Exercises for patellar tendonitis are crucial for managing and recovering from this common knee ailment. This guide delves into the specifics of targeted exercises, from understanding the condition itself to progressive overload strategies and the importance of proper warm-up and cool-down routines. We’ll cover everything from strengthening quadriceps to improving flexibility, and even discuss crucial considerations like footwear and body weight.
This comprehensive approach provides a detailed roadmap for effectively managing patellar tendonitis through exercise. We’ll explore the anatomy, causes, and symptoms to equip you with a deeper understanding of this condition. Each exercise will be meticulously described, accompanied by safety precautions and progressive overload strategies for optimal results. By following these guidelines, you’ll be empowered to take control of your recovery and return to your active lifestyle.
Understanding Patellar Tendonitis
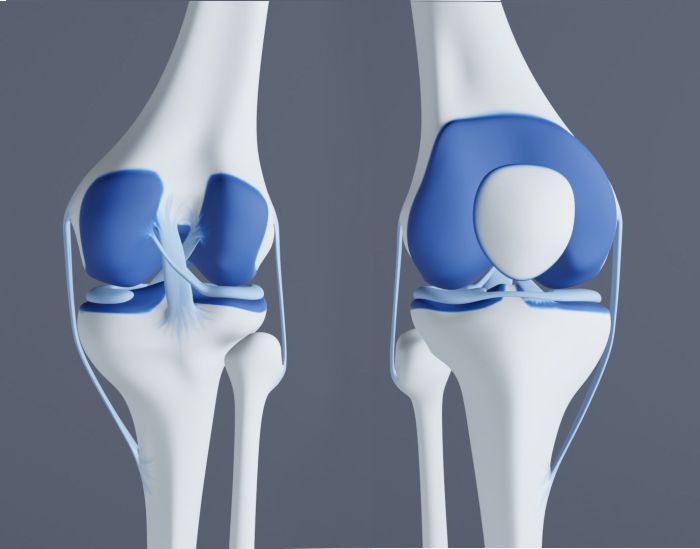
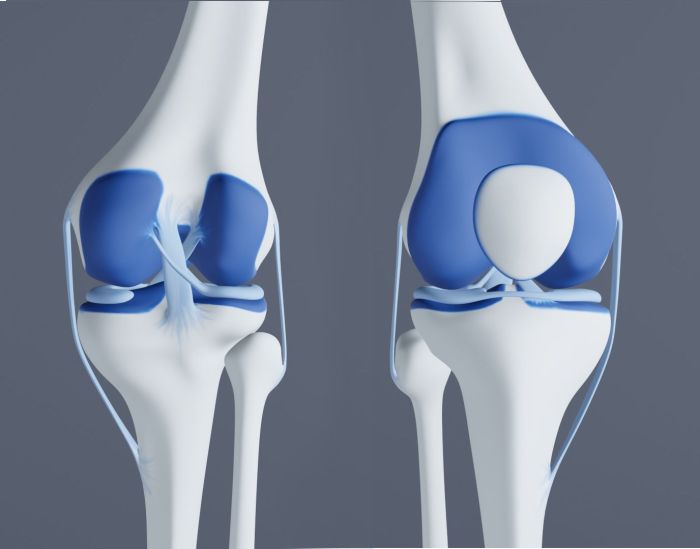
Patellar tendonitis, often called “jumper’s knee,” is a common overuse injury affecting the knee. It’s characterized by inflammation and pain in the patellar tendon, the tough band of tissue connecting the kneecap (patella) to the shinbone (tibia). Understanding the anatomy, causes, and symptoms is crucial for effective self-management and seeking appropriate medical attention.This condition typically arises from repetitive stress on the tendon, leading to microtears and inflammation.
It’s important to differentiate patellar tendonitis from other knee problems to ensure accurate diagnosis and treatment.
So, you’ve got patellar tendonitis? Finding the right exercises is key for recovery. While focusing on those, you might also be curious about lucrative medical careers, like those detailed in this article about what are the highest paying physician careers. Knowing that, you can keep working on your rehab program, focusing on strengthening exercises that are specifically designed to target the patellar tendon.
