Subclinical hypothyroidism and the heart: This complex interplay between a subtle thyroid condition and cardiovascular health is a crucial area of study. Many people may have this condition without realizing it, and the impact on their heart can be significant. This post delves into the intricacies of how subclinical hypothyroidism affects the heart, exploring its prevalence, mechanisms, and potential risks.
We’ll also look at strategies for early detection, effective management, and ultimately, protecting cardiovascular health.
The connection between a slightly underactive thyroid and heart issues is intriguing. We’ll examine the physiological pathways that link these two, and discover how subtle changes in thyroid hormones can have a surprising impact on the cardiovascular system. Understanding this relationship is key to proactive health management and early intervention.
Introduction to Subclinical Hypothyroidism: Subclinical Hypothyroidism And The Heart
Subclinical hypothyroidism is a condition where thyroid hormone levels are slightly below the normal range, but not low enough to cause the full range of symptoms associated with overt hypothyroidism. It’s a relatively common condition, often detected during routine blood tests rather than presenting with noticeable symptoms. Understanding its link to cardiovascular health is crucial for early detection and appropriate management.The physiological mechanisms connecting subclinical hypothyroidism and the heart are complex.
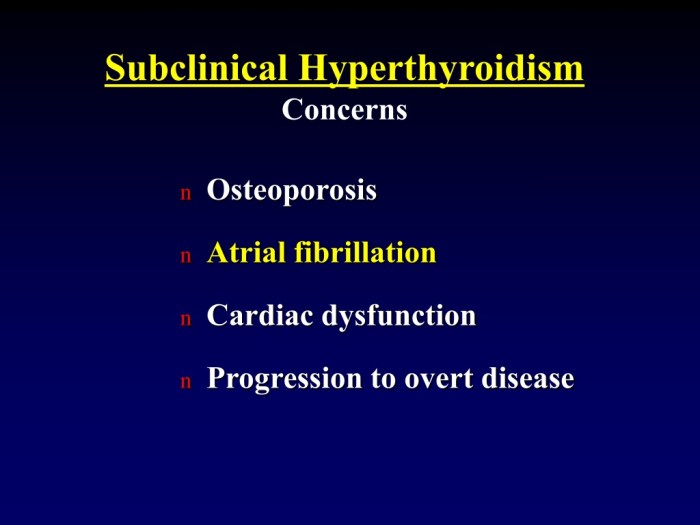
Reduced thyroid hormone levels can lead to a cascade of effects impacting the heart. For example, lower thyroid hormone can alter the body’s metabolism, affecting cholesterol and lipid profiles. This can increase the risk of atherosclerosis, a hardening and narrowing of the arteries, and subsequent cardiovascular issues. Furthermore, subclinical hypothyroidism may influence the heart’s rhythm and contractility, contributing to a higher risk of heart failure and other cardiovascular complications.
These effects are often subtle and don’t immediately manifest as noticeable symptoms, highlighting the importance of regular check-ups and blood tests.The prevalence of subclinical hypothyroidism varies depending on factors like age and geographic location, but it is estimated to affect a significant portion of the population, potentially even reaching 10% or more in certain demographics. The prevalence of subclinical hypothyroidism in the general population is a significant public health concern.
Early detection and management are essential to minimize potential cardiovascular complications and improve overall health outcomes.Early detection and management of subclinical hypothyroidism are paramount, particularly concerning cardiovascular health. Left unaddressed, the subtle but persistent effects on the heart can increase the risk of heart disease. Prompt diagnosis and appropriate treatment can mitigate these risks and improve long-term cardiovascular well-being.
Individuals with risk factors for cardiovascular disease or those experiencing symptoms like fatigue or unexplained weight changes should discuss the possibility of subclinical hypothyroidism with their healthcare provider.
