Treatment of ankylosing spondylitis is a multifaceted approach that addresses the diverse needs of those affected. This comprehensive guide delves into the intricacies of diagnosing, managing, and living with this chronic inflammatory condition. We’ll explore everything from the initial diagnosis to long-term management strategies, and the impact on daily life.
The guide covers the spectrum of approaches, from medications and physical therapy to lifestyle modifications and patient support. It provides insights into the progression of the disease, comparing it to similar conditions, and outlining various diagnostic methods. The importance of ongoing research and the evolving treatment landscape will also be discussed.
Overview of Ankylosing Spondylitis
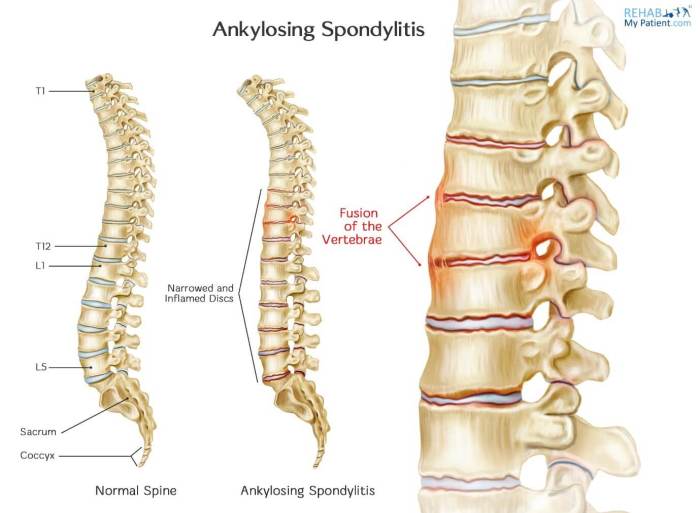
Ankylosing spondylitis (AS) is a chronic inflammatory condition primarily affecting the spine and sacroiliac joints. Characterized by inflammation and stiffness, it can lead to progressive fusion of the spine and other affected areas over time. Understanding its various stages and how it differs from other inflammatory back pain conditions is crucial for effective management.Ankylosing spondylitis typically begins insidiously, often with subtle back pain, stiffness, and limited range of motion, particularly in the morning.
These initial symptoms can be easily dismissed, often mistaken for simple back pain or other musculoskeletal issues. As the disease progresses, the inflammation intensifies, leading to increasing stiffness and pain, often radiating to the hips and other areas. The progressive nature of AS can result in significant structural changes, such as the fusion of vertebrae and reduced spinal mobility.
Definition and Symptoms
Ankylosing spondylitis is a type of spondyloarthritis, characterized by inflammation of the spine and sacroiliac joints. Common symptoms include persistent low back pain, stiffness, and limited range of motion, especially in the morning. Pain often improves with activity but worsens with rest. Other symptoms can include pain in the hips, shoulders, and other areas. These symptoms can fluctuate in severity and duration.
Progression of the Disease
The progression of AS varies from person to person, but generally follows a pattern. Early stages are often marked by subtle symptoms, like intermittent back pain and stiffness. As the disease advances, the pain and stiffness become more persistent and severe. Eventually, the inflammation can cause the bones in the spine to fuse, leading to a loss of spinal flexibility and reduced range of motion.
This fusion can affect other areas of the body, like the hips or chest.
Characteristics of Ankylosing Spondylitis
“Ankylosing spondylitis is a progressive disease, and early diagnosis and treatment are crucial for slowing disease progression and preventing long-term complications.”
Key characteristics include:
- Chronic Inflammation: The underlying inflammatory process is the driving force behind the symptoms and structural changes.
- Axial Involvement: Primarily affects the spine and sacroiliac joints, leading to stiffness and pain in these areas.
- Progressive Nature: The disease tends to progress gradually, with symptoms worsening over time if left untreated.
- Potential for Structural Damage: Inflammation can lead to the fusion of bones in the spine and other affected areas.
- Systemic Manifestations: AS can affect other parts of the body, such as the eyes, heart, and lungs.