Anatomy of the Patellar Tendon
The patellar tendon, a crucial component of the knee joint, plays a vital role in knee extension. It’s composed of dense, fibrous connective tissue, designed to withstand considerable tensile forces during movement. This tendon transmits the force generated by the quadriceps muscle group to the tibia, allowing for straightening of the knee. The patella, acting as a pulley, enhances the leverage of the quadriceps, facilitating smooth knee extension.
Proper alignment and strength of the surrounding muscles are essential for optimal tendon function.
Causes and Risk Factors
Patellar tendonitis often results from repetitive movements that place excessive stress on the tendon. Activities such as jumping, running, and squatting, especially with improper form or excessive force, are common culprits. Athletes participating in sports like basketball, volleyball, and track and field are particularly susceptible. Individuals with a predisposition to flat feet or weakened leg muscles, such as those with tight hamstrings or weak hip abductors, also face a higher risk.
Other risk factors include poor footwear, improper training techniques, and inadequate warm-up routines.
Symptoms
The hallmark symptom of patellar tendonitis is pain around the kneecap. The pain is often described as a dull ache, or sharp, and can range from mild to severe. The pain is typically localized to the area below the kneecap, along the patellar tendon. The intensity of pain can increase with activities that stress the tendon, such as running, jumping, or climbing stairs.
Pain may also be aggravated by prolonged sitting, kneeling, or direct pressure on the tendon.
Comparison with Other Knee Conditions
While patellar tendonitis involves pain around the kneecap, it’s essential to distinguish it from other knee conditions. Conditions like Osgood-Schlatter disease, affecting adolescents, or meniscus tears, present with different symptoms and require distinct treatment approaches. A thorough examination by a healthcare professional is crucial for accurate diagnosis.
Grades of Patellar Tendonitis Severity
| Grade | Description | Symptoms |
|---|---|---|
| Mild | Initial inflammation and mild pain. Pain is present after activity but subsides with rest. | Slight tenderness, minimal pain during activity, pain relieved by rest. |
| Moderate | Increased pain and inflammation. Pain may persist even after rest. Limited range of motion. | Moderate pain during activity, pain lingers after activity, noticeable swelling, restricted movement. |
| Severe | Significant inflammation and pain. Pain is persistent, even at rest. Severe limitation of activity. | Intense pain, swelling, difficulty with weight-bearing, significant limitation of activity, possible creaking or popping sounds. |
This table provides a general guideline. Individual experiences may vary. A healthcare professional should provide a precise diagnosis and personalized treatment plan.
Exercise Recommendations for Patellar Tendonitis
Managing patellar tendonitis effectively involves a multifaceted approach that goes beyond rest. A carefully designed exercise program plays a crucial role in strengthening the supporting muscles, improving flexibility, and promoting proper patellar tracking. This comprehensive program aims to reduce pain, prevent recurrence, and restore optimal knee function.
Exercise Recommendations Table
This table Artikels key exercises for managing patellar tendonitis, categorized by their function and incorporating crucial precautions.
| Exercise Type | Description | Sets/Reps | Precautions |
|---|---|---|---|
| Quadriceps Strengthening | Focuses on building strength in the muscles that support the kneecap. | 2-3 sets of 10-15 repetitions, 2-3 times per week | Avoid excessive pain or discomfort. Listen to your body and modify the exercise if needed. Gradually increase the intensity and repetitions as tolerated. |
| Knee Flexibility and Range of Motion | Improves mobility in the knee joint and surrounding tissues. | 2-3 sets, holding each stretch for 20-30 seconds, 2-3 times per week | Avoid bouncing or forcing the stretch. Focus on a gentle, controlled movement. Hold stretches within your pain-free range. |
| Patellar Tracking Exercises | Improves the smooth movement of the kneecap within the groove. | 2-3 sets of 10-15 repetitions, 2-3 times per week | Perform exercises slowly and with control to avoid further irritation. If pain is experienced, stop immediately. |
| Low-Impact Cardio | Improves blood flow and reduces inflammation without excessive stress on the knee. | 30 minutes, 3-5 times per week | Choose activities like walking, swimming, or stationary cycling. Listen to your body and adjust intensity as needed. |
| Blood Flow and Inflammation Reduction | Increases blood flow to the affected area, promoting healing. | Daily or as directed by a physical therapist | Gentle massage or light heat application. Avoid activities that increase pain or inflammation. |
Quadriceps Strengthening Exercises
Strengthening the quadriceps is essential for supporting the kneecap and reducing stress on the patellar tendon. These exercises should be performed with controlled movements and proper form.