Comparison of Subclinical and Overt Hypothyroidism
A crucial aspect of understanding subclinical hypothyroidism involves contrasting it with overt hypothyroidism. This comparison highlights the differences in symptom presentation and potential impact on the cardiovascular system.
| Characteristic | Subclinical Hypothyroidism | Overt Hypothyroidism |
|---|---|---|
| Thyroid-Stimulating Hormone (TSH) Levels | Elevated TSH, but within the upper limit of normal range. | Elevated TSH, significantly above the normal range. |
| Symptoms | Often asymptomatic, or symptoms are mild and nonspecific (e.g., fatigue, mild weight gain, constipation). | More pronounced symptoms, including fatigue, significant weight gain, cold intolerance, dry skin, hair loss, slowed heart rate, and muscle weakness. |
| Impact on the Heart | Increased risk of subtle cardiac changes, such as dyslipidemia, increased heart rate variability, and subtle alterations in cardiac function, but usually not clinically significant. | More significant cardiac effects, including bradycardia (slow heart rate), potential for heart failure, and increased risk of atrial fibrillation. |
| Treatment | Treatment is often individualized based on risk factors and symptoms, potentially including thyroid hormone replacement therapy. | Treatment typically involves thyroid hormone replacement therapy to restore normal thyroid hormone levels. |
This table illustrates the gradual progression from subclinical to overt hypothyroidism. The subtle nature of subclinical hypothyroidism emphasizes the importance of routine screenings and monitoring, particularly in individuals at higher risk.
Cardiovascular Effects of Subclinical Hypothyroidism
Subclinical hypothyroidism, a condition characterized by slightly elevated thyroid-stimulating hormone (TSH) levels but normal free thyroid hormone levels, is increasingly recognized as a potential risk factor for cardiovascular issues. While the symptoms are often subtle, the impact on the cardiovascular system can be significant and warrants careful monitoring. Understanding these effects is crucial for early detection and appropriate management.The mechanisms linking subclinical hypothyroidism and cardiovascular dysfunction are multifaceted and not fully understood.
However, it’s widely accepted that alterations in thyroid hormone levels can disrupt various physiological processes, impacting cardiovascular function. These disruptions, although subtle in the early stages, can gradually contribute to an increased risk of cardiovascular events over time.
Specific Cardiovascular Changes
Subclinical hypothyroidism is associated with a range of cardiovascular changes. These include alterations in blood pressure, heart rate, lipid profiles, and potentially increased inflammation. These changes, while often subtle, can contribute to a greater risk of developing cardiovascular diseases over time.
Blood Pressure
Subclinical hypothyroidism is frequently associated with elevated blood pressure. Studies have shown a correlation between higher TSH levels and increased systolic and diastolic blood pressure. This effect may be linked to the influence of thyroid hormones on the renin-angiotensin-aldosterone system, contributing to vascular constriction and fluid retention.
Heart Rate
While not always a consistent finding, some studies suggest a subtle increase in resting heart rate in individuals with subclinical hypothyroidism. This effect may be due to the influence of thyroid hormones on cardiac contractility and autonomic nervous system function.
Lipid Profiles
Subclinical hypothyroidism often results in alterations in lipid profiles, characterized by elevated total cholesterol, LDL cholesterol (bad cholesterol), and decreased HDL cholesterol (good cholesterol). This dyslipidemia may contribute to a higher risk of atherosclerosis and cardiovascular disease.
Impact on Cardiovascular Risk Factors
| Cardiovascular Risk Factor | Impact of Subclinical Hypothyroidism |
|---|---|
| Blood Pressure | Often elevated systolic and diastolic pressure |
| Heart Rate | Potentially elevated resting heart rate |
| Lipids | Elevated total cholesterol, LDL, and decreased HDL |
| Inflammation | Potentially increased inflammatory markers |
A recent meta-analysis highlighted a statistically significant association between subclinical hypothyroidism and an increased risk of cardiovascular events, including heart attacks and strokes.
Relationship with Cardiovascular Events
Several studies have demonstrated a link between subclinical hypothyroidism and an increased risk of cardiovascular events. This increased risk may be due to the cumulative effects of subtle cardiovascular changes, such as elevated blood pressure, altered lipid profiles, and increased inflammation, over time. For instance, a study in a large cohort of patients found that individuals with subclinical hypothyroidism had a higher incidence of coronary artery disease compared to those with normal thyroid function.
Risk Factors and Modifiable Factors
Subclinical hypothyroidism, while often asymptomatic, can significantly impact cardiovascular health. Understanding the factors that increase the risk of developing cardiovascular issues associated with this condition is crucial for preventative strategies. Identifying modifiable risk factors allows for targeted interventions to minimize the potential harm. This section delves into the interplay between age, gender, other contributing factors, and lifestyle choices, highlighting actionable steps for improved cardiovascular well-being in individuals with subclinical hypothyroidism.Age, gender, and genetics are intrinsic factors that contribute to the risk of subclinical hypothyroidism and its associated cardiovascular consequences.
