Rolandic epilepsy symptoms causes diagnosis and treatment is a comprehensive exploration of this neurological condition. We’ll delve into the diverse range of symptoms, from subtle facial twitches to more pronounced motor issues, and examine the possible causes, ranging from genetic predispositions to acquired brain injuries. Understanding the diagnostic process, including crucial tools like EEGs and imaging, is key, as is the discussion of various treatment options, including medication and, in some cases, surgical interventions.
We’ll also look at long-term management strategies and the impact on daily life, offering a holistic view of this condition.
This in-depth look at rolandic epilepsy aims to provide a clear understanding of the condition, equipping readers with essential information. The multifaceted nature of this epilepsy type demands a thorough examination of its various facets, from its underlying causes to the most effective treatment approaches. We’ll provide a balanced perspective, acknowledging the complexities and uncertainties involved in managing this neurological disorder.
Symptoms of Rolandic Epilepsy
Rolandic epilepsy, also known as focal epilepsy of the temporal lobe, presents a diverse range of symptoms, primarily affecting the face, arm, or leg on the opposite side of the brain’s seizure focus. Understanding these symptoms is crucial for prompt diagnosis and effective treatment. Recognizing the pattern and severity of symptoms can help differentiate Rolandic epilepsy from other seizure types and guide appropriate medical interventions.
Symptom Manifestations by Body Part
Symptoms of Rolandic epilepsy frequently begin in the face and then spread to the arm and leg. This characteristic progression is often seen as the seizure develops. The initial symptoms are frequently subtle and can be easily overlooked, especially in children. It is important to note that the symptoms are not always consistent and can vary in severity and presentation.
- Face: Symptoms can include twitching or jerking movements of the face, tingling sensations, or numbness. These sensations may progress to more pronounced facial contortions and grimaces. A person may experience difficulty with speech or have an altered sense of taste or smell. Examples include a sudden and brief contraction of the eyelid or lip on one side of the face, or a more complex series of facial contortions, lasting seconds or minutes.
- Arm: Symptoms in the arm may manifest as involuntary movements like jerking, stiffness, or clumsiness. Individuals may experience a loss of coordination or weakness in the arm, making it difficult to perform tasks. Symptoms can range from a slight tremor to a more pronounced shaking or flailing of the arm.
- Leg: Similar to the arm, symptoms in the leg can involve involuntary movements, weakness, or loss of coordination. This may lead to stumbling, tripping, or difficulty walking. Individuals might experience a sudden jerking movement in the leg or a feeling of heaviness, or numbness.
Severity and Variability of Symptoms
The severity of Rolandic epilepsy symptoms can vary significantly. Some individuals experience only mild symptoms, such as a brief twitch or a subtle tingling sensation, while others experience more intense and prolonged symptoms. The severity can fluctuate depending on the individual’s underlying health conditions, the specific location of the seizure focus in the brain, and the overall health status. Symptoms can also differ depending on the stage of the seizure.
Rolandic epilepsy, a tricky condition, often presents with various symptoms like unusual sensations, motor twitches, or even altered consciousness. Understanding its causes, like genetic predisposition or brain injuries, is crucial for diagnosis. Different treatments, from medication to surgery, are employed depending on the specific situation. This neurological condition can sometimes lead to distinct posturing, like decorticate or decerebrate posturing, which are crucial signs to note during diagnosis.
For a deeper understanding of these posturing differences, check out this helpful resource on decorticate vs decerebrate posturing. Ultimately, accurate diagnosis and tailored treatment plans remain essential for managing Rolandic epilepsy effectively.
Early stages might show subtle signs, whereas later stages can manifest more severe and generalized symptoms.
Symptom Presentation Across Individuals and Seizure Stages
Symptoms of Rolandic epilepsy are not standardized; they can vary considerably between individuals. Even within the same individual, symptoms can change over time, depending on factors such as the specific trigger or the progression of the seizure. The pattern of symptom onset and spread can differ significantly. Some individuals might exhibit a more localized reaction, while others may experience a broader range of symptoms.
