. These include a wide range of bacteria, viruses, and parasites, each with the potential to disrupt the gut’s normal functioning. The exact mechanisms through which these infections contribute to the disease remain under investigation.
Relationship Between Gut Microbiome and Ulcerative Colitis
The gut microbiome, a complex ecosystem of bacteria, fungi, and viruses, plays a vital role in maintaining gut health. Dysbiosis, an imbalance in the microbial community, is increasingly recognized as a contributing factor to various inflammatory conditions, including ulcerative colitis. Infectious agents can disrupt this balance, leading to a shift in the composition of the gut microbiome. This alteration can trigger an inflammatory response and contribute to the development or worsening of ulcerative colitis.
Examples of Infectious Agents
Various bacterial, viral, and parasitic infections have been linked to ulcerative colitis. These include:
- Salmonella: Certain strains of Salmonella bacteria are known to cause gastroenteritis, which can lead to inflammation in the digestive tract and potentially trigger or worsen colitis symptoms.
- Campylobacter: Campylobacter infections are often associated with diarrhea and abdominal pain. There’s evidence suggesting a link between these infections and the development of inflammatory bowel diseases, including ulcerative colitis.
- Clostridium difficile: This bacterium is a significant cause of antibiotic-associated diarrhea and colitis. Its toxins can disrupt the gut’s lining and contribute to the inflammation characteristic of ulcerative colitis.
- Yersinia enterocolitica: Infections with this bacterium can mimic ulcerative colitis symptoms, causing abdominal pain, diarrhea, and fever. In some cases, Yersinia infections have been linked to the development or worsening of ulcerative colitis.
- Viral infections, such as cytomegalovirus (CMV) and herpes simplex virus, have also been associated with inflammatory bowel disease. These infections can trigger an inflammatory response and alter the gut microbiome composition.
- Parasitic infections, like Giardia, can lead to intestinal inflammation and diarrhea, potentially influencing the development or worsening of colitis.
Table: Potential Links Between Infectious Agents and Ulcerative Colitis
| Infectious Agent | Potential Link to Ulcerative Colitis |
|---|---|
| Salmonella | Can cause gastroenteritis, potentially triggering or exacerbating colitis. |
| Campylobacter | Associated with diarrhea and abdominal pain; potential link to inflammatory bowel diseases. |
| Clostridium difficile | Causes antibiotic-associated diarrhea and colitis; toxins disrupt gut lining. |
| Yersinia enterocolitica | Can mimic colitis symptoms; potential link to development or worsening of colitis. |
| Viruses (e.g., CMV, HSV) | Can trigger an inflammatory response and alter gut microbiome. |
| Parasites (e.g., Giardia) | Cause intestinal inflammation and diarrhea; potential impact on colitis. |
Medication and Ulcerative Colitis
Certain medications and drug exposures can potentially increase the risk of developing ulcerative colitis or exacerbate existing symptoms. Understanding these potential connections is crucial for both prevention and effective management of the condition. This section delves into the relationship between specific medications and ulcerative colitis, exploring the impact on gut health and potential interactions.Medication use is a complex factor in many health conditions, and ulcerative colitis is no exception.
While many medications are generally safe, some can trigger or worsen inflammatory responses in the gut, leading to complications for individuals with ulcerative colitis. This can be due to direct effects on the gut lining, interactions with existing immune responses, or other factors.
Potential Medications Associated with Increased Risk
Certain medications may increase the risk of developing ulcerative colitis or worsen its symptoms. While not a definitive cause in all cases, there are recognized links. The specific mechanisms through which these medications impact gut health are still being investigated, but some potential pathways are known.
Ulcerative colitis, a chronic inflammatory condition, has various potential causes and risk factors. While the exact causes remain somewhat elusive, genetics, environmental triggers, and the gut microbiome are all thought to play a role. Interestingly, stress and lifestyle choices can also be contributing factors. For instance, are you experiencing headaches from long hours at your computer?
This can lead to increased stress and affect your overall well-being, potentially impacting the gut. It’s important to consider the connection between stress, diet, and other factors when looking into ulcerative colitis causes and risk factors. is working at my computer causing my headaches
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, are commonly used for pain relief. Their potential to irritate the gastrointestinal tract, including the colon, can exacerbate inflammation in individuals predisposed to ulcerative colitis. Long-term use or high doses of NSAIDs may increase the risk.
- Certain antibiotics: Some antibiotics, while crucial for treating bacterial infections, may disrupt the delicate balance of gut microbiota. This imbalance can potentially contribute to inflammation and exacerbate existing ulcerative colitis symptoms in susceptible individuals.