Comparison with Other Inflammatory Back Pain Conditions
| Characteristic | Ankylosing Spondylitis | Reactive Arthritis | Psoriatic Arthritis | Enteropathic Arthritis |
|---|---|---|---|---|
| Primary Site of Involvement | Spine and sacroiliac joints | Peripheral joints, often with skin involvement | Peripheral joints, often with skin lesions | Gut-associated, often with gastrointestinal issues |
| Typical Symptoms | Low back pain, stiffness, limited range of motion | Pain and swelling in joints, especially the lower extremities, skin manifestations | Joint pain, swelling, skin psoriasis | Joint pain, often accompanied by digestive problems |
| Associated Conditions | Uveitis (eye inflammation), aortic insufficiency | Urethritis, conjunctivitis, diarrhea | Psoriasis, skin lesions | Crohn’s disease, ulcerative colitis |
This table provides a concise overview, highlighting key differences. A proper diagnosis requires a comprehensive evaluation by a healthcare professional.
Diagnostic Methods: Treatment Of Ankylosing Spondylitis
Understanding the specific signs and symptoms of ankylosing spondylitis (AS) is crucial for early diagnosis and effective treatment. However, a definitive diagnosis often requires a combination of physical examinations, imaging studies, and blood tests. The diagnostic process aims to identify characteristic patterns that support the suspicion of AS, while also ruling out other conditions with similar presentations.
Common Diagnostic Tests
Various diagnostic tests are employed to confirm a suspicion of ankylosing spondylitis. These methods are instrumental in evaluating the extent and location of inflammation, identifying structural changes, and ruling out other conditions. The combination of these tests helps healthcare providers formulate an accurate diagnosis.
Imaging Techniques, Treatment of ankylosing spondylitis
Imaging plays a vital role in the diagnosis of ankylosing spondylitis. X-rays, MRI scans, and CT scans provide valuable insights into the structural changes associated with the disease.
- X-rays: Early stages of AS may not show significant changes on X-rays. However, as the disease progresses, characteristic findings such as sacroiliitis (inflammation of the sacroiliac joints) and syndesmophytes (new bone growth on the vertebral bodies) become apparent. X-rays are particularly useful for visualizing the sacroiliac joints, where inflammation is frequently observed early in the disease process.
Managing ankylosing spondylitis involves a multifaceted approach, focusing on pain relief and maintaining mobility. While medication plays a crucial role, a healthy diet can also significantly impact the overall well-being of those with the condition, similar to the importance of type 2 diabetes meal planning. This means paying attention to nutrient-rich foods and portion control, all of which ultimately contribute to better symptom management and a more active lifestyle in treating ankylosing spondylitis.
The X-ray images reveal the narrowing of the joint space and bony erosions. These are characteristic findings in AS.
- MRI Scans: MRI scans offer a more detailed view of soft tissues and bone marrow than X-rays. They can detect early inflammation in the sacroiliac joints and spinal ligaments even before structural changes are visible on X-rays. MRI is particularly helpful in evaluating the extent of inflammation throughout the spine and surrounding tissues, providing valuable insights into the disease’s progression and activity.
Furthermore, MRI scans can differentiate between inflammation and other potential causes of back pain.
- CT Scans: CT scans, while less sensitive than MRI in detecting early inflammation, provide high-resolution images of bone structures. This detail is particularly helpful in assessing the extent of bony fusion and ankylosis (stiffening) in the spine. CT scans can be used to further delineate the structural changes that accompany AS, such as bony bridging or fusion of the spine, and provide additional insights into the condition’s severity.
The scans may show narrowing of the intervertebral spaces and calcification of the ligaments.
Blood Tests
Blood tests are used to assess the inflammatory markers in the body. These markers can indicate the presence of inflammation, a key characteristic of ankylosing spondylitis.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP): Elevated levels of ESR and CRP are frequently observed in individuals with active AS. These blood tests provide an indication of the inflammatory process within the body. High levels of these markers suggest ongoing inflammation, which is a hallmark of AS. These tests aid in monitoring the disease activity and response to treatment.
Diagnostic Criteria
Various criteria have been developed to aid in the diagnosis of ankylosing spondylitis. These criteria provide a standardized approach to evaluating patients and establishing a diagnosis.
- Modified New York Criteria: These criteria are frequently used to diagnose AS. They involve assessing various factors, including the duration and location of back pain, the presence of specific symptoms, and the results of physical examinations and imaging studies. The modified New York criteria provide a structured approach to diagnosis, allowing for a more consistent and reliable assessment of patients suspected of having AS.
