Signs of diabetes diagnosing type 2 diabetes is a critical health concern impacting millions globally. This in-depth exploration delves into the early warning signs, diagnostic procedures, risk factors, symptoms, and crucial prevention strategies. Understanding the subtle cues and diagnostic processes is paramount for early intervention and effective management.
We’ll cover everything from common symptoms like increased thirst and frequent urination to the role of blood tests and lifestyle factors in diagnosis. Furthermore, we’ll examine the key risk factors and potential complications, equipping you with valuable knowledge to proactively address this widespread health challenge.
Early Warning Signs
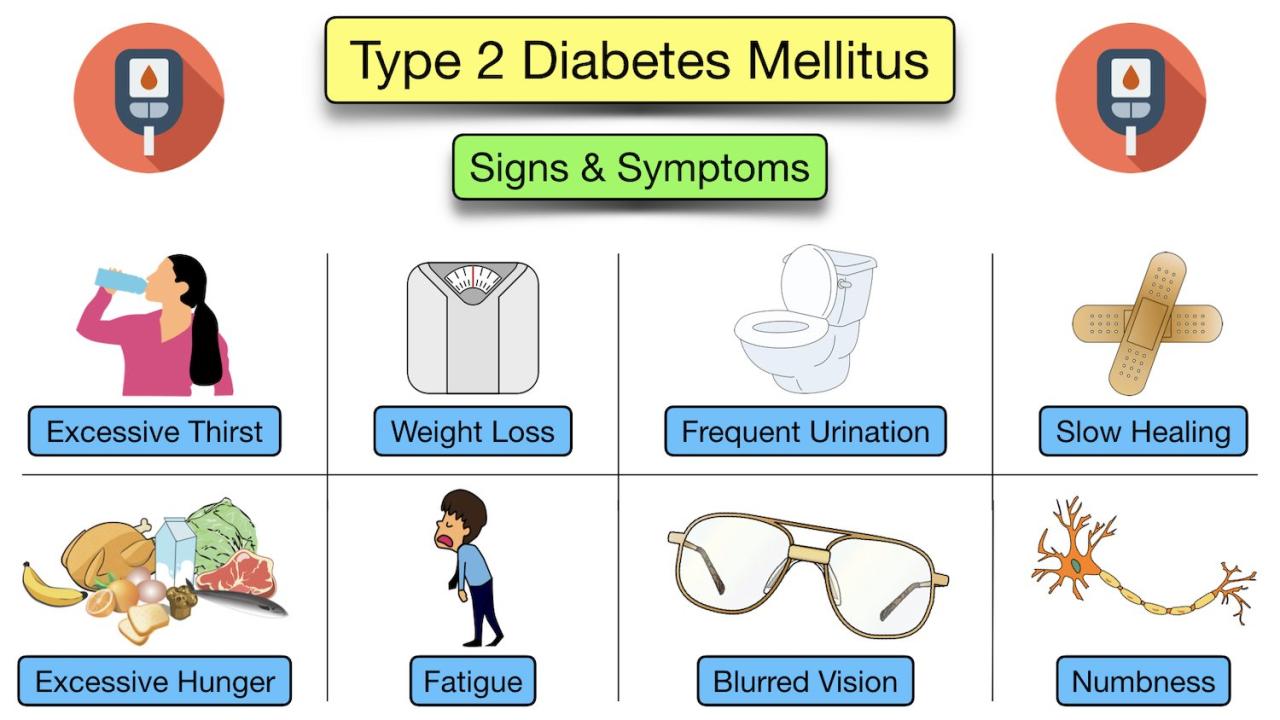
Understanding the early warning signs of elevated blood sugar levels is crucial for timely diagnosis and management of type 2 diabetes. While some signs are more common and noticeable, others might be subtle, requiring a heightened awareness. Recognizing these variations, particularly in men and women, can significantly impact early intervention and improve overall health outcomes.
Common Early Signs
Early indicators of elevated blood sugar levels often present subtly, and sometimes mimic other health concerns. Recognizing these common signs can help individuals seek timely medical attention. These signs often involve a combination of symptoms, rather than a single isolated event.