- Straight Leg Raises: Lie on your back with one leg straight and the other bent. Slowly lift the straight leg, maintaining a straight line from the knee to the hip. Lower the leg slowly. This targets the quadriceps femoris.
- Quad Sets: Squeeze your quadriceps muscle for a few seconds, holding the contraction. Repeat several times. This is a great way to maintain muscle activation throughout the day.
- Wall Slides: Stand facing a wall with your back against it. Slowly slide your back down the wall, bending your knees. Keep your back straight. This targets the quadriceps and hamstrings, and helps to improve knee extension.
Flexibility and Range of Motion Exercises
Improving flexibility and range of motion in the knee and surrounding areas is crucial for reducing stiffness and promoting proper function.
- Hamstring Stretches: Lie on your back with one leg straight in the air. Grab the back of your thigh and pull gently towards your chest. Hold the stretch for 20-30 seconds. Repeat on the other leg.
- Hip Flexor Stretches: Kneel on one knee, with the other leg bent in front. Lean forward, keeping your back straight, and feel the stretch in your hip flexors. Hold for 20-30 seconds and repeat on the other side.
- IT Band Stretches: Stand with your feet shoulder-width apart. Cross one leg over the other and bend your knee. Lean forward, keeping your back straight, until you feel the stretch in the outside of your hip and thigh. Hold for 20-30 seconds and repeat on the other side.
Patellar Tracking Exercises, Exercises for patellar tendonitis
Improving patellar tracking involves exercises that strengthen the muscles around the kneecap and encourage proper alignment.
- Kneeling Hip Flexor Stretch: Start on your hands and knees. Keeping your back straight, extend one leg out in front of you, resting the top of your foot on the floor. Feel the stretch in your hip flexor. Hold for 20-30 seconds and repeat on the other leg.
- Banded Patellar Tracking Exercises: Use a resistance band to provide gentle resistance while performing exercises that target the kneecap. This is helpful for restoring proper movement.
- Prone Knee Extensions: Lie on your stomach with your legs straight. Lift one leg, keeping the knee straight, until it is slightly off the floor. Lower slowly.
Low-Impact Exercises
Low-impact exercises are crucial for building strength and endurance without putting excessive stress on the patellar tendon.
- Swimming: An excellent low-impact exercise that engages many muscle groups without putting significant stress on the knee joint. It helps maintain cardiovascular health and strength.
- Cycling: Stationary or outdoor cycling allows for controlled exertion and minimal stress on the knee joint. Vary the resistance and duration to adjust the intensity.
- Elliptical Training: This low-impact cardio machine provides a full-body workout with minimal stress on the knees.
Blood Flow and Inflammation Reduction Exercises
These exercises promote healing and reduce inflammation in the affected area.
- Light Massage: Gently massage the affected area with circular motions to increase blood flow.
- Heat Therapy: Applying a warm compress or taking a warm bath can help relax the muscles and increase blood flow.
- Ice Packs: Applying ice packs for 15-20 minutes at a time can help reduce inflammation and pain.
Progressive Overload Strategies
This table illustrates how to gradually increase the intensity of your exercises over time.
| Week | Exercise Type | Sets/Reps | Description |
|---|---|---|---|
| 1-2 | Quad Strengthening | 2 sets of 10-12 reps | Start with a manageable weight or resistance. Focus on proper form. |
| 3-4 | Quad Strengthening | 2 sets of 12-15 reps | Gradually increase the repetitions as tolerated. |
| 5-6 | Quad Strengthening | 3 sets of 12-15 reps | Increase the number of sets to further challenge the muscles. |
Exercise Progression and Modifications

As your patellar tendonitis heals, gradually increasing the intensity and duration of exercises is crucial. A well-structured progression allows your body to adapt to the demands of exercise without exacerbating pain. Modifications are essential for accommodating individual fitness levels and pain tolerances. Proper rest and recovery are equally important to prevent setbacks and promote healing.