For instance, one individual might experience a sudden twitch of the face, while another might experience a complete loss of motor function in the arm and leg on the opposite side.
Table of Common Symptom Presentation
| Symptom | Body Part | Frequency | Duration |
|---|---|---|---|
| Facial twitching/jerking | Face | Variable | Seconds to minutes |
| Numbness/tingling | Face, arm, leg | Variable | Seconds to minutes |
| Speech difficulties | Face | Occasional | Seconds to minutes |
| Arm weakness/incoordination | Arm | Variable | Seconds to minutes |
| Leg weakness/incoordination | Leg | Variable | Seconds to minutes |
| Stumbling/tripping | Leg | Occasional | Seconds to minutes |
| Generalized tonic-clonic movements | Multiple body parts | Less frequent | Minutes |
Causes of Rolandic Epilepsy

Rolandic epilepsy, a focal seizure disorder affecting the brain’s frontal lobe, often presents in childhood. While the exact cause isn’t always clear, a variety of factors can contribute to its development. Understanding these potential causes is crucial for diagnosis and targeted treatment strategies. This section delves into the complexities of Rolandic epilepsy’s etiology, exploring genetic predispositions, acquired conditions, and the role of brain development.Rolandic epilepsy, a focal seizure disorder, can arise from a combination of genetic vulnerabilities and acquired factors impacting brain development.
Rolandic epilepsy, characterized by its unique symptoms, has various causes. Diagnosing it often involves a combination of neurological exams and tests. Fortunately, treatment options exist, but understanding the complexities of this condition is key. While not directly related, the procedures involved in quadruple bypass heart surgery ( what is quadruple bypass heart surgery ) highlight the dedication to treating life-altering medical conditions.
Ultimately, effective management of rolandic epilepsy symptoms relies on a thorough understanding of its diverse presentations and tailored treatment plans.
The interplay of these elements influences the likelihood of developing the condition. Genetic predisposition often increases the risk, but environmental factors can also trigger the disorder. Understanding these complexities is key to developing personalized treatment plans and preventative measures.
Genetic Predispositions
Genetic factors play a significant role in the susceptibility to Rolandic epilepsy. Variations in genes influence the structure and function of neural pathways, making individuals more prone to this condition.
- Specific genetic mutations can increase the risk. Examples include mutations in genes associated with ion channel function, synaptic transmission, and neuronal development. These mutations can disrupt normal brain activity, making individuals more vulnerable to seizure activity.
- Family history of epilepsy, particularly Rolandic epilepsy, is a strong indicator of genetic predisposition. A family history often suggests a higher chance of inheriting genes associated with the condition. This can inform diagnostic strategies and management approaches for at-risk individuals.
- The presence of other neurological disorders in a family history, such as intellectual disabilities or developmental delays, might also suggest a genetic link to Rolandic epilepsy.
Acquired Conditions
Acquired conditions, such as infections, injuries, or developmental abnormalities, can also contribute to the onset of Rolandic epilepsy.
- Infections during pregnancy or early childhood, such as meningitis or encephalitis, can cause brain inflammation and damage, increasing the risk of epilepsy.
- Head injuries, including trauma from falls or accidents, can lead to scarring and dysfunction in the brain, potentially triggering Rolandic epilepsy.
- Developmental abnormalities, such as cortical dysplasia, a structural defect in the brain’s outer layer, can result in increased seizure susceptibility.
Role of Brain Development
The process of brain development plays a vital role in the etiology of Rolandic epilepsy. Impairments in this crucial developmental stage can increase the risk.
- Immature neural circuits during early childhood are more susceptible to disruptions that can lead to epilepsy.
- Abnormal migration of neurons during brain development can result in abnormal brain structure, increasing the risk of epilepsy.
- Neurodevelopmental disorders, such as autism spectrum disorder or cerebral palsy, can be associated with an increased risk of Rolandic epilepsy.