Imaging Findings in Ankylosing Spondylitis
The following table summarizes the key imaging findings associated with ankylosing spondylitis.
| Imaging Study | Characteristic Findings |
|---|---|
| X-rays | Sacroiliitis (inflammation of the sacroiliac joints), syndesmophytes (new bone growth on the vertebral bodies), narrowing of joint spaces, bony erosions. |
| MRI | Early inflammation in sacroiliac joints and spinal ligaments, soft tissue edema, enthesitis (inflammation at the tendon/ligament attachment points). |
| CT | Bony fusion or bridging of the vertebrae, ankylosis (stiffening) of the spine, narrowing of intervertebral spaces, calcification of ligaments. |
Treatment Approaches

Ankylosing spondylitis, a chronic inflammatory condition affecting the spine and sacroiliac joints, requires a multifaceted approach to management. Effective treatment aims to reduce pain, improve mobility, and slow disease progression. The strategies employed often involve a combination of medications, physical therapy, and, in some cases, surgery.Treatment plans for ankylosing spondylitis are highly personalized and should be developed in close collaboration with a rheumatologist.
Factors like the severity of the disease, individual patient response to therapies, and overall health considerations influence the chosen treatment strategy.
Medication Management
Medication plays a crucial role in managing ankylosing spondylitis. It helps to control inflammation, reduce pain, and potentially slow the progression of the disease. Different classes of medications are utilized, each with its own mechanisms of action and potential side effects.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs like ibuprofen and naproxen are frequently the first-line treatment for ankylosing spondylitis. They effectively reduce pain and inflammation. Their over-the-counter availability makes them accessible, but patients should be mindful of potential gastrointestinal side effects and monitor their use closely.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as methotrexate, are often prescribed when NSAIDs alone are insufficient. They aim to modify the course of the disease and potentially slow the progression of ankylosis (fusion of the spine). DMARDs can have more pronounced side effects, and their use requires careful monitoring and potential adjustments to the treatment plan.
- Biologics: Biologics, a newer class of medications, target specific components of the immune system involved in the inflammatory process. These medications can be highly effective in reducing inflammation and pain, especially in cases where other treatments have not been sufficient. However, they are associated with potential risks, including increased susceptibility to infections, and should be administered under close medical supervision.
Physical Therapy and Exercise
Physical therapy and exercise are integral components of ankylosing spondylitis management. They help maintain flexibility, improve mobility, and reduce pain. Regular exercise, including specific stretches and strengthening exercises, can help maintain spinal mobility and prevent stiffness.
- Maintaining Flexibility: A regular stretching routine is crucial for preserving spinal flexibility and preventing the stiffness associated with ankylosing spondylitis. Gentle, controlled stretches, guided by a physical therapist, are essential to maintain joint mobility and prevent the progressive fusion of the spine.
- Strengthening Exercises: Strengthening exercises, focused on core muscles and surrounding areas, help support the spine and reduce the risk of further spinal damage. This support minimizes pain and enhances posture and stability.
- Aerobic Exercise: Aerobic exercises like swimming, cycling, or walking can help improve cardiovascular health and overall well-being, important aspects in managing the disease.
Surgical Treatment
Surgical interventions are reserved for cases of ankylosing spondylitis where other treatments have failed to adequately manage pain or improve mobility. Surgery may be considered for severe spinal deformity, debilitating pain, or significant nerve compression.
- Surgical Procedures: Surgical procedures for ankylosing spondylitis vary depending on the specific needs of the patient. They may include spinal fusion procedures to stabilize the spine, decompression surgeries to alleviate nerve compression, or joint replacements for affected joints. The choice of procedure depends on the extent of the spinal involvement and the patient’s overall health.
Comparison of Medication Classes
| Medication Class | Mechanism of Action | Typical Benefits | Potential Side Effects |
|---|---|---|---|
| NSAIDs | Reduce inflammation and pain by inhibiting cyclooxygenase enzymes. | Effective pain relief and inflammation reduction. | Gastrointestinal issues (e.g., ulcers, bleeding). |
| DMARDs | Modify the immune response and slow disease progression. | Potential to slow disease progression and improve symptoms. | Potentially more severe side effects (e.g., liver damage, blood disorders). |
| Biologics | Target specific components of the immune system involved in inflammation. | Highly effective in reducing inflammation and pain. | Increased risk of infections, other side effects. |
Non-Pharmacological Interventions
Beyond medication, a holistic approach to managing ankylosing spondylitis (AS) emphasizes non-pharmacological interventions. These strategies, often overlooked, play a crucial role in improving quality of life and managing symptoms. They work synergistically with medication to provide comprehensive pain relief and functional improvement. Implementing these methods alongside medical treatment can significantly enhance overall well-being.Effective management of AS involves a multifaceted approach.
Non-pharmacological interventions, including lifestyle modifications and specific therapies, are vital in complementing pharmacological treatments and fostering a proactive approach to disease control. By incorporating these strategies into daily routines, individuals with AS can experience greater comfort, reduced pain, and improved mobility.