- Anti-inflammatory medications used for other conditions: Some anti-inflammatory medications used to treat other conditions, such as certain autoimmune diseases, might have an indirect effect on the gut. These medications may influence immune responses that could contribute to the development or worsening of ulcerative colitis.
- Immunosuppressants: While immunosuppressants are crucial for treating various conditions, including autoimmune diseases, some of these medications may alter the immune response, potentially increasing susceptibility to inflammation and conditions like ulcerative colitis.
Medication Interactions and Ulcerative Colitis
Interactions between medications can significantly affect the risk or progression of ulcerative colitis. Understanding these interactions is essential for optimizing treatment strategies.
- Drug-drug interactions: Certain medications can interact with each other, either enhancing or diminishing the effects of one or both. For example, combining NSAIDs with certain antibiotics might increase the risk of gastrointestinal side effects, potentially worsening inflammation in individuals with ulcerative colitis.
- Medication-induced changes in gut microbiota: Some medications can alter the composition of gut bacteria. These changes may contribute to increased inflammation and complications for those with ulcerative colitis.
Table of Potential Drug Exposures and Ulcerative Colitis
The following table summarizes the potential relationship between certain drug exposures and ulcerative colitis. It is crucial to note that this is not an exhaustive list and individual responses may vary.
| Potential Drug Exposure | Potential Impact on Ulcerative Colitis | Further Considerations |
|---|---|---|
| NSAIDs | Increased risk of gastrointestinal irritation, potential exacerbation of existing inflammation. | Long-term use and high doses are associated with increased risk. |
| Certain Antibiotics | Disruption of gut microbiota, potential exacerbation of symptoms. | Antibiotic-associated colitis is a known concern. |
| Immunosuppressants | Altered immune response, potential impact on disease activity. | May be beneficial in some cases but carries risks. |
| Anti-inflammatory medications (for other conditions) | Potential indirect impact on gut inflammation, variable effects. | Further research is needed to fully understand the relationship. |
Diagnostic Procedures
Pinpointing ulcerative colitis often involves a multi-step process, combining patient history, physical examination, and various diagnostic tests. Understanding these procedures is crucial for accurate diagnosis and timely treatment. Early and accurate diagnosis is essential for effective management and preventing complications.
Common Diagnostic Methods
Accurate diagnosis of ulcerative colitis relies on a combination of methods. These methods start with a thorough patient history and physical examination, which helps to identify potential risk factors and symptoms. This initial assessment provides a crucial foundation for further investigations.
While the exact causes of ulcerative colitis remain a mystery, certain risk factors are increasingly linked to the condition. Lifestyle choices, like diet and exercise, play a role, but genetics also seem to contribute. Interestingly, some studies suggest a potential connection between certain types of obesity, such as visceral fat accumulation, and an increased risk of developing ulcerative colitis.
Understanding the interplay between different types of obesity and inflammatory bowel diseases like ulcerative colitis is crucial for developing more targeted preventative strategies. More research is needed to fully understand these correlations, however, and ultimately pin down the root causes of ulcerative colitis.
Key Tests to Identify and Differentiate
Several key tests are used to confirm the diagnosis and distinguish ulcerative colitis from other conditions with similar symptoms. These tests help narrow down the possibilities and provide a more precise understanding of the underlying cause. Blood tests, stool tests, and imaging techniques all contribute to the diagnostic process.
Endoscopic Procedures
Endoscopic procedures play a critical role in visualizing the colon and rectum. These procedures allow healthcare professionals to directly observe the affected areas and assess the extent and severity of inflammation. They are essential for confirming the diagnosis and evaluating the disease activity.
Summary of Endoscopic Procedures
- Colonoscopy: A colonoscopy involves inserting a flexible tube with a camera (endoscope) into the rectum and colon. This allows visualization of the entire colon, enabling detailed examination of the lining and identification of any abnormalities, such as inflammation, ulcers, or polyps. Biopsies can be taken during the procedure to confirm the diagnosis and assess the severity of the condition.
- Sigmoidoscopy: A sigmoidoscopy is a less extensive procedure focusing on the sigmoid colon, the lower part of the large intestine. It is often used as a preliminary test if a colonoscopy is not immediately accessible. If the inflammation appears limited to this region, a sigmoidoscopy may be sufficient for diagnosis.
