Stages of osteoarthritis of the hip, a debilitating condition affecting millions, progresses through distinct phases. Understanding these stages is crucial for effective management and improving quality of life. This guide delves into the various stages, exploring their symptoms, treatment options, and impact on daily activities.
From the initial subtle signs to the more advanced and debilitating stages, this comprehensive overview will help you navigate the complexities of hip osteoarthritis. We’ll cover everything from the underlying mechanisms to the lifestyle changes that can help slow the progression of the disease.
Introduction to Hip Osteoarthritis: Stages Of Osteoarthritis Of The Hip
Hip osteoarthritis, often referred to as degenerative joint disease of the hip, is a chronic condition characterized by the breakdown and progressive deterioration of the cartilage within the hip joint. This leads to pain, stiffness, and reduced mobility, significantly impacting the quality of life for those affected. The underlying mechanisms involve a complex interplay of factors, including genetics, age, and lifestyle choices.The progression of hip osteoarthritis involves the gradual loss of cartilage, a smooth tissue that cushions the joint surfaces.
As cartilage wears away, the underlying bone surfaces rub against each other, leading to inflammation, pain, and the formation of bone spurs (osteophytes). This process can be accelerated by various factors, such as repetitive stress on the joint, obesity, and previous joint injuries.
Types of Hip Osteoarthritis
Hip osteoarthritis can be categorized into primary and secondary types, based on the underlying causes. Primary osteoarthritis arises without any identifiable predisposing factors, while secondary osteoarthritis is linked to pre-existing conditions or injuries. The differing etiologies can significantly impact treatment strategies.
Risk Factors for Hip Osteoarthritis
Several factors increase the risk of developing hip osteoarthritis. Age is a significant contributor, with the risk increasing as individuals get older. Genetics play a role, as some individuals are predisposed to the condition due to inherited factors. Obesity and repetitive stress on the hip joint, such as from certain occupations or sports activities, also contribute to the development of the disease.
Previous joint injuries, such as fractures or dislocations, can also increase the risk of developing osteoarthritis.
Comparison of Primary and Secondary Hip Osteoarthritis
| Characteristic | Primary Hip Osteoarthritis | Secondary Hip Osteoarthritis |
|---|---|---|
| Cause | Unknown; no specific identifiable cause | Linked to a pre-existing condition (e.g., previous injury, hip dysplasia, inflammatory arthritis) or repetitive stress |
| Prevalence | More common in older adults | Can occur at any age, but often associated with pre-existing conditions |
| Risk Factors | Age, genetics, family history | Previous hip injury, hip dysplasia, inflammatory arthritis, repetitive stress, obesity |
| Treatment | Similar to secondary, but may require a deeper understanding of the underlying factors to determine if a predisposition exists | Treatment focuses on addressing the underlying cause and managing symptoms. |
Stages of Hip Osteoarthritis
Hip osteoarthritis, a degenerative joint disease, progresses through distinct stages. Understanding these stages is crucial for effective management and treatment planning. Early recognition of symptoms and progression allows for proactive interventions, potentially slowing disease progression and improving quality of life. Early diagnosis and appropriate management strategies can significantly impact the long-term outcomes for individuals affected by this condition.
Stages of Hip Osteoarthritis Progression
Hip osteoarthritis typically progresses through four stages, each characterized by increasing severity of joint damage and associated symptoms. This gradual deterioration leads to a decline in function and increased pain, impacting daily activities.
Understanding the stages of osteoarthritis in the hip is crucial for effective management. Early stages often involve mild pain and stiffness, but as the condition progresses, symptoms intensify. Interestingly, some treatments for other conditions, like the innovative use of excimer laser for psoriasis excimer laser for psoriasis , are also being explored for potential benefits in managing joint pain.
Ultimately, ongoing research and personalized care plans remain vital for navigating the different stages of hip osteoarthritis.
- Stage 1: Minimal or No Joint DamageIn this initial stage, minimal changes occur within the hip joint. While some early signs of cartilage breakdown might be present, they are not readily apparent or significantly impactful on daily activities. Pain and stiffness may be mild and intermittent, often mistaken for other conditions. Symptoms are often subtle and easily ignored. This phase is frequently identified through routine checkups or during specific diagnostic testing, highlighting the importance of regular medical evaluations, especially for individuals with risk factors.