Lifestyle Modifications
Lifestyle adjustments can profoundly impact the management of AS. Dietary choices and regular exercise are fundamental components of a well-rounded approach. A balanced diet rich in anti-inflammatory foods and regular physical activity contribute to pain reduction and improved joint function. Adequate hydration is also essential for overall health and comfort.
| Category | Specific Modifications |
|---|---|
| Diet | Prioritize anti-inflammatory foods like fruits, vegetables, and omega-3 rich fish. Limit processed foods, red meat, and sugary drinks. |
| Exercise | Engage in regular low-impact exercises like swimming, cycling, and walking. Consistency is key, even if starting with short durations. |
| Hydration | Drink plenty of water throughout the day to maintain joint lubrication and overall bodily functions. |
| Stress Management | Practice relaxation techniques like yoga, meditation, or deep breathing exercises to reduce stress and its impact on pain. |
Physical Therapy
Physical therapy is crucial in managing AS. Trained therapists design personalized exercise programs and manual therapy techniques to improve joint mobility, reduce pain, and maintain flexibility. This tailored approach ensures that each individual receives the best possible care based on their unique needs and challenges. Early intervention is often key to preventing long-term complications.Physical therapists use a variety of techniques, including stretching, strengthening exercises, and manual mobilization, to improve range of motion and reduce stiffness.
These methods help maintain flexibility in the spine and other affected joints.
Occupational Therapy
Occupational therapy plays a significant role in adapting daily tasks and activities to accommodate the limitations imposed by AS. This approach is tailored to the specific needs of each individual. By evaluating daily routines, occupational therapists identify areas for modification and implement strategies to maintain independence and quality of life.Occupational therapists assist patients in adapting their homes and work environments.
They may provide assistive devices or suggest modifications to improve ease of movement and reduce physical strain.
Exercise Routines and Stretches
Regular exercise is essential for maintaining mobility and reducing pain in AS. Specific exercises and stretches can be incredibly beneficial in managing the condition.
- Gentle stretches: Holding gentle stretches for 30 seconds, several times a day, can significantly improve flexibility. Examples include spinal twists, forward bends, and neck rotations. These should be tailored to individual tolerance and pain levels.
- Low-impact aerobic exercises: Activities like swimming, cycling, or walking can improve cardiovascular health and maintain muscle strength without putting undue stress on joints. Starting slowly and gradually increasing intensity is crucial.
- Strengthening exercises: Strengthening exercises, like those focusing on core muscles, can help support the spine and reduce pain. These should be performed under the guidance of a physical therapist.
Monitoring and Management Strategies
Living with ankylosing spondylitis (AS) requires a proactive and ongoing approach to monitoring and management. Effective strategies involve regular medical check-ups, targeted therapies, and a commitment to self-care. This proactive approach allows for early intervention, minimizes complications, and improves overall quality of life.
Importance of Regular Follow-up Appointments
Regular visits to a rheumatologist are crucial for monitoring the progression of AS and adjusting treatment plans as needed. These appointments allow for the evaluation of disease activity, assessment of spinal mobility, and identification of potential complications. Consistent follow-up helps track the effectiveness of therapies and enables the rheumatologist to make necessary adjustments to ensure optimal management of the condition.
Role of Healthcare Professionals
Rheumatologists play a central role in the management of AS, guiding treatment strategies and monitoring disease progression. They are experienced in diagnosing AS, prescribing medications, and managing potential complications. Physical therapists are also essential in developing exercise programs tailored to the individual’s needs, improving spinal mobility, and mitigating pain. These professionals work collaboratively to provide comprehensive care and support.
Patient Self-Management and Adherence
Patient self-management is vital in the overall management of AS. This involves actively participating in treatment plans, adhering to medication schedules, and consistently performing prescribed exercises. Understanding the disease and its impact on daily life allows patients to develop coping mechanisms and lifestyle adjustments. This proactive approach can significantly enhance the effectiveness of medical interventions.
Strategies for Managing Pain and Stiffness
Managing pain and stiffness associated with AS requires a multifaceted approach. Regular exercise, including low-impact activities like swimming and walking, can help improve spinal mobility and reduce stiffness. Heat therapy, such as warm baths or heating pads, can provide temporary relief from muscle pain and stiffness. Pain management medications, as prescribed by the rheumatologist, can also be used to control symptoms.