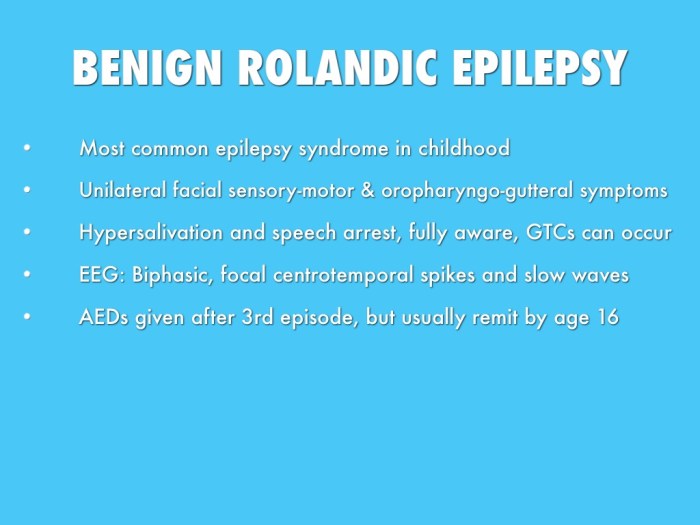
Age of Onset
The typical age range of onset for Rolandic epilepsy is generally during childhood, often between the ages of 3 and 10 years. However, cases can also occur in adolescence or even adulthood.
Prevalence of Different Causes
| Cause | Description | Prevalence |
|---|---|---|
| Genetic Predisposition | Inherited variations in genes influencing neural pathways | Estimated to be significant, but precise prevalence is difficult to quantify due to genetic complexity |
| Infections (Meningitis/Encephalitis) | Brain inflammation caused by infections | Variable prevalence depending on geographic location and incidence of infectious diseases |
| Head Trauma | Injury to the brain due to accidents or falls | Relatively common, particularly in younger age groups |
| Developmental Abnormalities (e.g., Cortical Dysplasia) | Structural defects in the brain’s outer layer | Less common but potentially severe |
Diagnosis of Rolandic Epilepsy
Unraveling the mystery of Rolandic epilepsy often hinges on a meticulous diagnostic process. Pinpointing this specific type of seizure disorder requires a combination of careful assessments, sophisticated tests, and a keen understanding of the patient’s symptoms. This process aims to differentiate Rolandic epilepsy from other neurological conditions that may present with similar symptoms.The diagnostic journey for Rolandic epilepsy typically involves a systematic approach.
Neurological examinations play a crucial role in evaluating the patient’s overall neurological function. These examinations assess motor skills, sensory responses, and cognitive abilities. The examination findings, when combined with the patient’s reported symptoms, can provide valuable clues for further investigation.
Neurological Examinations
Neurological examinations are essential in the initial stages of diagnosis. A comprehensive neurological examination assesses various aspects of the patient’s neurological function, including motor skills, sensory responses, reflexes, and coordination. Detailed observation of any focal symptoms, such as abnormal movements or sensory disturbances, can be crucial in identifying the location and nature of the seizure focus. The findings of the examination are used to guide the selection of further diagnostic tests.
Electroencephalograms (EEGs)
Electroencephalograms (EEGs) are a critical tool in diagnosing Rolandic epilepsy. EEGs measure the electrical activity in the brain, and characteristic abnormalities, such as spikes and sharp waves, are often present during seizures or between seizures. The timing and location of these abnormalities are crucial for determining the seizure origin. These patterns help to distinguish Rolandic epilepsy from other seizure types.
Imaging Techniques
Imaging techniques, like Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans, play a vital role in ruling out structural abnormalities that might mimic Rolandic epilepsy symptoms. MRI scans provide detailed images of the brain’s internal structures, allowing for the identification of lesions, tumors, or malformations. CT scans, though less detailed, can still reveal significant structural abnormalities, aiding in the differential diagnosis.
Imaging techniques are particularly important in cases where the cause of the seizures is suspected to be structural.
