The integumentary system anatomy and function is a fascinating exploration of the skin, its appendages, and its crucial role in maintaining homeostasis. From the outermost layer of the epidermis to the intricate network of sensory receptors, this system plays a vital part in protecting our bodies from the external environment. We’ll delve into the layers of the skin, explore the appendages like hair and nails, and examine the fascinating world of skin color and pigmentation.
Understanding the structure and function of the integumentary system is crucial for comprehending its intricate relationship with other body systems. It’s not just a barrier, but a dynamic organ system that contributes to everything from temperature regulation to sensory perception and immune response. This comprehensive overview will dissect the anatomy of the skin and its various components, illuminating the interplay between structure and function.
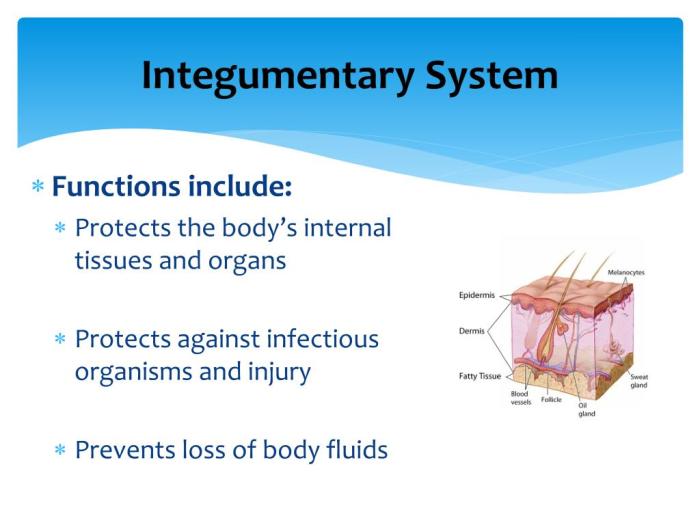
Introduction to the Integumentary System
The integumentary system, our body’s largest organ system, is more than just skin deep. It plays a crucial role in protecting us from the external environment, regulating our internal temperature, and even aiding in the production of vital vitamins. Understanding its intricate workings is essential for comprehending our overall health and well-being.This system is intricately connected to other bodily systems.
For example, its role in temperature regulation impacts the cardiovascular system, while its sensory receptors provide input to the nervous system. Its interactions extend to the skeletal system, providing support and attachment sites for some structures, and the immune system, as it houses and interacts with immune cells. This interconnectedness highlights the importance of maintaining the integrity of this system for overall body function.
Components of the Integumentary System
The integumentary system comprises several interconnected tissues and structures, working in concert to perform its diverse functions. Key components include the epidermis, dermis, subcutaneous tissue, hair follicles, sweat glands, and nails. These elements, with their specialized structures and functions, form a complex protective barrier.
Major Components of the Integumentary System
The integumentary system is a multifaceted shield, comprised of various components that work together to protect and maintain the body. Understanding these components and their roles is vital to grasping the system’s overall function.
| Component | Location | Description | Key Function |
|---|---|---|---|
| Epidermis | Outermost layer of the skin | A stratified squamous epithelium composed of keratinized cells. It contains melanocytes that produce melanin, providing pigmentation and UV protection. | Provides a waterproof barrier, protects against pathogens, and regulates temperature. |
| Dermis | Layer beneath the epidermis | A dense connective tissue layer containing collagen and elastin fibers, blood vessels, nerves, hair follicles, and sweat glands. | Provides structural support, houses sensory receptors, and regulates temperature. |
| Subcutaneous Tissue (Hypodermis) | Beneath the dermis | A layer of loose connective tissue and adipose tissue. It connects the skin to underlying tissues and organs. | Insulates the body, stores energy, and provides cushioning. |
| Hair Follicles | Embedded in the dermis | Structures that produce hair, and contain sebaceous glands that secrete sebum, an oily substance. | Provides insulation, protection, and sensory input. Sebum keeps skin and hair lubricated. |
| Sweat Glands | Located in the dermis and subcutaneous tissue | Exocrine glands that secrete sweat, a fluid that helps regulate body temperature and eliminate waste products. There are eccrine and apocrine sweat glands. | Regulates body temperature through evaporation and eliminates waste. |
| Nails | Protective coverings on the tips of fingers and toes | Hard, keratinized plates that protect the tips of digits. | Protects the tips of digits and aids in grasping objects. |
Anatomy of the Skin
The skin, our largest organ, is a complex and fascinating structure that plays a vital role in protecting us from the external environment. Understanding its anatomy, from the outermost layer to the deeper tissues, reveals the intricate design that allows it to perform its many functions, such as regulating temperature, protecting against pathogens, and synthesizing vitamin D. Its layers work together in a remarkable symphony to maintain our overall health and well-being.