Diagnostic Tests and Associated Procedures
| Diagnostic Test | Procedure Description | Purpose |
|---|---|---|
| Complete Blood Count (CBC) | Measures various components of the blood, including red blood cells, white blood cells, and platelets. | Helps identify anemia, infection, or other systemic issues that might accompany ulcerative colitis. |
| Stool Tests | Analyze stool samples for the presence of blood, white blood cells, or other abnormalities. | Helps identify signs of inflammation or bleeding within the colon, indicative of potential inflammatory bowel disease. |
| Colonoscopy | Visual examination of the colon using a flexible endoscope. | Provides direct visualization of the colon lining, allowing identification of inflammation, ulcers, and other lesions. Biopsies can be taken for further analysis. |
| Sigmoidoscopy | Visual examination of the lower part of the colon (sigmoid colon) using a flexible endoscope. | Useful for initial assessment if colonoscopy is not immediately available. Can help to confirm localized inflammation. |
| Biopsy | Removal of a small tissue sample for microscopic examination. | Essential for confirming the diagnosis by identifying characteristic histological changes in the colon tissue associated with ulcerative colitis. |
Risk Factors and Prevention
While the precise cause of ulcerative colitis remains elusive, understanding risk factors and implementing preventive strategies can significantly impact disease management. This involves recognizing modifiable lifestyle choices that can potentially reduce the likelihood of developing the condition or lessening its severity. Focusing on a holistic approach, including diet, stress management, and overall well-being, is key to minimizing the risk.Although some risk factors are unavoidable, many lifestyle aspects are controllable.
By making informed decisions and proactively managing potential triggers, individuals can take proactive steps to mitigate their risk. This proactive approach emphasizes empowering individuals with the knowledge and tools to take control of their health and well-being.
Lifestyle Factors and Risk Reduction
Adopting healthy lifestyle habits can play a crucial role in minimizing the risk of developing ulcerative colitis or in mitigating its impact. Maintaining a balanced diet, managing stress levels, and engaging in regular physical activity are all key components of this approach.
- Dietary Recommendations: A balanced diet rich in fruits, vegetables, and whole grains can be beneficial. Reducing processed foods, red meat, and saturated fats might also be helpful. The specific dietary needs of each individual can vary greatly, making it vital to consult with a registered dietitian or healthcare professional to develop a personalized plan.
- Stress Management Techniques: Chronic stress can exacerbate various health conditions, including ulcerative colitis. Incorporating stress-reducing techniques, such as yoga, meditation, or deep breathing exercises, can be valuable in managing stress and potentially minimizing its impact on the disease.
- Regular Physical Activity: Maintaining a regular exercise routine can contribute to overall well-being and potentially influence the immune system’s response. Finding an enjoyable form of physical activity, such as walking, swimming, or cycling, can be a significant part of a healthy lifestyle.
Managing Potential Risk Factors
Identifying and addressing potential risk factors is crucial in reducing the likelihood of developing or worsening ulcerative colitis. This approach is particularly helpful in proactively managing potential triggers and contributing factors.
- Smoking Cessation: Smoking has been linked to an increased risk of developing ulcerative colitis and exacerbating symptoms. Quitting smoking is a significant step towards improving overall health and potentially reducing the risk of developing or worsening the condition.
- Maintaining a Healthy Weight: Maintaining a healthy weight through a balanced diet and regular exercise can have a positive impact on overall health and potentially reduce the risk of developing ulcerative colitis.
- Avoiding Triggers: Identifying specific foods or situations that trigger symptoms is crucial. By avoiding these triggers, individuals can effectively manage symptoms and minimize the risk of flare-ups.
Preventive Measures, Ulcerative colitis causes and risk factors
Preventive measures aim to reduce the likelihood of developing ulcerative colitis. Early detection and intervention are key components of disease management.
- Regular Check-ups: Regular check-ups with a gastroenterologist are essential for early detection and management of potential issues. This proactive approach can help in identifying and addressing potential problems early on, allowing for appropriate interventions and minimizing the severity of the condition.
- Genetic Counseling: If a family history of ulcerative colitis exists, genetic counseling can provide valuable information and support for individuals who may be at increased risk.
End of Discussion
In conclusion, ulcerative colitis causes and risk factors are multifaceted, encompassing genetic, environmental, and immune system elements. Understanding these factors can aid in early detection, risk reduction, and improved management strategies. This comprehensive look at the complexities surrounding ulcerative colitis is a vital step towards a deeper understanding of this condition and its various potential contributors. Further research is always valuable to gain a clearer understanding.