Gradual Progression of Exercise Intensity and Duration
Begin with exercises that elicit minimal discomfort. As pain subsides and your body adapts, gradually increase the intensity and duration of the exercises. This could involve increasing the weight lifted, the number of repetitions, or the duration of the hold in a static stretch. A good rule of thumb is to increase the intensity or duration by no more than 10% per week.
For example, if you are performing 10 repetitions of a calf raise, increase to 11 repetitions the following week, and so on. Listen to your body; if you experience significant pain, reduce the intensity or duration.
Modifications for Different Fitness Levels and Pain Tolerances
Modifying exercises allows individuals with varying fitness levels and pain tolerances to participate safely. For example, if a seated calf raise is too difficult, you could perform them against a wall for support. If a standing calf raise causes pain, you can perform the exercise with one leg at a time, or reduce the repetitions. Resistance bands can also be used to reduce the load on the tendon.
Adjustments can be made to any exercise, ensuring that the exercise is challenging but not painful. The key is to find the right balance between challenging yourself and protecting the affected area.
Incorporating Rest and Recovery into the Exercise Routine
Rest and recovery are essential components of any exercise program, especially when dealing with tendonitis. Allowing your body adequate time to recover reduces the risk of re-injury and promotes healing. Rest periods between sets and rest days are important. Listen to your body and take rest days when needed. For example, if you feel fatigued or experience increased pain, don’t hesitate to take a rest day.
Importance of Listening to Your Body and Adjusting Exercises as Needed
Your body provides valuable feedback on how it’s responding to exercise. Paying close attention to any pain signals is crucial for preventing setbacks. Adjusting exercises as needed is key to a successful recovery. For instance, if you feel pain during a particular exercise, stop immediately and modify or substitute the exercise. This might involve changing the position, the intensity, or even replacing the exercise with a similar one that doesn’t aggravate the pain.
Strengthening exercises are crucial for patellar tendonitis recovery. Focus on exercises that target the quadriceps and hamstrings, but be sure to listen to your body. While exploring alternative remedies, it’s also worth considering bee pollen, which some believe has healing properties, though more research is needed. You can find out more about bee pollen and what to consider in this helpful article: bee pollen what should i know about it.
Ultimately, a balanced approach including physical therapy exercises and a well-rounded diet is key to managing patellar tendonitis.
Strategies for Preventing Exercise-Induced Pain Flare-Ups
To prevent pain flare-ups, warm up thoroughly before each exercise session. This helps prepare the muscles and tendons for the workout. Cool down afterward to gradually reduce the blood flow to the affected area, allowing for recovery. Consider using ice packs to help reduce inflammation. Maintaining proper form during exercises is vital.
Improper form can place excessive stress on the patellar tendon, potentially leading to pain flare-ups. Listen to your body’s signals; if you feel any pain, stop the exercise immediately.
Common Exercise Mistakes to Avoid
| Mistake | Explanation | Solution |
|---|---|---|
| Skipping warm-up | Lack of preparation can strain the tendon. | Perform 5-10 minutes of light cardio and dynamic stretching. |
| Using improper form | Incorrect technique puts undue stress on the tendon. | Seek guidance from a physical therapist or qualified professional. |
| Pushing through pain | Ignoring pain can worsen the injury. | Stop the exercise immediately and rest. |
| Overtraining | Excessive exercise can hinder recovery. | Adjust the intensity and duration of exercises based on your body’s response. |
| Insufficient rest | Lack of rest days inhibits recovery. | Incorporate rest days into your routine and listen to your body. |
Importance of Proper Warm-up and Cool-down
Proper warm-up and cool-down routines are crucial for preventing injuries and optimizing performance during exercises for patellar tendonitis. These preparatory and recovery phases are not merely optional additions but essential components of any exercise program. They prepare the body for the demands of exercise, reduce the risk of strains and tears, and promote the body’s natural recovery processes.
A well-structured routine will enhance the effectiveness of your exercises and contribute to a faster recovery.Effective warm-up and cool-down routines are essential for preventing injuries and promoting recovery. They prepare the body for the demands of exercise and facilitate the body’s natural recovery processes. This is particularly important for individuals with patellar tendonitis, as these routines help prevent further strain on the affected tendon.