Layers of the Epidermis
The epidermis, the outermost layer of the skin, acts as a formidable barrier against the outside world. It is composed of several layers of stratified squamous epithelial cells, each with distinct characteristics and functions. These layers work together to create a protective shield against environmental hazards.
- Stratum Corneum: This is the outermost layer of the epidermis, composed of dead, flattened keratinocytes. These cells are tightly packed together and filled with keratin, a tough protein that provides waterproofing and protection. The constant shedding of these cells is a natural process.
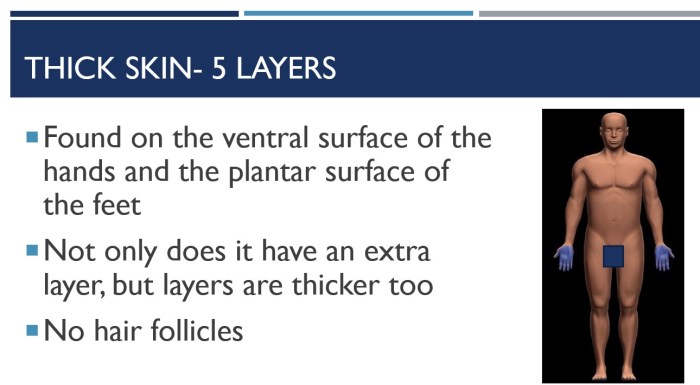
- Stratum Lucidum: Found only in thick skin areas like the palms and soles, this layer consists of clear, flattened keratinocytes. The cells lack nuclei and organelles, contributing to the layer’s transparency.
- Stratum Granulosum: In this layer, keratinocytes begin to flatten and die. They produce keratohyalin granules, which contribute to the waterproofing function of the skin. The cells also produce lamellar granules that release lipids, further contributing to the skin’s barrier function.
- Stratum Spinosum: This layer contains numerous keratinocytes connected by desmosomes. These specialized junctions provide strength and integrity to the epidermis. Melanocytes, responsible for producing melanin, are also present in this layer.
- Stratum Basale: This is the deepest layer of the epidermis, directly attached to the dermis. It contains actively dividing keratinocytes, melanocytes, and Merkel cells. The keratinocytes produced here eventually migrate upward, differentiating into the various layers above. Merkel cells are involved in touch sensation.
Layers of the Dermis
The dermis, located beneath the epidermis, is a thicker, connective tissue layer that provides support and structure to the skin. It contains a rich network of blood vessels, nerves, hair follicles, and glands. The dermis’s intricate design allows it to support the epidermis and provide a multitude of functions.
- Papillary Layer: This is the upper layer of the dermis, composed of loose connective tissue. It contains dermal papillae, finger-like projections that interlock with the epidermis, enhancing the skin’s structural integrity. These papillae also contain capillaries, contributing to the skin’s nourishment and temperature regulation.
- Reticular Layer: This is the deeper layer of the dermis, composed of dense irregular connective tissue. It contains collagen and elastin fibers that provide strength, flexibility, and elasticity to the skin. The arrangement of these fibers determines the skin’s overall texture and appearance.
Layers of the Hypodermis
The hypodermis, also known as the subcutaneous tissue, is the deepest layer of the skin. It connects the skin to underlying tissues and organs. It primarily consists of adipose tissue, which provides insulation, cushioning, and energy storage. Its structural components contribute to the overall form and function of the skin.