- Frequent urination, especially at night (polyuria): This is a classic symptom as the kidneys work overtime to filter excess glucose from the blood, leading to increased urine production. This can disrupt sleep and lead to dehydration.
- Increased thirst (polydipsia): The frequent urination associated with elevated blood sugar levels often leads to dehydration, prompting the body to signal a need for more fluids.
- Unexplained weight loss: While seemingly contradictory to other symptoms, the body may be breaking down fat and muscle tissue to compensate for the inability to effectively utilize glucose for energy, resulting in weight loss.
- Blurred vision: Changes in blood sugar levels can affect the lens of the eye, leading to temporary blurring or other vision disturbances.
- Slow-healing sores or cuts: High blood sugar can impair blood circulation and the body’s ability to repair tissues, leading to prolonged healing times for wounds.
Less Common, but Potentially Serious Indicators
Beyond the common signs, certain less frequent indicators might signal a more severe underlying issue. These often require immediate medical attention.
- Recurrent infections: Frequent infections, such as yeast infections or urinary tract infections, can be a sign of impaired immune function due to high blood sugar levels. The body’s ability to fight off infections diminishes when blood sugar is not properly regulated.
- Fatigue and weakness: A persistent feeling of tiredness and weakness can be a result of the body’s inability to utilize glucose for energy efficiently.
- Numbness or tingling in the hands or feet (peripheral neuropathy): Prolonged high blood sugar can damage nerves, particularly in the extremities, leading to these sensations. This is a serious complication that requires immediate medical attention.
Differences in Manifestation Between Men and Women
While many early signs are similar across genders, subtle variations exist.
- Men might experience more pronounced fatigue and decreased libido, alongside potential erectile dysfunction. Women might experience more frequent yeast infections.
Severity and Impact Comparison
| Sign | Severity | Impact | Potential Risk Factors |
|---|---|---|---|
| Frequent urination (polyuria) | Mild | Disruption of sleep, dehydration | High blood sugar levels, fluid intake, diet |
| Increased thirst (polydipsia) | Mild | Dehydration, discomfort | High blood sugar levels, fluid intake, diet |
| Unexplained weight loss | Mild to Moderate | Malnutrition, energy imbalance | High blood sugar levels, inadequate caloric intake, underlying conditions |
| Blurred vision | Mild | Impaired vision, safety concerns | High blood sugar levels, eye health |
| Slow-healing sores/cuts | Moderate | Increased risk of infection, potential complications | High blood sugar levels, impaired circulation |
| Recurrent infections | Moderate to Severe | Impaired immune function, potential complications | High blood sugar levels, compromised immune system |
| Fatigue and weakness | Mild to Moderate | Reduced productivity, overall discomfort | High blood sugar levels, lack of energy, underlying conditions |
| Numbness/tingling (peripheral neuropathy) | Severe | Chronic pain, nerve damage, mobility issues | High blood sugar levels, prolonged duration of elevated blood sugar |
Diagnosing Type 2 Diabetes
Navigating the path to a diabetes diagnosis involves a combination of factors. It’s not a single test, but a comprehensive assessment considering your medical history, lifestyle, and physical examination. Understanding the process empowers individuals to actively participate in their healthcare and ensure accurate identification of the condition.Diagnosing type 2 diabetes requires a multi-faceted approach that goes beyond a single blood test.
The process involves careful consideration of various elements to arrive at an accurate and comprehensive diagnosis. This detailed examination ensures the best possible outcomes and facilitates appropriate management strategies.
Diagnostic Procedures
A comprehensive diagnostic process for type 2 diabetes is critical. It involves a series of steps to confirm a diagnosis, which begins with a thorough medical history review. This information, coupled with blood tests and physical examinations, helps healthcare professionals determine the presence and extent of the condition.
Role of Blood Tests
Blood tests play a crucial role in diagnosing type 2 diabetes. These tests measure key indicators that provide insights into the body’s metabolic state.
- Fasting Plasma Glucose (FPG): A fasting plasma glucose (FPG) test measures the level of glucose in the blood after an overnight fast. A result of 126 mg/dL or higher on two separate tests indicates a diagnosis of diabetes.