- Stage 2: Mild Joint DamageAs the disease progresses, the cartilage in the hip joint begins to deteriorate more noticeably. In this stage, the joint experiences minor damage, leading to mild pain and stiffness. Symptoms may increase with prolonged activity or weight-bearing. Patients might experience occasional discomfort during specific movements, such as getting out of a chair or climbing stairs. Physical findings may show subtle signs of joint space narrowing on imaging tests.
Understanding the stages of hip osteoarthritis is crucial for managing the condition effectively. While dealing with this, it’s fascinating to consider how some people experience a completely different kind of discomfort, like the fear of belly buttons, also known as omphalophobia. This phobia, as detailed in this informative article on fear of belly buttons omphalophobia definition symptoms causes treatment , highlights the wide range of anxieties that can impact us.
Ultimately, recognizing the various stages of hip osteoarthritis is key to proper treatment and pain management.
Individuals may experience a reduced range of motion, and pain may be more frequent and noticeable, particularly after periods of inactivity.
- Stage 3: Moderate Joint DamageSignificant cartilage loss and joint damage are evident in this stage. Pain and stiffness become more pronounced, impacting daily activities. Patients may experience pain even at rest. Movement becomes more restricted, and individuals may have difficulty performing tasks that involve weight-bearing or repetitive motions. Physical findings show significant joint space narrowing and bone spurs (osteophytes) on imaging.
This stage often requires more aggressive management strategies to maintain mobility and function. For example, a patient might require regular physical therapy sessions to improve their joint flexibility and strength.
- Stage 4: Severe Joint DamageIn the final stage, significant cartilage loss has occurred, and the joint is severely damaged. Pain and stiffness are constant and debilitating, impacting nearly all aspects of daily life. Individuals may experience significant limitations in mobility and have difficulty with basic tasks. Physical findings reveal extensive joint space narrowing, severe bone spurs, and possible joint deformity. This stage often requires surgical intervention, such as a hip replacement, to restore function and alleviate pain.
For example, a patient might experience excruciating pain even with minimal movement, severely affecting their ability to walk or perform basic household chores.
Symptom and Physical Findings Comparison
The severity of symptoms and physical findings varies across the different stages. Mild discomfort and stiffness in the early stages contrast sharply with the constant and debilitating pain experienced in the later stages.
| Stage | Pain | Stiffness | Impact on Daily Activities |
|---|---|---|---|
| 1 | Mild, intermittent | Minimal | Minimal to no impact |
| 2 | Moderate, occasional | Mild, after activity | Slight impact on some activities |
| 3 | Moderate to severe, persistent | Significant, even at rest | Significant impact on most daily activities |
| 4 | Severe, constant, debilitating | Extreme, limiting mobility | Unable to perform most daily activities independently |
Symptoms and Diagnosis
Understanding the symptoms and diagnostic methods for hip osteoarthritis is crucial for early intervention and effective management. Accurate diagnosis allows for personalized treatment plans tailored to the specific needs of each patient. This section delves into the common symptoms associated with each stage, the diagnostic tools used, and the role of imaging and physical examinations in determining the stage of the disease.
Common Symptoms of Hip Osteoarthritis
Symptoms of hip osteoarthritis often develop gradually, increasing in severity as the disease progresses. Early detection is key to managing the condition effectively. Patients may experience subtle discomfort initially, which can easily be attributed to other factors. This gradual progression makes it essential to be aware of the subtle signs and symptoms.
- Stage 1 (Minimal): Mild pain, typically after prolonged activity or weight-bearing. Discomfort might be described as stiffness or aching in the groin, hip, or buttock. It is often intermittent and easily relieved with rest.
- Stage 2 (Mild): Pain becomes more persistent and may occur with less activity. Stiffness is more noticeable, particularly in the morning or after periods of inactivity. Patients may experience a decreased range of motion in the hip joint.