Warm-up Routine Significance
A proper warm-up routine prepares the muscles and joints for the demands of exercise. It gradually increases blood flow to the working muscles, enhancing oxygen delivery and nutrient supply. This improved blood flow also helps reduce the risk of muscle strains and tears. A good warm-up routine prepares the body for the demands of exercise and improves performance.
Components of a Suitable Warm-up
A comprehensive warm-up routine typically involves a combination of activities. A general warm-up phase is followed by specific dynamic stretches for the targeted areas. This gradual increase in activity prepares the body for the exercises and helps prevent injuries.
- General Warm-up: This initial phase involves light cardio activities like brisk walking or jogging, lasting 5-10 minutes. This increases heart rate and blood flow to the muscles, preparing them for more strenuous activity. This preparatory phase is essential for improving blood circulation and increasing muscle temperature. A proper general warm-up helps the body to gradually adjust to the upcoming activity, minimizing the risk of injury and maximizing performance.
- Dynamic Stretching: Dynamic stretches involve controlled movements that mimic the exercises to be performed. This helps prepare the muscles and joints for the specific demands of the exercise routine. Examples include leg swings, arm circles, and torso twists. These movements enhance flexibility and range of motion, reducing the risk of muscle strains and promoting a smooth transition to more strenuous activity.
Dynamic Warm-up Exercises for the Knee
Dynamic exercises specifically target the knee and surrounding muscles, enhancing flexibility and preparing the joint for activity.
- Knee Circles: Slowly and gently circle the knee in both directions, increasing the range of motion gradually. This enhances joint mobility and reduces stiffness.
- Leg Swings: Perform forward and backward leg swings, focusing on maintaining a controlled and smooth motion. This helps improve flexibility and blood flow to the knee joint.
- Heel Slides: While maintaining a straight posture, slide one heel towards your glutes, feeling the stretch in the front of the thigh. This improves flexibility in the hip flexors and quads.
- Butt Kicks: Bring your heels towards your glutes in a rhythmic and controlled motion. This exercise improves the flexibility of the hamstrings.
Static Stretching Exercises
Static stretching involves holding a stretch for a specific duration. This helps improve flexibility and range of motion in the affected areas.
So, I’ve been researching exercises for patellar tendonitis, and it’s fascinating how seemingly unrelated health issues can impact recovery. For example, a lot of people with diabetes experience yeast infections, which can sometimes affect overall physical function, making exercises for patellar tendonitis even more challenging. Finding ways to manage both conditions is key, and understanding how they connect can help with targeted recovery.
Fortunately, there are plenty of resources available, and I’m continuing my research to find the best exercises for patellar tendonitis, especially given the importance of a holistic approach, and to help people better understand how factors like diabetes and yeast infections might affect recovery.
- Quadriceps Stretch: Hold onto a stable surface and pull one leg back, keeping the knee straight. Hold the stretch for 20-30 seconds. This stretches the quadriceps muscle group, enhancing flexibility and reducing muscle tension.
- Hamstring Stretch: Extend one leg straight in front of you and reach towards your toes. Hold the stretch for 20-30 seconds. This stretch targets the hamstrings and improves their flexibility.
- Calf Stretch: Place your hands against a wall or a sturdy surface, keeping one leg back and the other leg forward. Lean into the stretch, feeling the stretch in the calf muscle. Hold for 20-30 seconds. This targets the calf muscles and promotes flexibility.
Cool-down Routine
A cool-down routine gradually reduces the intensity of exercise, allowing the body to transition back to a resting state.
- Light Cardio: Engage in light cardio activities, such as walking or cycling, for 5-10 minutes. This helps gradually reduce heart rate and blood pressure, promoting blood circulation.
- Static Stretching: Hold static stretches for each of the affected areas (quadriceps, hamstrings, and calves) for 20-30 seconds each. This improves flexibility and reduces muscle soreness.