- Oral Glucose Tolerance Test (OGTT): An OGTT assesses how the body processes glucose after consuming a sugary drink. This test is particularly useful when the fasting glucose levels are borderline. A two-hour glucose level of 200 mg/dL or higher suggests diabetes.
- Hemoglobin A1c (HbA1c): HbA1c reflects the average blood sugar levels over the past two to three months. An HbA1c level of 6.5% or higher on two separate tests suggests diabetes. This test provides a long-term perspective on glucose control.
Importance of Medical History
A complete medical history is essential for diagnosing type 2 diabetes. A detailed account of the patient’s health history provides context for the current situation and helps identify potential risk factors.
- Family history: A family history of diabetes significantly increases an individual’s risk. Knowing if close relatives have the condition can help predict the likelihood of developing type 2 diabetes.
- Lifestyle factors: A review of lifestyle factors such as diet, exercise, and weight can help determine if there are contributing elements. An individual who maintains a sedentary lifestyle and consumes a diet high in sugar and processed foods is at a greater risk.
- Other health conditions: Pre-existing conditions like hypertension, high cholesterol, and cardiovascular issues can influence the development of diabetes. Knowing about such conditions helps to formulate a holistic approach to the diagnosis.
Contribution of Lifestyle Factors
Lifestyle factors are key components in the diagnosis of type 2 diabetes. Understanding the role of diet, exercise, and weight management is crucial. Individuals with a history of poor diet, lack of exercise, and obesity are more susceptible to developing the condition.
- Diet: A diet high in processed foods, sugar, and saturated fats can lead to insulin resistance, increasing the risk of type 2 diabetes. Examples include sugary drinks, fast food, and excessive intake of processed carbohydrates.
- Exercise: Regular physical activity helps the body use insulin effectively. A sedentary lifestyle significantly increases the risk of developing type 2 diabetes. A consistent exercise routine can significantly reduce the likelihood of the disease.
- Weight Management: Obesity is a major risk factor for type 2 diabetes. Maintaining a healthy weight through a balanced diet and regular exercise is crucial in preventing and managing the condition. A person with a BMI of 30 or higher has a significantly higher risk of developing diabetes.
Significance of Physical Examinations
Physical examinations are an integral part of the diagnostic process. These examinations help assess overall health and identify associated conditions. A thorough physical examination can reveal signs of insulin resistance, such as high blood pressure, elevated cholesterol, or increased waist circumference.
- Blood Pressure: High blood pressure is often linked to type 2 diabetes. Measurements during the physical examination can help assess the risk.
- Cholesterol Levels: Elevated cholesterol levels are another risk factor. The physical examination may include blood tests to evaluate cholesterol levels.
- Waist Circumference: Increased waist circumference can indicate abdominal fat, a significant risk factor for type 2 diabetes. The physical examination may include measurements to assess waist circumference.
Risk Factors and Predisposition
Understanding the factors that increase your likelihood of developing type 2 diabetes is crucial for proactive health management. This knowledge empowers you to make informed lifestyle choices and seek appropriate medical interventions if needed. Recognizing your risk factors allows you to focus on prevention strategies and potentially delay or even prevent the onset of the disease.Type 2 diabetes is not solely a result of lifestyle choices; genetic predisposition plays a significant role.
While you can’t change your genes, understanding your family history and personal genetic makeup can help you make informed decisions about managing your risk. This section explores the key risk factors, lifestyle influences, genetic predisposition, and common comorbidities associated with type 2 diabetes, offering a comprehensive overview for proactive health management.
Key Risk Factors
Numerous factors contribute to the development of type 2 diabetes. Age, family history, and ethnicity are often significant indicators of increased risk. Certain medical conditions, such as high blood pressure and high cholesterol, also raise the likelihood of developing the disease.
Lifestyle Factors
Unhealthy lifestyle choices significantly increase the risk of type 2 diabetes. Maintaining a healthy weight, engaging in regular physical activity, and consuming a balanced diet are crucial for mitigating risk. Lack of physical activity, poor dietary habits, and excess weight are strong predictors of type 2 diabetes development.