Common Complications and Mitigation Strategies
| Common Complications | Mitigation Strategies |
|---|---|
| Cardiovascular disease: AS increases the risk of developing cardiovascular issues like hypertension and atherosclerosis. | Maintaining a healthy weight, regular exercise, a balanced diet low in saturated fats, and monitoring blood pressure are crucial. |
| Osteoporosis: Inflammation associated with AS can weaken bones, increasing the risk of fractures. | Adequate calcium and vitamin D intake, weight-bearing exercises, and medication (as prescribed by the doctor) can help strengthen bones. |
| Eye inflammation (uveitis): Uveitis is a common ocular complication, potentially leading to vision loss if left untreated. | Regular eye exams and prompt treatment of uveitis by an ophthalmologist are critical. Following the rheumatologist’s treatment plan closely is essential. |
| Pulmonary complications: AS can affect the lungs, potentially causing restrictive lung disease. | Regular respiratory function tests, pulmonary rehabilitation, and managing any respiratory infections promptly are important. |
| Neurological complications: In some cases, AS can impact the nervous system, leading to nerve pain or other neurological issues. | Close monitoring by neurologists, following treatment plans, and managing pain and inflammation are vital. |
Specific Considerations for Patients
Ankylosing spondylitis (AS) isn’t just a physical condition; it significantly impacts a patient’s overall well-being, affecting their social interactions, emotional state, and professional life. Understanding these multifaceted implications is crucial for effective management and support. This section delves into the personal challenges faced by AS patients and the resources available to navigate these difficulties.Beyond the physical limitations, AS can create emotional and social challenges.
The chronic nature of the disease, coupled with the potential for pain and stiffness, can lead to feelings of isolation, frustration, and anxiety. This often manifests as difficulties maintaining relationships, participating in social activities, and pursuing hobbies. Acknowledging these challenges is vital to ensuring comprehensive care.
Ankylosing spondylitis treatment often involves a multifaceted approach, focusing on managing pain and stiffness. While physical therapy and medication are key components, sometimes surgery is necessary. For example, in cases of specific injuries like clavicle fractures, surgical intervention might be required, like in surgery for clavicle fractures. Ultimately, the best treatment for ankylosing spondylitis is tailored to the individual patient and their specific needs.
Impact on Different Aspects of Life
AS can profoundly impact various aspects of a patient’s life. The persistent pain, stiffness, and fatigue can significantly reduce physical activity levels, affecting participation in social gatherings and recreational pursuits. This can lead to feelings of isolation and a diminished social circle.Emotional well-being is also impacted. The unpredictable nature of the disease, coupled with the potential for long-term complications, can contribute to anxiety, depression, and low self-esteem.
The fear of pain flares, the uncertainty of future limitations, and the social stigma associated with chronic illness can significantly affect mental health. Addressing these emotional aspects is just as important as managing the physical symptoms.Vocational life can be equally affected. The varying degrees of physical limitations and fatigue associated with AS can create challenges in maintaining employment.
The need for frequent medical appointments, pain management, and potential disability accommodations can disrupt work schedules and potentially lead to career adjustments. Understanding the potential impact on career choices and proactively planning for potential accommodations is crucial.
Managing ankylosing spondylitis involves a multifaceted approach, and a crucial component is diet. While there’s no single ‘cure-all’ food, a balanced diet is key. For example, consulting a dietitian about incorporating high protein drinks, as recommended by many dietitians, can be helpful in supporting muscle strength and overall well-being. This can be a positive addition to your treatment plan, alongside other strategies like physical therapy and medication, to effectively manage the symptoms of ankylosing spondylitis.
high protein drinks dietitian recommendation can provide valuable insights.
Importance of Patient Education and Support Groups
Comprehensive patient education is essential for effectively managing AS. Understanding the disease’s progression, potential complications, and available treatment options empowers patients to actively participate in their care. Education also helps patients to recognize early warning signs of exacerbations, enabling them to seek prompt medical attention. This knowledge is crucial for preventing long-term complications.Support groups play a vital role in the journey of AS patients.
Connecting with others who share similar experiences provides a platform for emotional support, practical advice, and the sharing of coping strategies. The sense of community and shared understanding can significantly alleviate feelings of isolation and provide a safe space for emotional expression. Finding support groups or online forums dedicated to AS is crucial.
Resources Available to Patients
Numerous resources are available to assist AS patients. Local and national support groups provide a crucial network for emotional support and practical guidance. Online forums and social media groups offer opportunities to connect with others, share experiences, and access a wealth of information. These virtual communities can be invaluable for connecting with experts and peers, offering a sense of shared experience and understanding.Furthermore, many organizations offer educational materials, resources, and support services tailored to the needs of AS patients.