Cellular Components of the Skin
| Cell Type | Layer Location | Function | Special Characteristics |
|---|---|---|---|
| Keratinocytes | Epidermis (all layers) | Produce keratin, a tough protein that provides waterproofing and protection. | Most abundant cell type in the epidermis; undergo keratinization |
| Melanocytes | Epidermis (stratum basale) | Produce melanin, a pigment that protects against UV radiation. | Contain melanin granules; distribute melanin to keratinocytes |
| Merkel Cells | Epidermis (stratum basale) | Sensory receptors involved in touch sensation. | Associated with sensory nerve endings; contribute to tactile discrimination |
| Langerhans Cells | Epidermis (stratum spinosum) | Immune cells that participate in the immune response. | Dendritic cells; phagocytic function |
| Fibroblasts | Dermis | Produce collagen and elastin fibers, contributing to skin strength and elasticity. | Produce extracellular matrix components; important for tissue repair |
Diagram of Skin Cross-Section
Imagine a vertical slice through the skin. The outermost layer, the epidermis, appears as a thin, multi-layered sheet. The stratum corneum, the outermost layer, is composed of flattened, dead cells, and is visible as a continuous layer. Beneath this, the stratum lucidum (only in thick skin) is transparent. The stratum granulosum shows cells beginning to flatten and die.
The stratum spinosum is a spiky layer with keratinocytes connected by desmosomes. The stratum basale, the deepest epidermal layer, is in direct contact with the dermis. The dermis, appearing thicker than the epidermis, is divided into the papillary and reticular layers. The papillary layer shows projections (papillae) that interlock with the epidermis. The reticular layer is composed of dense connective tissue containing collagen and elastin fibers.
Deepest of all is the hypodermis, appearing as a layer of fatty tissue (adipose). Blood vessels and nerves are scattered throughout the dermis and hypodermis.
Appendages of the Skin: The Integumentary System Anatomy And Function
The skin isn’t just a protective barrier; it’s a dynamic system with intricate appendages that contribute to its overall function and health. These appendages, including hair, nails, and glands, play crucial roles in maintaining homeostasis, regulating body temperature, and providing sensory input. Understanding their structures and functions is key to appreciating the complexity of the integumentary system.
Hair
Hair follicles are complex structures embedded in the dermis, extending into the subcutaneous tissue. They are responsible for producing hair, a filamentous protein structure composed primarily of keratin. The structure of hair includes the shaft, the root, and the follicle itself. The shaft, the visible portion of the hair, is composed of overlapping keratinized cells. The root, which is embedded within the follicle, is responsible for hair growth.
The follicle is lined with specialized cells that produce and nourish the hair. Hair growth is a cyclical process, with periods of active growth and resting phases. Hair color is determined by the amount and type of melanin produced by specialized cells within the follicle.
Nails
Nails are hard, keratinized plates that protect the tips of the fingers and toes. They are formed from specialized epithelial cells that are continuously produced at the nail root. The nail plate is composed of tightly packed, flattened keratinocytes. The nail root, which is hidden beneath the skin at the base of the nail, is the origin of new nail growth.
The nail bed is the underlying skin that supports the nail plate. The lunula, the whitish semilunar area at the base of the nail, is the actively growing part of the nail.
Glands
Skin glands are essential for maintaining homeostasis and regulating various bodily functions. They are classified into two main types: sweat glands and sebaceous glands. Understanding the difference between these glands and their functions is critical for grasping the complexity of the integumentary system.
Sweat Glands
Sweat glands are exocrine glands that produce sweat, a watery secretion that plays a crucial role in thermoregulation. These glands are distributed throughout the skin, particularly on the palms, soles, and forehead. Two main types of sweat glands exist: eccrine and apocrine. Eccrine glands are responsible for the majority of sweat production, regulating body temperature. Apocrine glands are primarily located in the armpits and groin area, and their secretions become noticeable during puberty.
Sebaceous Glands
Sebaceous glands are exocrine glands that produce sebum, an oily substance that lubricates the skin and hair. These glands are found throughout the body, except on the palms and soles. Sebum helps to maintain skin moisture and flexibility, protecting the skin from environmental damage. Sebum also plays a role in antimicrobial defense, inhibiting the growth of certain bacteria.
The integumentary system, our skin, hair, and nails, is a pretty amazing protective barrier. But sometimes, waking up with stomach pain can be a real downer, and it’s important to consider the causes. Knowing the delicate balance of your digestive system can help you better understand potential triggers, and this could impact your overall health, just as the integumentary system protects your body from the outside world.