Spotting the signs of diabetes, especially when diagnosing type 2, can be tricky. While there’s no one-size-fits-all approach, common symptoms include frequent urination and increased thirst. This is often similar to the adage “feed a cold, starve a fever,” which, in the context of health, doesn’t apply to managing diabetes. However, recognizing these symptoms early is crucial for prompt diagnosis and management.
Understanding the nuances of each symptom is key to getting the right care.
Genetic Predisposition
A family history of type 2 diabetes substantially increases your risk. If close relatives have the disease, your chances of developing it also increase. Genetic predisposition is a complex interplay of multiple genes, making it challenging to isolate specific genes responsible for increased risk. However, the presence of these genes can increase your susceptibility to developing the disease if combined with lifestyle factors.
Common Comorbidities
Type 2 diabetes is often associated with other health problems. Conditions like high blood pressure, heart disease, and stroke are frequently linked to diabetes. These comorbidities can complicate management and highlight the importance of comprehensive health assessments.
Relationship Between Risk Factors and Likelihood of Development
| Risk Factor | Description | Likelihood of Development |
|---|---|---|
| Family History | Presence of type 2 diabetes in close relatives (parents, siblings, grandparents). | Increased |
| Age | The risk generally increases with age, particularly after age 45. | Increased |
| Ethnicity | Certain ethnic groups have a higher predisposition to type 2 diabetes. | Increased |
| Obesity | Excess body weight, particularly abdominal fat, is a significant risk factor. | Increased |
| Physical Inactivity | Lack of regular exercise and a sedentary lifestyle. | Increased |
| Poor Diet | High intake of processed foods, sugary drinks, and unhealthy fats. | Increased |
| High Blood Pressure | Chronically elevated blood pressure. | Increased |
| High Cholesterol | Elevated levels of LDL (“bad”) cholesterol. | Increased |
| Gestational Diabetes | Diabetes during pregnancy. | Increased |
Symptoms and Complications
Type 2 diabetes, while often insidious in its early stages, can manifest with a range of symptoms and lead to serious long-term complications. Understanding these symptoms and potential issues is crucial for early detection and effective management. Early intervention can significantly reduce the risk of severe complications.The progression of type 2 diabetes often involves a gradual decline in the body’s ability to regulate blood sugar levels.
This gradual shift can result in a variety of symptoms, ranging from seemingly minor discomfort to more pronounced and concerning health issues. Monitoring these symptoms is essential for individuals at risk and those already diagnosed with type 2 diabetes.
Common Symptoms
Many people experience subtle symptoms initially, which may be attributed to other conditions. Recognizing these early warning signs can facilitate prompt diagnosis and management. Common symptoms include frequent urination, especially at night, increased thirst, and unexplained weight loss. These symptoms arise from the body’s attempt to eliminate excess glucose through urination.
Long-Term Complications
Type 2 diabetes can significantly impact various organ systems, leading to a spectrum of long-term complications. These complications often develop gradually and can range from minor inconveniences to life-threatening conditions. Some of the most prevalent complications include cardiovascular disease, nerve damage (neuropathy), kidney damage (nephropathy), eye damage (retinopathy), and foot problems. The severity of these complications depends on the duration and control of blood sugar levels.
Correlation Between Blood Sugar Control and Health Issues
Maintaining consistent blood sugar control is paramount in mitigating the risk of long-term complications. Poor blood sugar control, or hyperglycemia, can lead to significant health problems across multiple organ systems. For example, prolonged high blood sugar levels can damage blood vessels, increasing the risk of heart disease, stroke, and other cardiovascular issues. Furthermore, uncontrolled blood sugar can harm the nerves, leading to neuropathy, and the kidneys, potentially causing kidney disease.
Figuring out the signs of diabetes, especially type 2, can be tricky. You might notice increased thirst or frequent urination, which can be confusing. Sometimes, those symptoms are related to other things, like your menstrual cycle. Did you know that you might burn more calories during your period? Check out this fascinating article to learn more about how your body changes during that time do you burn more calories on your period.