Comprehensive Warm-up and Cool-down Routine
| Activity | Duration | Description |
|---|---|---|
| Warm-up | 10-15 minutes | Includes brisk walking, arm circles, leg swings, and knee circles. |
| Dynamic Stretches | 5-7 minutes | Focus on knee mobility and surrounding muscle groups, such as quadriceps, hamstrings, and calves. |
| Workout | As needed | Perform exercises for patellar tendonitis, as prescribed. |
| Cool-down | 10-15 minutes | Includes light cardio (walking) and static stretching (quadriceps, hamstrings, calves). |
Additional Considerations and Support
Patellar tendonitis, often a frustrating condition, requires a multifaceted approach encompassing not only targeted exercises but also crucial lifestyle adjustments and supportive measures. Proper footwear, body weight management, and pain management strategies all play significant roles in alleviating symptoms and promoting healing. Understanding these factors can greatly enhance the effectiveness of your treatment plan.
Proper Footwear
Choosing appropriate footwear is essential for supporting the knees and preventing further stress on the patellar tendon. Shoes with adequate cushioning and arch support can absorb impact, reducing the force transmitted through the knee joint. Look for shoes with a firm heel counter to provide stability and prevent excessive rolling inward or outward of the foot. Consider running shoes or athletic shoes designed for specific activities, like running or jumping, as they often provide superior support compared to everyday shoes.
Properly fitted footwear can significantly reduce the risk of re-injury and promote faster healing.
Supportive Knee Braces
Knee braces can provide additional support and stability to the knee joint, particularly during activities that put high stress on the patellar tendon. Braces can help to stabilize the patella and reduce the strain on the tendon, potentially alleviating pain and inflammation. Compression braces can aid in reducing swelling, while hinged braces can help to control patellar tracking.
However, it’s crucial to choose a brace that fits correctly and is appropriate for the specific activity. Over-the-counter braces are often sufficient for mild cases, while custom-fit braces might be recommended for more severe or persistent pain.
Body Weight and Alignment
Maintaining a healthy body weight is crucial for reducing stress on the patellar tendon. Excess weight puts extra pressure on the knees, increasing the risk of developing or exacerbating patellar tendonitis. Maintaining a healthy weight through a balanced diet and regular exercise can significantly lessen the strain on the joint and promote healing. Good posture and alignment also play a role.
Proper alignment minimizes stress on the tendon, preventing further irritation and inflammation. Consider consulting a physical therapist for personalized advice on proper posture and movement patterns.
Pain and Inflammation Management
Effective pain and inflammation management strategies are crucial for improving quality of life and promoting healing. Rest, ice, compression, and elevation (RICE) can help reduce pain and swelling. Over-the-counter pain relievers, such as ibuprofen or naproxen, can also help manage discomfort. However, it’s important to consult a doctor before taking any medication, especially if you have underlying health conditions.
In some cases, more aggressive approaches, such as corticosteroid injections, may be considered. These should only be used under the guidance of a healthcare professional.
Nutrition and Hydration
Proper nutrition and hydration are vital for overall health and tissue repair. A balanced diet rich in fruits, vegetables, and protein can provide the nutrients needed for optimal healing. Adequate hydration is essential for maintaining joint lubrication and facilitating nutrient transport to the tissues. Drinking plenty of water throughout the day can help reduce inflammation and promote overall well-being.
A diet rich in collagen-boosting foods might also be beneficial.
Physical Therapy
Physical therapy plays a crucial role in managing patellar tendonitis. A physical therapist can develop a personalized exercise program to strengthen the muscles around the knee, improve flexibility, and address any biomechanical imbalances. They can also provide guidance on proper movement patterns and techniques to reduce stress on the patellar tendon. This specialized care can significantly contribute to long-term recovery and prevention of future injuries.
Supportive Knee Brace Examples
| Brace Type | Benefits |
|---|---|
| Compression Brace | Reduces swelling and provides mild support. |
| Hinged Brace | Controls patellar tracking and offers greater stability. |
| Wraparound Brace | Provides adjustable support and compression around the knee. |
| Patellar Stabilizing Brace | Specifically designed to stabilize the patella and reduce irritation. |
Illustrative Examples and Visual Aids: Exercises For Patellar Tendonitis

Visual aids and practical examples are crucial for understanding and effectively applying exercises for patellar tendonitis. Seeing proper form and progressing through exercises safely are essential for avoiding further injury and maximizing results. This section provides clear demonstrations of key aspects, from warm-up routines to exercise progressions and self-massage techniques, making the entire process more accessible and understandable.