Older individuals are more prone to developing the condition, possibly due to hormonal changes and physiological aging processes. Furthermore, women are disproportionately affected, likely due to hormonal fluctuations throughout their lives, particularly during pregnancy and menopause. Genetic predispositions also play a role, increasing susceptibility to both subclinical hypothyroidism and cardiovascular issues.
Subclinical hypothyroidism can subtly impact heart health, potentially increasing risks. While a healthy gut is crucial for overall well-being, understanding how to cleanse your colon safely is important for managing potential digestive issues that could influence thyroid function. A balanced approach to gut health, like following a reputable guide on how to cleanse your colonsafely , might help optimize your system and ultimately support a healthier heart in the context of subclinical hypothyroidism.
It’s always wise to consult a doctor for personalized advice, especially when dealing with thyroid conditions.
Age-Related Risk, Subclinical hypothyroidism and the heart
Older adults frequently experience a decline in thyroid function, which can increase their vulnerability to subclinical hypothyroidism. This is often coupled with other age-related changes, such as hypertension, atherosclerosis, and increased inflammation, all of which can synergistically exacerbate cardiovascular risk. For example, a 70-year-old woman with a family history of heart disease and a recent diagnosis of subclinical hypothyroidism may be at significantly higher risk for developing cardiovascular events than a younger individual without these risk factors.
Gender-Related Risk
Women are more susceptible to subclinical hypothyroidism than men, potentially due to hormonal fluctuations. Studies suggest that women experience a higher incidence of thyroid disorders throughout their lives, particularly during pregnancy and the post-menopausal period. The interplay between estrogen levels and thyroid function may contribute to this increased risk. A 50-year-old woman experiencing menopausal symptoms and diagnosed with subclinical hypothyroidism might face a heightened risk of cardiovascular problems compared to a similarly aged man.
Other Risk Factors
Several other factors contribute to the overall risk of subclinical hypothyroidism and its impact on cardiovascular health. These include:
- Iodine Deficiency: Insufficient iodine intake, crucial for thyroid hormone production, can lead to hypothyroidism. Areas with limited iodine in their diet frequently experience higher rates of subclinical hypothyroidism.
- Autoimmune Conditions: Individuals with autoimmune diseases, such as Hashimoto’s thyroiditis, are at a higher risk for subclinical hypothyroidism. The presence of an autoimmune condition can create a cascade of health concerns, increasing the likelihood of adverse cardiovascular outcomes.
- Certain Medications: Some medications can interfere with thyroid hormone production, leading to hypothyroidism. Individuals taking certain medications, such as lithium or amiodarone, may be more susceptible to subclinical hypothyroidism.
Lifestyle Factors and Cardiovascular Effects
Lifestyle factors significantly influence the severity of cardiovascular effects associated with subclinical hypothyroidism. A diet lacking essential nutrients, excessive stress, and a sedentary lifestyle can exacerbate the condition. Conversely, adopting a healthy lifestyle can mitigate the risk.
- Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins, combined with adequate iodine intake, can support thyroid function and overall cardiovascular health. Conversely, a diet high in processed foods, saturated fats, and refined sugars can contribute to inflammation and exacerbate cardiovascular risk in individuals with subclinical hypothyroidism.
- Stress Management: Chronic stress can negatively impact both thyroid function and cardiovascular health. Stress-reducing activities, such as yoga, meditation, and spending time in nature, can positively impact overall health in individuals with subclinical hypothyroidism.
- Physical Activity: Regular physical activity can improve cardiovascular health by lowering blood pressure, improving lipid profiles, and reducing inflammation. A sedentary lifestyle can negatively impact cardiovascular health, regardless of thyroid status.