However, persistent thirst and frequent urination, along with unexplained weight loss or fatigue, are still strong indicators that you should get checked out for potential diabetes.
Impact on Body Systems
Type 2 diabetes’s impact extends beyond a single body system. The disease can affect the circulatory system, leading to cardiovascular problems. It can damage the nerves, resulting in neuropathy, affecting sensation and movement. The kidneys can be impaired, potentially leading to kidney disease or failure. Damage to the eyes can result in retinopathy, potentially causing vision loss.
Foot problems are also common due to nerve damage and poor blood flow, increasing the risk of infection and ulcers. The impact is far-reaching and underscores the importance of proper management.
Symptoms, Complications, and Blood Sugar Levels
| Symptom | Description | Blood Sugar Level | Potential Complications |
|---|---|---|---|
| Frequent Urination | Increased need to urinate, especially at night | Elevated (often above 180 mg/dL after meals) | Dehydration, kidney problems |
| Increased Thirst | Persistent feeling of dryness and thirst | Elevated (often above 180 mg/dL after meals) | Dehydration, kidney problems |
| Unexplained Weight Loss | Loss of weight without intentional dieting or exercise | Elevated (often consistently above target range) | Metabolic disturbances, cardiovascular problems |
| Blurred Vision | Difficulty focusing or seeing clearly | Elevated (often consistently above target range) | Retinopathy, potentially leading to vision loss |
| Slow-healing sores | Wounds that take longer than usual to heal | Elevated (often consistently above target range) | Neuropathy, poor circulation, increased risk of infection |
Prevention and Management
Type 2 diabetes, while manageable, requires proactive strategies for prevention and effective management. Early intervention and lifestyle changes are crucial to reducing the risk of developing the condition and improving the overall well-being of those diagnosed. This section delves into the key aspects of prevention and management, including lifestyle modifications, medication, meal planning, and exercise.
Strategies for Preventing Type 2 Diabetes
Preventing type 2 diabetes hinges on understanding and addressing the risk factors. A healthy lifestyle, including a balanced diet and regular physical activity, significantly reduces the likelihood of developing the condition. Maintaining a healthy weight, managing stress, and getting sufficient sleep contribute to overall well-being and lower the risk of insulin resistance, a key factor in type 2 diabetes.
Importance of Lifestyle Modifications
Lifestyle modifications are fundamental to preventing and managing type 2 diabetes. A balanced diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, plays a crucial role in maintaining healthy blood sugar levels and weight. Reducing stress through relaxation techniques and prioritizing sleep are equally important aspects of lifestyle management.
One of the less-obvious signs of diabetes, especially when diagnosing type 2, can be changes in your bowel movements. For example, have you noticed your stool has become pale or clay-colored lately? This could be a symptom of a variety of things, including potential liver or pancreatic issues, which could also be related to diagnosing type 2 diabetes.
Checking out what can cause pale or clay colored stool could provide some helpful insights. what can cause pale or clay colored stool. Ultimately, if you’re concerned about any potential health issues, it’s always best to consult a doctor for a proper diagnosis.
Role of Medication in Managing the Condition
Medication plays a crucial role in managing type 2 diabetes. Certain medications help regulate blood sugar levels, reduce insulin resistance, or improve the body’s response to insulin. The specific medication and dosage are determined by an individual’s specific needs and health status. Regular consultations with healthcare professionals are essential for adjusting medication regimens as needed.
Healthy Meal Plans for Individuals with Diabetes
A healthy meal plan for individuals with diabetes focuses on portion control, balanced macronutrients, and mindful food choices. Prioritizing complex carbohydrates, lean proteins, and healthy fats ensures a steady release of energy and stable blood sugar levels. Examples include incorporating lean meats, poultry, fish, beans, lentils, and a variety of non-starchy vegetables. Portion sizes should be adjusted based on individual needs and activity levels.