- Stage 3 (Moderate): Pain intensifies and is present even during everyday activities. Stiffness is more pronounced and limits the ability to perform tasks such as walking, climbing stairs, or getting in and out of chairs. Patients may experience a noticeable limp. Night pain is also more common.
- Stage 4 (Severe): Significant pain is present even at rest. Stiffness is severe, severely limiting mobility. A noticeable limp is almost always present. Pain may radiate down the leg, and daily activities become nearly impossible without significant assistance.
Diagnostic Methods for Hip Osteoarthritis
Accurate diagnosis of hip osteoarthritis relies on a combination of methods. A thorough assessment by a healthcare professional is crucial.
- Patient History: The physician will inquire about the onset, duration, and characteristics of the pain. Details about the patient’s lifestyle, activities, and any previous injuries to the hip will be considered. This provides a crucial understanding of the patient’s condition.
- Physical Examination: A physical examination assesses the range of motion, joint stability, and presence of tenderness or swelling in the hip. This examination provides valuable insights into the structural integrity and functionality of the hip joint.
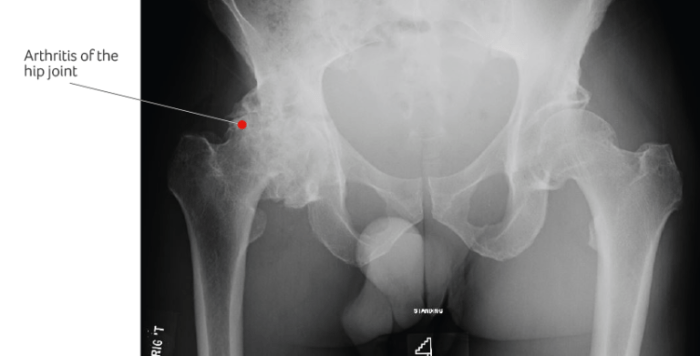
- Imaging Techniques: X-rays are essential for visualizing the joint space narrowing, bone spurs (osteophytes), and other structural changes. MRI scans provide detailed images of the soft tissues surrounding the hip joint, which can help assess cartilage damage and inflammation. These imaging techniques help in evaluating the extent of damage to the hip joint.
Role of Imaging in Staging
Imaging plays a crucial role in evaluating the extent of joint damage and determining the stage of osteoarthritis. X-rays are typically the initial imaging modality used.
| Stage | Typical X-ray Findings | MRI Findings (potential) |
|---|---|---|
| Stage 1 | Minimal or no visible changes | Possible early signs of cartilage thinning or inflammation |
| Stage 2 | Slight narrowing of the joint space, possible early osteophytes (bone spurs) | Cartilage thinning more noticeable; some synovitis (inflammation of the lining of the joint) |
| Stage 3 | Significant narrowing of the joint space, prominent osteophytes, and possible sclerosis (bone thickening) | More extensive cartilage damage; increased synovitis; possible meniscal tears |
| Stage 4 | Severe narrowing of the joint space, extensive osteophytes, and significant sclerosis. Possible joint subluxation or dislocation. | Severe cartilage loss; extensive synovitis; joint effusion (fluid buildup); significant structural damage. |
“A comprehensive diagnostic approach combining patient history, physical examination, and imaging studies is essential for accurate staging of hip osteoarthritis.”
Treatment Options and Management Strategies
Managing hip osteoarthritis involves a multifaceted approach tailored to the individual’s stage of the disease and overall health. Effective treatment aims to alleviate pain, improve function, and maintain quality of life. A combination of strategies, including lifestyle modifications, medication, physical therapy, and potentially surgery, can significantly impact the progression and management of hip osteoarthritis.
Non-Surgical Treatment Options
Non-surgical treatments are often the first line of defense in managing hip osteoarthritis, especially in the early stages. These strategies focus on reducing pain, improving joint function, and slowing disease progression.
- Physical Therapy: Physical therapy plays a crucial role in improving strength, flexibility, and range of motion around the hip joint. Exercises are designed to target specific muscles supporting the hip, helping to reduce pain and improve stability. Physical therapists can also teach patients proper body mechanics to minimize stress on the affected joint, such as exercises to improve posture and gait.