Risk Factor Table
| Risk Factor | Potential Impact on Cardiovascular Health |
|---|---|
| Age | Increased risk of cardiovascular disease due to physiological changes and increased prevalence of other risk factors. |
| Gender (Female) | Potentially higher risk due to hormonal fluctuations throughout life. |
| Iodine Deficiency | Compromised thyroid function, increasing vulnerability to cardiovascular problems. |
| Autoimmune Conditions | Increased risk of both subclinical hypothyroidism and cardiovascular complications. |
| Certain Medications | Interference with thyroid hormone production, potentially increasing cardiovascular risk. |
| Unhealthy Diet | Increased inflammation, adverse lipid profiles, and elevated blood pressure, exacerbating cardiovascular risk. |
| Chronic Stress | Negative impact on thyroid function and cardiovascular health. |
| Sedentary Lifestyle | Compromised cardiovascular health, regardless of thyroid status. |
Mitigation Strategies
Addressing modifiable risk factors is essential for mitigating cardiovascular risks in patients with subclinical hypothyroidism. Regular monitoring of thyroid function, adherence to treatment plans, and a healthy lifestyle are crucial.
Modifiable Lifestyle Factors
- Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins, along with sufficient iodine intake, supports optimal thyroid function and cardiovascular health.
- Stress Management Techniques: Incorporating stress-reducing activities, such as yoga, meditation, or spending time in nature, promotes overall well-being and can positively impact thyroid function.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking, swimming, or cycling, can improve cardiovascular health, reduce blood pressure, and improve lipid profiles.
- Smoking Cessation: Smoking is a significant cardiovascular risk factor, and quitting can significantly improve cardiovascular health.
Diagnostic and Management Strategies
Understanding subclinical hypothyroidism and its potential cardiovascular impact requires a careful approach to diagnosis and management. A proactive strategy, combining blood tests with lifestyle modifications, is often the most effective way to address the condition and mitigate potential risks. Early detection and tailored interventions can significantly improve outcomes for patients at risk.
Diagnostic Methods
Diagnosing subclinical hypothyroidism involves a systematic evaluation, primarily relying on blood tests to measure thyroid function. The most crucial tests are those that assess thyroid-stimulating hormone (TSH) levels and free thyroxine (T4) levels. Elevated TSH levels, coupled with normal T4 levels, often indicate subclinical hypothyroidism. Other assessments may include checking thyroid antibodies, such as anti-thyroid peroxidase (TPO) antibodies and anti-thyroglobulin antibodies, which can provide insights into the underlying cause of the condition.
Subclinical hypothyroidism can sometimes affect the heart, leading to various issues. One potential symptom is calf pain, which can stem from a number of different factors. Understanding the causes of calf pain and treatment options is crucial for proper diagnosis and management, as explored in detail on this page: causes of calf pain and treatment options.
Ultimately, recognizing these potential connections is key to ensuring comprehensive care for those with subclinical hypothyroidism and associated heart health concerns.
Management Strategies
Effective management of subclinical hypothyroidism often involves a combination of hormone replacement therapy and lifestyle modifications. Hormone replacement therapy, typically with levothyroxine, may be considered in certain situations, particularly when symptoms are present or when the elevated TSH levels are significantly high. Lifestyle modifications, such as adopting a balanced diet rich in iodine and maintaining a healthy weight, play a supportive role in managing the condition.
Individualized treatment plans are crucial, as the decision to initiate hormone replacement therapy often depends on the patient’s specific risk factors and symptoms.
Treatment Options and Cardiovascular Effects
| Treatment Option | Potential Effects on Cardiovascular Health | Considerations |
|---|---|---|
| Levothyroxine (hormone replacement therapy) | Potential reduction in cardiovascular risk factors like elevated cholesterol and blood pressure. However, long-term studies are needed to definitively determine the effects on cardiovascular outcomes. | Individualized dosage is critical to avoid potential side effects and optimize thyroid hormone levels. Careful monitoring is essential to adjust the dosage as needed. |
| Lifestyle modifications (diet, exercise, stress management) | These modifications can have a positive impact on cardiovascular health by improving overall well-being and reducing risk factors. | Lifestyle changes should be viewed as a complementary approach to medication, not a replacement for it. |
| No treatment (observation) | Monitoring is crucial to detect any progression to overt hypothyroidism or worsening cardiovascular risk factors. | Patients with minimal risk factors and no symptoms may be suitable for close observation. Regular follow-up is essential. |
Close Monitoring and Follow-Up
Regular monitoring of thyroid function tests and cardiovascular risk factors is vital in managing subclinical hypothyroidism. Patients should undergo periodic check-ups to assess TSH and T4 levels and to identify any potential cardiovascular complications. This allows for timely intervention if necessary. The frequency of follow-up appointments will depend on individual factors, including the severity of the condition, presence of symptoms, and other health conditions.