Comprehensive Overview of Regular Exercise Routines
Regular exercise routines are essential for individuals with type 2 diabetes. Physical activity improves insulin sensitivity, helps manage weight, and reduces the risk of cardiovascular complications. A combination of aerobic exercises, such as brisk walking, swimming, or cycling, and strength training exercises, such as weightlifting or bodyweight exercises, is recommended. Consistency and gradual progression are key to achieving optimal results.
Steps for Managing Diabetes, Signs of diabetes diagnosing type 2 diabetes
Effective diabetes management involves a multi-faceted approach. Here’s a comprehensive overview of steps to follow:
- Regular Check-ups: Consistent monitoring with healthcare professionals is essential for assessing blood sugar levels, adjusting medication, and addressing any complications.
- Healthy Diet: Prioritize whole grains, lean proteins, fruits, vegetables, and healthy fats while controlling portion sizes.
- Regular Exercise: Incorporate a mix of aerobic and strength training exercises into a regular routine.
- Medication Adherence: Follow prescribed medication regimens diligently and consult healthcare professionals for any adjustments.
- Stress Management: Employ stress-reducing techniques to minimize its impact on blood sugar control.
- Monitoring Blood Sugar: Regularly monitor blood sugar levels to identify patterns and trends.
- Healthy Sleep Habits: Prioritize sufficient sleep for optimal blood sugar control and overall health.
Tools and Resources: Signs Of Diabetes Diagnosing Type 2 Diabetes
Navigating the world of type 2 diabetes can feel overwhelming. Fortunately, a wealth of resources is available to help individuals understand, manage, and live fulfilling lives with this condition. This section will explore essential tools and support systems for effective diabetes management.
Reliable Resources for Information
A comprehensive understanding of type 2 diabetes relies on accurate and up-to-date information. Numerous credible sources provide valuable insights. The American Diabetes Association (ADA) is a leading authority, offering extensive educational materials, research updates, and advocacy efforts. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health, provides scientific information and research findings.
Other reputable organizations include the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Organizations Offering Support and Education
Numerous organizations dedicated to diabetes care provide vital support and educational programs. These organizations offer a range of services, including workshops, support groups, and online forums. Local chapters of the American Diabetes Association often host workshops and seminars on topics such as healthy eating, exercise, and medication management. Diabetes support groups provide invaluable peer-to-peer interaction and shared experiences.
Many hospitals and clinics also offer specialized diabetes education programs for individuals and their families.
Technology in Diabetes Management
Technology has revolutionized diabetes management, offering tools to track, monitor, and manage blood sugar levels more effectively. Continuous glucose monitors (CGMs) allow for real-time glucose readings, enabling proactive adjustments to medication or lifestyle choices. Smart insulin pumps can automate insulin delivery based on glucose readings, providing greater convenience and potentially reducing the risk of hyperglycemia or hypoglycemia. Mobile applications provide a platform for tracking blood sugar levels, medication schedules, and other important data, fostering greater awareness and control.
Online Tools for Blood Sugar Tracking
Numerous online tools and applications provide convenient and efficient methods for monitoring blood sugar levels. These tools can be instrumental in identifying patterns, trends, and potential issues. Many applications offer features for recording blood sugar readings, calculating carbohydrate intake, and managing medications. They often provide personalized insights and recommendations to improve glucose control. For instance, some apps can connect with continuous glucose monitors (CGMs) to automatically input data.
Support Groups in Managing Diabetes
Support groups offer invaluable assistance in coping with the challenges of type 2 diabetes. These groups provide a platform for sharing experiences, offering encouragement, and learning from others facing similar situations. Sharing personal stories and practical advice can be incredibly helpful. Members can discuss coping strategies, learn from each other’s experiences with different medications, and share insights on managing stress and maintaining a positive outlook.
Last Point
In conclusion, navigating the complexities of signs of diabetes diagnosing type 2 diabetes requires a comprehensive understanding of its multifaceted nature. From recognizing early warning signs to understanding diagnostic procedures, risk factors, and potential complications, this exploration provides a roadmap for proactive health management. By adopting preventative measures and actively managing the condition, individuals can significantly improve their overall well-being.
Remember, early detection and effective management are crucial for mitigating the long-term effects of type 2 diabetes.