Learning more about the anatomy and function of the integumentary system can lead to better overall health. For more on waking up with stomach pain, check out this helpful guide: waking up with stomach pain.
Comparison of Appendages
| Appendage | Structure | Function | Location |
|---|---|---|---|
| Hair | Filamentous protein structure composed of keratin | Protection, insulation, sensory input | Distributed throughout the body, except palms and soles |
| Nails | Hard, keratinized plates | Protection of fingertips and toes | Tips of fingers and toes |
| Eccrine Sweat Glands | Tubular glands | Thermoregulation | Distributed throughout the skin |
| Apocrine Sweat Glands | Tubular glands | Thermoregulation, possibly involved in scent | Armpits, groin |
| Sebaceous Glands | Holocrine glands | Lubrication of skin and hair, antimicrobial defense | Distributed throughout the body, except palms and soles |
Role in Homeostasis
Each appendage plays a critical role in maintaining homeostasis. Hair provides insulation, protecting the body from extreme temperatures. Nails protect the delicate tips of fingers and toes, while sweat glands regulate body temperature by releasing sweat, and sebaceous glands maintain skin moisture and flexibility, protecting the skin from environmental damage. These integrated systems contribute to the overall health and well-being of the individual.
Skin Color and Pigmentation
Skin color, a fascinating aspect of human diversity, is a complex interplay of genetic factors, environmental influences, and physiological processes. This intricate system not only defines our appearance but also plays a crucial role in protecting us from the harmful effects of the sun. Understanding the mechanisms behind skin color variations is essential for appreciating the beauty and diversity of our species, as well as recognizing the potential health implications associated with certain skin tones.
Mechanisms of Skin Color Variations
Skin color is primarily determined by the amount and type of melanin produced by specialized cells called melanocytes. Melanin, a pigment produced within melanocytes, acts as a natural sunscreen, absorbing ultraviolet (UV) radiation from the sun. Different types of melanin, such as eumelanin (brown/black) and pheomelanin (yellow/red), contribute to the spectrum of skin colors observed across populations. Variations in the production and distribution of these pigments result in a wide range of skin tones.
Other factors, like blood flow and the presence of carotenoids (pigments found in certain foods), also contribute to the overall skin color.
Role of Melanin in Skin Protection and Pigmentation
Melanin plays a critical role in protecting the skin from the damaging effects of UV radiation. The amount of melanin produced is directly related to the level of UV exposure. Higher melanin production leads to a darker skin tone, providing greater protection against sunburn and associated skin damage. This protective mechanism is crucial for preventing skin cancer and premature aging.
The integumentary system, encompassing skin, hair, and nails, plays a vital role in protecting our bodies. But did you know that what you eat can also impact your skin’s health? Choosing the right foods is crucial for overall well-being, including maintaining bone density. For instance, certain foods can hinder bone health, increasing the risk of osteoporosis. Learn more about foods to avoid with osteoporosis to ensure you’re supporting your body’s overall health.
Ultimately, a healthy diet supports the structural integrity of the integumentary system as well as your overall well-being.
Melanin’s protective function is further enhanced by its ability to absorb UV radiation and dissipate the absorbed energy as heat. The presence of melanin also significantly influences skin tone, with higher concentrations leading to darker skin colors.
Impact of Genetics, Sun Exposure, and Other Factors on Skin Tone
Genetics significantly influences skin tone, with individuals inheriting varying levels of melanin production capacity from their parents. Sun exposure is a crucial environmental factor in determining skin tone. Increased exposure to UV radiation triggers an increase in melanin production, leading to a temporary tanning effect. This response is a natural protective mechanism against the damaging effects of UV rays.
Other factors like hormones and certain medications can also influence skin tone. For instance, hormonal fluctuations during pregnancy can lead to changes in skin pigmentation.
Different Types of Skin Conditions and Diseases Related to Pigmentation
Several skin conditions and diseases can affect skin pigmentation, resulting in various skin tone abnormalities. These conditions can range from benign changes in pigmentation to more serious medical concerns. Examples include vitiligo, a condition characterized by the loss of pigment in certain areas of the skin, and melasma, a skin discoloration that often appears as brownish or grayish patches, particularly on the face.