- Medications: Pain relievers, such as over-the-counter analgesics like ibuprofen and acetaminophen, can help manage pain and inflammation. In some cases, stronger prescription medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and potentially corticosteroid injections, may be necessary for more significant pain relief. These medications can help improve mobility and reduce inflammation in the affected joint. It is crucial to consult a physician to determine the appropriate medication and dosage.
- Lifestyle Modifications: Weight management is critical in managing hip osteoarthritis. Excess weight puts added stress on the hip joint, accelerating the progression of the disease. Maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce pain and improve function. Regular exercise, including low-impact activities like swimming or walking, helps strengthen muscles around the hip and maintain joint mobility.
Avoiding activities that exacerbate pain is also important.
Surgical Treatment Options
Surgical intervention may be considered for individuals with advanced stages of hip osteoarthritis where non-surgical treatments are no longer sufficient to manage pain and improve function.
- Hip Resurfacing: This procedure involves replacing the damaged articular cartilage surface of the hip joint with a metal cap and a plastic liner. It’s typically suitable for younger, active individuals with early to moderate stages of osteoarthritis. A key benefit is preserving more of the natural hip structure compared to a total hip replacement.
- Total Hip Replacement: In this procedure, the damaged hip joint is replaced with an artificial joint (prosthesis). It is a more extensive procedure but can significantly improve pain and function in advanced stages of osteoarthritis. This is often the preferred surgical option for patients with severe pain, significant joint damage, or when other treatments have failed. Long-term success depends on proper post-operative care and adherence to physical therapy recommendations.
Treatment Comparison
The choice of treatment depends on several factors, including the stage of the disease, the patient’s overall health, activity level, and preferences. Non-surgical treatments are often tried first to avoid the potential risks associated with surgery.
| Stage | Non-Surgical Treatments | Surgical Treatments | Comparison |
|---|---|---|---|
| Early | Physical therapy, medication, lifestyle modifications | Hip resurfacing (in select cases) | Non-surgical methods are often sufficient in the early stages, with surgery reserved for severe cases or if non-surgical options fail. |
| Moderate | Physical therapy, medication, lifestyle modifications, corticosteroid injections | Hip resurfacing or partial hip replacement | Non-surgical options remain important, but surgical options become more viable to address pain and improve function. |
| Advanced | Physical therapy, medication, corticosteroid injections | Total hip replacement | Surgical intervention is usually necessary in advanced stages due to significant joint damage and decreased function. |
Impact on Quality of Life
Hip osteoarthritis, a degenerative joint disease, significantly impacts a person’s overall well-being. The pain, stiffness, and limited mobility associated with the condition can profoundly affect daily activities, emotional state, and social interactions. Understanding these multifaceted impacts is crucial for effective management and support.
Physical Function and Independence
Hip osteoarthritis progressively diminishes physical function. Initial stages might involve mild discomfort during prolonged standing or walking. As the disease advances, simple tasks like climbing stairs, getting in and out of a car, or even walking short distances become increasingly challenging. This gradual loss of mobility can lead to reduced independence in performing everyday activities. Individuals may need assistance with personal care tasks or household chores, impacting their ability to live independently.
The degree of impact varies greatly based on the severity of the disease and individual factors.
Emotional and Psychological Consequences, Stages of osteoarthritis of the hip
The chronic pain and limitations associated with hip osteoarthritis can take a toll on emotional well-being. Experiences of frustration, anxiety, and depression are not uncommon. The constant struggle with physical limitations and the need to adapt to a changing lifestyle can be emotionally taxing. Moreover, the social isolation that can result from reduced mobility can exacerbate feelings of loneliness and isolation.
Recognizing and addressing these emotional and psychological impacts is essential for comprehensive care.
Social Implications
Hip osteoarthritis can restrict social participation. Reduced mobility often limits involvement in social activities, like attending gatherings, participating in hobbies, or traveling. This can lead to social isolation and a diminished sense of connection with others. The impact on social life is further influenced by the individual’s support system and available resources. Maintaining social connections, even when limited, is crucial for emotional well-being.