Individualized Treatment Plans
“An individualized treatment plan, considering both thyroid function and cardiovascular health, is essential for patients with subclinical hypothyroidism.”
Tailoring treatment to the specific needs of each patient is critical. Factors such as age, existing cardiovascular conditions, and overall health status must be taken into account when developing a management strategy. This approach ensures the best possible outcome for each patient. For example, a patient with a family history of heart disease might require more aggressive monitoring and potential earlier intervention compared to a patient without such risk factors.
Subclinical hypothyroidism can subtly affect heart health, increasing the risk of certain issues. A healthy diet, including a handful of walnuts every day for health benefits, like this article suggests , might help manage some of these risks. These nutritious nuts are packed with antioxidants and healthy fats, which can contribute to overall cardiovascular well-being, ultimately benefiting those with subclinical hypothyroidism.
Illustrative Case Studies
Understanding subclinical hypothyroidism’s impact on the heart requires examining real-world examples. These case studies illustrate the diagnosis, management, and potential progression of cardiovascular issues associated with this condition. They also highlight how different management strategies can affect outcomes.
Case Study 1: Diagnosis and Management of Subclinical Hypothyroidism with Cardiovascular Issues
A 55-year-old female presented with fatigue, mild weight gain, and constipation. Routine blood tests revealed mildly elevated TSH levels and slightly reduced free T4 levels, indicative of subclinical hypothyroidism. Further assessment included an echocardiogram, which showed mild left ventricular hypertrophy and diastolic dysfunction. These findings suggested a potential link between the subclinical hypothyroidism and early cardiovascular changes.
Treatment with levothyroxine, a synthetic thyroid hormone, was initiated at a low dose and gradually titrated based on TSH and free T4 levels. Regular monitoring of TSH, free T4, and cardiovascular markers, including blood pressure, lipid profile, and echocardiographic parameters, was implemented. The patient showed significant improvement in her symptoms and a trend toward normalization of cardiovascular parameters within six months of treatment.
Case Study 2: Progression of Cardiovascular Problems in Untreated Subclinical Hypothyroidism
A 62-year-old male with a history of hypertension and dyslipidemia was diagnosed with subclinical hypothyroidism. Due to perceived lack of significant symptoms, treatment with levothyroxine was delayed. Over the next three years, the patient experienced a progressive increase in blood pressure, an elevation in LDL cholesterol, and a deterioration in echocardiographic parameters. A repeat echocardiogram revealed significant left ventricular hypertrophy and reduced ejection fraction, indicating the development of more advanced cardiovascular disease.
This case highlights the potential for untreated subclinical hypothyroidism to contribute to the progression of pre-existing cardiovascular risk factors and exacerbate existing conditions.
Case Study 3: Successful Management Strategy for Combined Conditions
A 48-year-old female with a history of subclinical hypothyroidism and pre-existing coronary artery disease underwent comprehensive risk factor modification. Her treatment plan included levothyroxine therapy to normalize thyroid function, alongside lifestyle interventions such as dietary modifications, regular exercise, and stress management techniques. Simultaneously, she received standard management for her coronary artery disease, including medications for hypertension and dyslipidemia.
This integrated approach resulted in significant improvements in her thyroid function, blood pressure, lipid profile, and overall cardiovascular health, as measured by improvements in exercise tolerance and reductions in cardiovascular risk markers. The case demonstrates that comprehensive management, addressing both subclinical hypothyroidism and pre-existing cardiovascular conditions, can lead to positive outcomes.
Impact of Management Approaches on Cardiovascular Outcomes
Different management strategies can significantly influence cardiovascular outcomes in patients with subclinical hypothyroidism. Early intervention with levothyroxine, combined with lifestyle modifications, often leads to improvements in cardiovascular risk markers. Delayed or inadequate treatment can result in the progression of cardiovascular issues, potentially leading to more severe conditions. For patients with pre-existing cardiovascular disease, the management of both conditions concurrently, through a multidisciplinary approach, is crucial for achieving optimal outcomes.