These conditions can have varying degrees of severity and may necessitate medical intervention for diagnosis and treatment. The diverse nature of these conditions highlights the importance of consulting with healthcare professionals for appropriate evaluation and management.
Table: Skin Colors, Causes, and Associated Health Concerns
| Skin Color | Causes | Associated Health Concerns | Further Notes |
|---|---|---|---|
| Light Skin | Lower melanin production, genetic predisposition | Increased risk of sunburn, skin cancer (melanoma, basal cell carcinoma, squamous cell carcinoma), premature aging | Requires more caution regarding sun exposure |
| Medium Skin | Moderate melanin production, genetic predisposition | Moderate risk of sunburn, skin cancer | May require sun protection measures, especially during peak sun hours |
| Dark Skin | High melanin production, genetic predisposition | Lower risk of sunburn, skin cancer | Still susceptible to sun damage, proper sun protection is recommended |
| Other Pigmentation Variations | Vitiligo, melasma, other skin conditions | May cause skin discoloration, discomfort, or other medical complications | Requires professional evaluation and treatment |
Sensory Receptors and Functions
The skin, our largest organ, is far more than just a protective barrier. It’s a complex sensory system, constantly monitoring our environment and relaying information to the brain. This intricate network of sensory receptors allows us to perceive touch, temperature, pain, and pressure, providing crucial feedback about our surroundings and our body’s condition. Understanding these receptors is key to appreciating the intricate interplay between the skin and the rest of the nervous system.
Types of Sensory Receptors
The skin houses a diverse array of sensory receptors, each specialized to detect specific stimuli. These receptors vary in structure and location, reflecting their distinct functions in gathering and transmitting information. Their sensitivity to different stimuli allows us to experience a wide range of sensations.
Mechanoreceptors
Mechanoreceptors respond to mechanical forces such as pressure, touch, and vibration. These receptors are crucial for detecting textures, shapes, and movements in our environment. Different types of mechanoreceptors are specialized for different types of stimuli.
| Sensory Receptor | Location | Stimuli Detected | Resulting Sensation |
|---|---|---|---|
| Merkel cells | Base of epidermis | Light touch, sustained pressure | Fine details, shapes |
| Meissner corpuscles | Dermis, especially hairless skin | Light touch, low-frequency vibration | Texture, grip |
| Ruffini endings | Dermis, hypodermis | Sustained pressure, skin stretching | Sustained touch, stretching |
| Pacinian corpuscles | Dermis, hypodermis | Deep pressure, high-frequency vibration | Deep pressure, vibrations |
Thermoreceptors
Thermoreceptors are specialized to detect changes in temperature. These receptors are crucial for maintaining a stable internal body temperature (thermoregulation). The skin contains both warm and cold receptors, allowing for a precise assessment of temperature gradients.
Nociceptors
Nociceptors are pain receptors that respond to potentially harmful stimuli, such as extreme temperatures, strong pressure, or chemical irritants. Their function is vital for protecting the body from tissue damage. Nociceptors are free nerve endings, meaning they lack specialized structures. Activation of nociceptors leads to the perception of pain.
Role in Body Awareness
The sensory information gathered by these receptors is crucial for body awareness and proprioception. Our ability to perceive the position and movement of our body parts depends on the signals sent from these receptors to the brain. This integrated sensory input contributes to our understanding of our body in space and guides our movements. These signals are also crucial for adjusting posture and coordination.
Regulation of Body Temperature
The input from thermoreceptors plays a key role in thermoregulation. Changes in temperature sensed by these receptors trigger physiological responses to maintain a stable internal temperature. For example, sweating cools the body during heat exposure. Conversely, shivering generates heat to combat cold temperatures. This regulatory mechanism is vital for maintaining homeostasis.
Integumentary System and Homeostasis
The integumentary system, encompassing the skin, hair, nails, and associated glands, plays a crucial role in maintaining the internal balance of the body, or homeostasis. This intricate system acts as a barrier against the external environment, while simultaneously regulating vital functions such as temperature control, fluid balance, and protection against pathogens. Understanding these functions is key to appreciating the system’s overall contribution to human health and well-being.The skin’s remarkable adaptability and intricate physiological mechanisms enable it to respond effectively to environmental changes, ensuring a stable internal environment despite external fluctuations.