Strategies to Maintain Quality of Life
Maintaining quality of life during each stage of hip osteoarthritis requires a multi-faceted approach. Regular exercise, tailored to the individual’s abilities and pain levels, is essential for preserving muscle strength and flexibility. Physical therapy plays a key role in developing strategies for managing pain and improving mobility. Proper nutrition and maintaining a healthy weight can help reduce stress on the joints.
Mental health support can assist in managing emotional challenges and improving coping mechanisms. Active participation in support groups can provide valuable emotional and practical support.
Assistive Devices
Assistive devices can significantly improve quality of life at various stages of hip osteoarthritis. In early stages, a walking cane or a supportive shoe insert can provide stability and reduce pain during ambulation. As the condition progresses, mobility aids like walkers or rollators can help maintain independence in navigating everyday environments. Adaptive equipment for daily living, such as raised toilet seats or grab bars, can facilitate personal care tasks and prevent falls.
The choice of assistive devices should be individualized based on the specific needs and limitations of each person.
Prevention and Risk Reduction
Hip osteoarthritis, a debilitating condition, can significantly impact a person’s quality of life. Fortunately, proactive measures can help prevent or reduce the risk of developing this disease, and even delay or mitigate its progression. Understanding the contributing factors and implementing lifestyle adjustments can make a substantial difference in maintaining healthy hip joints.
Lifestyle Modifications for Prevention
Adopting healthy lifestyle choices is crucial in preventing hip osteoarthritis. These modifications can not only delay the onset of the condition but also reduce the severity of symptoms if it does develop. A holistic approach encompassing diet, exercise, and overall well-being is essential for long-term joint health.
- Regular Exercise: Engaging in regular physical activity, including low-impact exercises like swimming, cycling, and walking, strengthens muscles around the hip joint, reducing stress on the cartilage. These exercises improve joint stability and flexibility, making the hips more resilient to wear and tear. A consistent exercise routine is vital for maintaining joint health and preventing stiffness.
- Maintaining a Healthy Weight: Excess weight places significant strain on the hip joints. Losing even a moderate amount of weight can substantially lessen the load on these delicate structures. Weight management programs, often incorporating dietary changes and exercise, are effective in preventing and managing hip osteoarthritis. For instance, a person who loses 10 pounds can reduce the load on their hips by approximately 40 pounds.
- Balanced Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients that support joint health. Adequate intake of vitamins and minerals, such as vitamin C and glucosamine, is vital for cartilage maintenance. Avoiding excessive consumption of processed foods, sugary drinks, and saturated fats is equally important.
- Proper Posture and Body Mechanics: Maintaining good posture and employing proper body mechanics when lifting heavy objects or performing daily activities can significantly reduce stress on the hip joints. This includes lifting with your legs, not your back, and using proper lifting techniques.
Maintaining Joint Health
Regular attention to joint health is crucial in preventing and managing hip osteoarthritis. This encompasses various strategies to bolster the resilience and well-being of the hip joints.
Understanding the stages of osteoarthritis in the hip is crucial for effective management. While diet isn’t a cure-all, incorporating the ten best foods for IBS, like those highlighted in this comprehensive guide the ten best foods for ibs , can potentially alleviate some symptoms that often accompany the later stages of hip OA. Ultimately, managing pain and improving mobility during different stages requires a multi-faceted approach.
- Warm-up and Cool-down: Prior to any physical activity, warming up the hip joints with gentle stretches prepares them for the workout. Similarly, cooling down after exercise allows the muscles to relax, promoting better recovery. These simple steps can reduce the risk of injury and promote overall joint health.
- Adequate Hydration: Staying well-hydrated ensures the cartilage receives the necessary lubrication to function optimally. Drinking plenty of water supports overall joint health and reduces stiffness.
- Supplementation: Consult a healthcare professional before taking any supplements, as certain supplements, like glucosamine and chondroitin, may help support cartilage health. However, their effectiveness in preventing or treating osteoarthritis is not definitively proven in all cases. Their use should be discussed with a physician to assess their suitability.