Warm-up Routine
A proper warm-up is essential to prepare the muscles and tendons for exercise, reducing the risk of injury. A dynamic warm-up, which involves controlled movements that gradually increase the range of motion and blood flow to the targeted area, is highly recommended. This is crucial for preparing the patellar tendon for the demands of exercise. A good warm-up helps prevent injuries and enhances performance.
- Light Cardio: Begin with 5-10 minutes of low-impact cardio, such as brisk walking or stationary cycling, to increase blood flow throughout the body.
- Dynamic Stretching: Perform dynamic stretches that focus on the quadriceps, hamstrings, and calf muscles. Examples include leg swings (forward, backward, and side-to-side), torso twists, and hip circles. Hold each stretch for 2-3 seconds and repeat 10-15 times for each exercise. These movements prepare the muscles for the workout.
- Specific Patellar Tendon Exercises: Incorporate specific exercises for the patellar tendon, such as gentle toe raises and heel slides, performed in a controlled manner. These help prepare the tendon for more demanding exercises.
Proper Exercise Form
Maintaining proper form during exercises is crucial for preventing further injury and maximizing effectiveness. Incorrect form can place excessive stress on the patellar tendon, potentially worsening the condition. Visualizing the proper form is essential to execute the exercises effectively.
Example: Single-Leg Calf Raises
Stand on one leg, maintaining a stable posture with the other leg slightly behind for balance. Keep the core engaged and the standing knee aligned with the ankle. Slowly raise up onto the ball of the foot, contracting the calf muscle, and lower back down slowly. Repeat 10-15 times, maintaining proper form throughout the exercise. Focus on controlled movement and avoid bouncing.
Exercise Progression Chart
A structured progression chart helps gradually increase the intensity and complexity of exercises, preventing overuse injuries. It ensures that the exercises remain challenging but not overly demanding for the injured tendon.
| Week | Exercise | Repetitions | Sets |
|---|---|---|---|
| 1 | Wall Slides | 10-15 | 2-3 |
| 2 | Single-Leg Calf Raises (against wall for support) | 10-15 | 2-3 |
| 3 | Single-Leg Calf Raises (no support) | 10-15 | 2-3 |
| 4 | Single-Leg Calf Raises with resistance band | 8-12 | 2-3 |
Ice Therapy
Applying ice therapy can help reduce inflammation and pain associated with patellar tendonitis. Proper application is crucial for effectiveness and avoiding skin irritation.
Wrap ice in a thin towel to prevent direct skin contact. Apply ice for 15-20 minutes at a time, several times a day. Avoid applying ice for longer than 20 minutes to prevent tissue damage.
Foam Roller Self-Massage
Self-massage using a foam roller can help improve blood flow, release muscle tension, and promote recovery. This is a helpful technique for addressing muscle imbalances that can contribute to patellar tendonitis.
Position the foam roller beneath the quadriceps muscle. Apply moderate pressure and roll slowly back and forth, focusing on areas of tightness or tenderness. Hold each area for 30-60 seconds. Always use caution and listen to your body.
Exercise Descriptions and Benefits
Understanding the specific exercises and their benefits is crucial for creating a targeted and effective treatment plan.
- Quadriceps Sets: These exercises strengthen the quadriceps muscle group, which plays a crucial role in supporting the patella and preventing tendon strain. Regular quadriceps sets help to improve the strength and stability of the surrounding muscles, reducing stress on the patellar tendon.
- Hamstring Stretches: Stretching the hamstrings can help alleviate tightness and imbalance, which can contribute to patellar tendonitis. Improving hamstring flexibility helps to maintain proper biomechanics during activities and reduces strain on the tendon.
Closing Notes
In conclusion, this guide provides a thorough understanding of exercises for patellar tendonitis, encompassing all essential aspects of effective management. From comprehending the condition itself to implementing progressive exercise routines, and emphasizing the crucial roles of warm-up, cool-down, and recovery, we’ve explored a comprehensive strategy. By incorporating these strategies into your recovery plan, you can effectively manage your pain, improve your knee function, and return to your desired level of activity.
Remember, consistency and proper form are key to achieving optimal results.