The integumentary system, our skin, plays a crucial role in protecting us from the outside world. Understanding its layers and functions is fascinating, but sometimes we need a little extra support for optimal health. For example, knowing when to take ashwagandha when to take ashwagandha can impact its effectiveness, much like how proper skin care contributes to the overall health of our integumentary system.
Ultimately, a well-functioning integumentary system is key to overall well-being.
This active participation in homeostasis makes the integumentary system a critical component of overall human health.
Thermoregulation
The skin’s role in regulating body temperature is paramount. Through a complex interplay of mechanisms, the skin maintains a stable internal temperature, crucial for optimal cellular function. This regulation involves both heat loss and heat conservation. When body temperature rises, the skin vasodilates, increasing blood flow to the surface, facilitating heat dissipation. Conversely, when body temperature drops, the skin vasoconstricts, reducing blood flow and conserving heat.
Sweat glands also contribute significantly to thermoregulation, releasing sweat that evaporates, drawing heat away from the body. This precisely controlled process ensures a stable internal temperature, preventing potentially harmful fluctuations.
Fluid Balance
The skin acts as a crucial barrier in maintaining fluid balance. Its tight structure prevents excessive water loss from the body, preventing dehydration. This protective function is critical in maintaining the proper hydration levels necessary for cellular function and overall well-being. Conversely, the skin also plays a role in excreting small amounts of water and electrolytes through sweat, contributing to the regulation of electrolytes and minerals in the body.
This dual role underscores the skin’s importance in maintaining a delicate balance of fluids within the body.
Protection Against Pathogens
The skin forms a formidable barrier against pathogens. Its physical integrity, along with the presence of antimicrobial peptides and other protective components, prevents the entry of harmful microorganisms. This barrier function is essential in preventing infections and maintaining overall health. Additionally, the skin’s constant shedding of dead cells helps remove potential pathogens from the surface, further contributing to this protective function.
This layered approach to defense underscores the skin’s vital role in protecting the body from external threats.
Wound Healing
Wound healing is a complex process involving several distinct phases, each characterized by specific cellular and molecular events. The process is essential for restoring the integrity of the skin and preventing infection. The intricate steps involved in wound healing highlight the remarkable regenerative capacity of the integumentary system.
- Inflammation: The initial phase of wound healing is characterized by the body’s inflammatory response. Blood vessels dilate, increasing blood flow to the injured area, allowing immune cells to reach the site and eliminate pathogens. This crucial step sets the stage for subsequent healing events.
- Proliferation: The proliferation phase involves the formation of new tissue. Fibroblasts, specialized cells, synthesize collagen and other extracellular matrix components, forming a scar tissue that gradually replaces the damaged tissue. This process is essential for restoring the structural integrity of the skin.
- Maturation: During the maturation phase, the scar tissue gradually remodels and matures. Collagen fibers reorganize, resulting in a scar that becomes less prominent and more functional over time. The skin gradually regains its normal appearance and function, highlighting the body’s remarkable regenerative capacity.
Physiological Responses to Environmental Changes
The integumentary system displays remarkable adaptability in response to environmental fluctuations. For instance, exposure to intense sunlight triggers the production of melanin, providing protection against harmful ultraviolet radiation. Similarly, exposure to extreme cold can result in vasoconstriction to conserve heat, while exposure to extreme heat can lead to vasodilation and sweating to dissipate heat. These adaptive responses ensure that the skin can effectively cope with varying environmental conditions, maintaining homeostasis despite fluctuations.
Wound Healing Flowchart
| Stage | Description |
|---|---|
| Inflammation | Blood vessels dilate, immune cells arrive, pathogens are eliminated. |
| Proliferation | Fibroblasts synthesize collagen, forming new tissue. |
| Maturation | Scar tissue remodels, collagen reorganizes, scar becomes less prominent. |
Integumentary System Disorders
The integumentary system, our body’s largest organ, is constantly exposed to environmental factors and internal imbalances. This vulnerability makes it susceptible to a wide array of disorders, ranging from mild irritations to severe conditions. Understanding these disorders is crucial for early detection, proper diagnosis, and effective treatment.Skin disorders manifest in various ways, affecting not only appearance but also overall health and well-being.