Importance of Early Diagnosis and Intervention
Early detection and intervention are paramount in managing hip osteoarthritis effectively. Early diagnosis enables prompt treatment and lifestyle adjustments, potentially slowing disease progression and improving outcomes.
- Regular Check-ups: Regular check-ups with a healthcare professional allow for early identification of potential issues, including early signs of hip osteoarthritis. This enables timely intervention, which can significantly impact the course of the disease.
- Seeking Professional Advice: Individuals experiencing hip pain or stiffness should consult a healthcare professional for proper diagnosis and treatment options. Early diagnosis enables prompt intervention, potentially slowing disease progression and improving outcomes.
Weight Management’s Role
Weight management plays a pivotal role in preventing and managing hip osteoarthritis. Reducing excess weight minimizes the strain on the hip joints, potentially slowing the progression of the disease.
Maintaining a healthy weight is crucial in preventing hip osteoarthritis. Losing even a moderate amount of weight can substantially lessen the load on the hip joints.
Illustrations and Visual Aids
Understanding hip osteoarthritis requires a visual approach to grasp the progressive nature of the condition. Visual aids, such as diagrams and illustrations, can effectively convey complex anatomical changes and treatment outcomes. This section delves into various visual representations that highlight the stages of osteoarthritis, the impact on the hip joint, and the effects of different treatment strategies.
Diagrammatic Progression of Osteoarthritis
Visualizing the progression of osteoarthritis is crucial for understanding its impact on the hip joint. A diagram showing the normal hip joint, alongside stages of osteoarthritis, would be highly beneficial. The diagram should progressively illustrate the narrowing of the joint space, the formation of bone spurs (osteophytes), and the thickening of the cartilage. The illustration should include labels highlighting the affected structures and the increasing severity of the condition at each stage.
Anatomy of the Hip Joint in Relation to Osteoarthritis
A detailed diagram of the hip joint, highlighting the key components such as the femur, acetabulum, cartilage, and surrounding ligaments, is essential. This diagram should clearly depict the normal structure of the joint and how these structures are affected by osteoarthritis. The diagram can be color-coded to distinguish between healthy and diseased areas, clearly illustrating the loss of cartilage and the development of bone spurs.
This visual representation will help patients and healthcare professionals understand the intricate anatomy of the hip joint and the specific locations of the degenerative changes.
Impact of Bone Loss on the Hip Joint at Different Stages
A series of diagrams showcasing the hip joint at different stages of osteoarthritis would illustrate the impact of bone loss. The diagrams should visually depict the progressive narrowing of the joint space, the loss of cartilage, and the formation of osteophytes at increasing severity levels. The diagrams should be labeled with the stage of osteoarthritis and the corresponding amount of bone loss.
Examples of stages with different degrees of bone loss, and the impact on joint mobility, can be added.
Demonstration of Treatment Modalities on Joint Structure
Visual aids can effectively demonstrate the effects of different treatment modalities on joint structure. A series of diagrams depicting the hip joint before and after treatments like physical therapy, medication, or surgery can be beneficial. For example, a diagram showing the improvement in joint space after physical therapy, or a comparison of the hip joint before and after joint replacement surgery.
This visualization can help patients understand the potential benefits and outcomes of various treatment options.
Diagram of Stages of Hip Osteoarthritis and Corresponding Symptoms
A comprehensive diagram depicting the stages of hip osteoarthritis and their corresponding symptoms is vital. This diagram should be a flow chart or a table, showcasing the stage of osteoarthritis, the associated symptoms, and the severity levels. The table can include the typical pain levels, mobility limitations, and other symptoms that typically present at each stage. This diagram can be used as a quick reference tool to assist in the diagnosis and management of hip osteoarthritis.
It will be especially useful for patients to track their own symptoms and discuss them with their healthcare provider.
Outcome Summary
In conclusion, the stages of hip osteoarthritis present a spectrum of challenges, impacting individuals in diverse ways. Understanding the progression, symptoms, and available treatments is vital for effective management and maintaining a good quality of life. This guide offers a roadmap to navigate this complex condition, empowering individuals to make informed decisions and seek appropriate support.