Summary of Key Findings from Case Studies
| Case Study | Condition | Management | Outcome |
|---|---|---|---|
| 1 | Subclinical Hypothyroidism, Mild Cardiovascular Changes | Levothyroxine, Monitoring | Improved Symptoms, Trend toward Normalization of Cardiovascular Parameters |
| 2 | Subclinical Hypothyroidism, Untreated | Delayed Treatment | Progression of Cardiovascular Issues (Hypertension, Dyslipidemia, Left Ventricular Hypertrophy) |
| 3 | Subclinical Hypothyroidism, Pre-existing Coronary Artery Disease | Levothyroxine, Lifestyle Modifications, Standard Management for CAD | Significant Improvements in Thyroid Function, Blood Pressure, Lipid Profile, Cardiovascular Health |
Future Research Directions
Unraveling the intricate link between subclinical hypothyroidism and cardiovascular health requires further investigation. Current research suggests a potential association, but more in-depth studies are crucial to confirm causality and fully understand the mechanisms involved. This exploration into future research directions will highlight key areas demanding attention, potential innovative approaches, and the need for larger, more comprehensive studies to solidify our understanding of this complex relationship.The current body of evidence hints at a correlation between subclinical hypothyroidism and increased cardiovascular risk.
However, the exact nature of this relationship and the underlying mechanisms remain partially obscured. Further research is essential to clarify the impact of subclinical hypothyroidism on specific cardiovascular parameters, including blood pressure, lipid profiles, and endothelial function. This will allow for more precise risk stratification and tailored management strategies.
Identifying Predictive Biomarkers
Understanding the subtle shifts in the body’s response to subclinical hypothyroidism is critical for developing early detection strategies. Future research should focus on identifying specific biomarkers that could predict the development of cardiovascular complications in individuals with subclinical hypothyroidism. These biomarkers could include novel inflammatory markers, specific protein or hormone levels, or even genetic predispositions. This proactive approach would allow for early intervention and potentially mitigate the long-term impact on cardiovascular health.
For example, a study might investigate the role of specific inflammatory cytokines in patients with subclinical hypothyroidism and their association with atherosclerosis progression.
Optimizing Diagnostic Tools
Current diagnostic methods for subclinical hypothyroidism may not capture the full spectrum of the disease’s impact on cardiovascular health. Further research should explore novel diagnostic tools that provide a more comprehensive assessment of cardiovascular risk factors in individuals with subclinical hypothyroidism. These could involve advanced imaging techniques, such as echocardiography or cardiac MRI, to evaluate subtle structural or functional changes in the heart.
Alternatively, novel blood tests targeting specific aspects of cardiovascular function could provide more detailed insights. For instance, assessing endothelial function through flow-mediated dilation could help determine cardiovascular risk in this population.
Evaluating Treatment Strategies
Determining the optimal treatment strategies for subclinical hypothyroidism, specifically with regards to cardiovascular health, requires further investigation. Research should explore whether current treatment options for subclinical hypothyroidism effectively reduce cardiovascular risk factors. Moreover, research should investigate whether additional therapeutic interventions, such as specific medications or lifestyle modifications, may further mitigate cardiovascular risk. For example, studies could examine the effect of adding statins to standard hypothyroidism treatment on lipid profiles and cardiovascular outcomes in patients with subclinical hypothyroidism.
Longitudinal Studies and Multicenter Trials
A significant gap in our knowledge is the long-term impact of subclinical hypothyroidism on cardiovascular health. Longitudinal studies that follow individuals with subclinical hypothyroidism over several years are essential to assess the long-term cardiovascular outcomes and establish a clearer link between the condition and cardiovascular events. Multicenter studies with large sample sizes are crucial to validate findings across different populations and enhance the generalizability of results.
These studies should incorporate detailed cardiovascular risk assessments, including blood pressure monitoring, lipid profiles, and imaging studies, to provide a comprehensive understanding of the long-term consequences of subclinical hypothyroidism.
Last Recap
In conclusion, subclinical hypothyroidism and the heart are intricately connected. This post has highlighted the subtle yet significant impact this condition can have on cardiovascular health. Early detection, tailored management plans, and a proactive approach to lifestyle choices are vital for minimizing risks and optimizing long-term heart health in individuals with subclinical hypothyroidism. Further research is crucial to refine our understanding and improve patient outcomes.