These materials can be accessed through websites, pamphlets, and presentations, providing valuable insights into the disease and its management.
Potential Impact on Quality of Life
AS can significantly impact a patient’s quality of life. The chronic pain, fatigue, and physical limitations can restrict daily activities, impacting social interactions, vocational pursuits, and overall well-being. Understanding the multifaceted nature of this impact is critical for healthcare providers and support systems to effectively address the patient’s needs.
Potential Career Adjustments
| Potential Career Adjustment | Description |
|---|---|
| Job Modifications | Adjusting tasks, responsibilities, or work environment to accommodate physical limitations. Examples include modified work schedules, assistive devices, or ergonomic adaptations. |
| Career Transition | Exploring alternative career paths that are less physically demanding or better suited to the patient’s abilities. This might involve retraining or seeking new opportunities. |
| Temporary Leave or Reduced Workload | Taking temporary breaks or reducing work hours to manage flare-ups or address medical needs. |
| Telecommuting or Remote Work | Working from home or a remote location to avoid strenuous commutes or physical demands of a traditional office setting. |
| Seeking Disability Accommodations | Utilizing resources and accommodations to maintain employment, such as modified duties, adjusted work hours, or assistive technologies. |
Future Research Directions
The journey to better understanding and managing ankylosing spondylitis (AS) is an ongoing one. Ongoing research is crucial to refining diagnostic tools, developing more effective treatments, and ultimately improving the quality of life for those affected by this chronic inflammatory condition. This exploration into future research directions will illuminate the exciting avenues currently being pursued.
Understanding the Pathogenesis of AS
Research continues to unravel the complex interplay of genetic and environmental factors contributing to the development of AS. Identifying specific genetic markers and environmental triggers is critical for developing preventive strategies and personalized treatments. Studies are investigating the role of immune dysregulation, particularly the involvement of specific immune cells and inflammatory pathways. Further exploration into the precise mechanisms of bone and cartilage damage in AS is also crucial for developing effective therapeutic targets.
Developing Novel Therapeutic Strategies
Current treatments for AS primarily focus on managing symptoms and slowing disease progression. However, there’s a need for more targeted therapies that address the underlying causes of the condition. Research is actively exploring the use of biologics and small molecule inhibitors targeting specific inflammatory pathways. Furthermore, investigations are underway to develop therapies that directly address the bone and cartilage damage associated with AS, potentially through regenerative medicine approaches.
Clinical trials are evaluating the efficacy and safety of new therapies, such as those that modulate the immune system’s response, or that promote cartilage regeneration.
Improving Diagnostic Accuracy and Early Detection
Early diagnosis of AS is crucial for effective treatment and disease management. Research is focusing on developing more sensitive and specific diagnostic markers, potentially using blood tests or imaging techniques to detect subtle signs of inflammation before the development of significant structural changes. This could lead to earlier interventions and better outcomes. New diagnostic tools are being evaluated for their ability to detect the disease earlier, and potentially differentiate AS from other similar conditions.
This proactive approach will allow for more timely and appropriate treatment interventions.
Personalized Medicine Approaches
Recognizing the significant variability in disease presentation and response to treatment in AS patients, research is exploring personalized medicine approaches. This involves developing strategies to tailor treatment plans based on individual patient characteristics, including genetic predisposition, environmental factors, and disease severity. This could involve utilizing genetic profiling to predict individual responses to specific treatments, leading to more effective and less harmful therapies.
The goal is to move away from a one-size-fits-all approach and toward individualized treatment plans for each patient.
Table of Key Research Areas and Potential Impact
| Research Area | Potential Impact |
|---|---|
| Understanding the pathogenesis of AS | Development of preventive strategies and personalized treatments |
| Developing novel therapeutic strategies | More targeted therapies addressing underlying causes of AS |
| Improving diagnostic accuracy and early detection | Earlier interventions and better outcomes |
| Personalized medicine approaches | Tailored treatment plans based on individual characteristics |
Conclusive Thoughts
In conclusion, the treatment of ankylosing spondylitis is a dynamic process requiring a collaborative effort between patients and healthcare professionals. Understanding the different facets of the disease, from diagnosis to long-term management, is key to effectively navigating this condition. We’ve highlighted the importance of personalized care, patient education, and the support network available to those affected. By combining knowledge and resources, individuals with ankylosing spondylitis can improve their quality of life.