Recognizing the common causes, symptoms, and diagnostic methods for these conditions empowers individuals to seek timely medical attention and manage their skin health effectively.
Common Integumentary System Disorders
Numerous factors contribute to skin disorders, including genetic predisposition, environmental irritants, infections, and underlying medical conditions. Understanding the interplay of these factors helps in the diagnosis and treatment of these conditions.
- Acne: A common skin condition characterized by inflammation of the sebaceous glands, often appearing as pimples, blackheads, and cysts. Hormonal fluctuations, particularly during puberty and adulthood, are frequently implicated in acne development. Poor hygiene and the presence of bacteria on the skin can exacerbate the condition. Symptoms typically include redness, swelling, pain, and the formation of comedones (blackheads and whiteheads).
- Eczema: A chronic inflammatory skin condition that presents with dry, itchy, and inflamed skin. While the exact cause is often unknown, factors such as allergies, environmental triggers, and genetics may play a role. Symptoms vary, but common features include dry, cracked skin, redness, itching, and sometimes oozing or crusting.
- Psoriasis: A chronic autoimmune disorder characterized by rapid skin cell turnover, leading to red, scaly patches on the skin. Genetic predisposition is a significant risk factor, and environmental triggers like stress and infections can exacerbate the condition. Symptoms include thick, silvery scales, redness, and inflammation. In severe cases, it can affect joints and lead to psoriatic arthritis.
Diagnostic Procedures
Diagnosis of skin disorders often involves a combination of clinical examination and potentially, laboratory tests. Physicians evaluate the affected area, considering its location, appearance, and associated symptoms.
- Visual Inspection: A thorough visual assessment is the initial step in diagnosing skin disorders. This includes evaluating the color, texture, size, shape, and distribution of lesions.
- Biopsy: A skin biopsy involves removing a small sample of skin tissue for microscopic examination. This procedure is crucial for confirming the diagnosis, especially in cases of suspected cancer or other serious conditions.
- Allergy Testing: If allergies are suspected, allergy testing can help identify potential triggers for eczema or other allergic skin reactions. Patch testing is a common method for this.
Treatment Options, The integumentary system anatomy and function
Treatment approaches for skin disorders vary depending on the specific condition and its severity. They can range from topical medications to systemic therapies.
- Topical Medications: These treatments are applied directly to the affected skin area and include creams, ointments, and lotions. They often target inflammation, dryness, or infection.
- Systemic Medications: These medications are taken orally or intravenously and are used for more severe or widespread skin conditions. They can include oral antibiotics, immunosuppressants, or other drugs depending on the condition.
- Lifestyle Modifications: Maintaining a healthy lifestyle, such as managing stress, avoiding triggers, and maintaining good hygiene, can play a significant role in managing skin disorders.
Recognizing and Distinguishing Skin Disorders
Accurately recognizing and distinguishing various skin disorders requires a comprehensive understanding of their respective symptoms and presentations.
| Skin Disorder | Causes | Symptoms | Treatment Options |
|---|---|---|---|
| Acne | Hormonal imbalances, bacteria, genetics | Pimples, blackheads, cysts, redness, swelling | Topical medications, antibiotics, oral contraceptives |
| Eczema | Unknown (possible allergies, genetics, environmental triggers) | Dry, itchy, inflamed skin, redness, oozing | Moisturizers, topical corticosteroids, immunosuppressants |
| Psoriasis | Autoimmune disorder, genetic predisposition, environmental factors | Red, scaly patches, inflammation, thick scales | Topical medications, phototherapy, systemic medications |
Final Review
In conclusion, the integumentary system anatomy and function are complex and essential for overall health and well-being. From its role in protection and temperature regulation to its intricate sensory network, this system plays a vital part in our daily lives. Understanding the components, functions, and disorders of the integumentary system is crucial for maintaining optimal health and addressing any potential issues.
The next time you look in the mirror, appreciate the remarkable complexity of this amazing organ system.