Diagnostic Procedures for Different Age Groups, Rolandic epilepsy symptoms causes diagnosis and treatment
The diagnostic approach varies slightly based on the patient’s age. For infants and children, the focus is on identifying any developmental delays or underlying conditions that might contribute to the seizures. The use of video-EEG monitoring might be considered for children to capture seizure activity. In adults, the diagnostic process usually involves a more detailed evaluation of the patient’s medical history and neurological status.
Ruling Out Other Neurological Conditions
Differentiating Rolandic epilepsy from other neurological conditions with similar symptoms is crucial for accurate diagnosis. Conditions like migraine, trigeminal neuralgia, and focal neurological deficits may mimic some of the symptoms of Rolandic epilepsy. Detailed neurological examinations, EEG findings, and imaging studies help to distinguish between these conditions and confirm the diagnosis of Rolandic epilepsy. A thorough evaluation of the patient’s medical history is essential to rule out potential contributing factors.
Diagnostic Steps
- Detailed medical history and physical examination, including neurological evaluation, are conducted.
- Electroencephalogram (EEG) is performed to identify characteristic electrical patterns associated with Rolandic epilepsy.
- Neuroimaging techniques, such as MRI or CT scans, are used to rule out structural abnormalities or lesions.
- Video-EEG monitoring may be employed to capture seizure activity and further characterize the EEG patterns.
- Differential diagnosis is performed to rule out other neurological conditions with similar symptoms.
Treatment Options for Rolandic Epilepsy
Rolandic epilepsy, characterized by focal seizures originating in the Rolandic cortex, necessitates a multifaceted approach to treatment. Effective management aims to reduce seizure frequency and severity, improve quality of life, and prevent potential complications. A comprehensive strategy typically combines medication, potential surgical interventions, and lifestyle adjustments.A tailored treatment plan is crucial, as individual responses to different therapies vary.
Factors like seizure type, frequency, and location within the Rolandic cortex, alongside the patient’s overall health, are considered when developing a personalized approach.
Rolandic epilepsy, characterized by its unique symptoms, has various causes, diagnoses, and treatments. Understanding these complexities is crucial for effective management. Similar to how stroke symptoms in women can present differently than in men, stroke symptoms in women often require specialized attention, this highlights the importance of individualized approaches to neurological conditions. The key to successful treatment for Rolandic epilepsy lies in early diagnosis and a tailored treatment plan, much like a personalized approach to any neurological challenge.
Anti-epileptic Drugs (AEDs)
AEDs are the cornerstone of Rolandic epilepsy treatment. They work by modulating neuronal activity, reducing the likelihood of abnormal electrical discharges that trigger seizures. Various AEDs are available, each with its own mechanism of action, efficacy, and potential side effects.
Pros and Cons of Different AEDs
The choice of AED depends on several factors, including the patient’s individual response, potential side effects, and drug interactions. Some AEDs may be more effective at controlling specific seizure types than others. For example, some AEDs are better at preventing complex partial seizures while others are more effective at controlling absence seizures. Understanding the pros and cons of different AEDs is essential for successful treatment.
Careful monitoring of the patient’s response to the drug and its potential side effects is crucial.
Surgical Interventions
Surgical interventions are considered for patients who do not adequately respond to medication or experience significant side effects. Surgical approaches vary based on the location and type of seizure focus. Surgical resection of the affected brain tissue aims to eliminate the seizure source. Partial resection involves removing only the portion of the brain generating seizures, while a more extensive procedure may involve removing a larger area of the brain if necessary.Surgical procedures carry risks, including potential neurological deficits and cognitive impairments.
The decision to pursue surgery requires careful consideration of the potential benefits and risks, and involves a thorough evaluation of the patient’s neurological status and seizure characteristics. Surgical success depends on factors like the precise location of the seizure focus, the extent of brain tissue involved, and the individual’s overall health.
Lifestyle Adjustments
Lifestyle modifications can play a supportive role in managing Rolandic epilepsy. Adequate sleep, stress management techniques, and a balanced diet can help reduce seizure triggers and improve overall well-being. Maintaining a regular sleep schedule and avoiding known triggers, such as stress or fatigue, are often important components of a comprehensive management strategy.
Multidisciplinary Approach
Managing Rolandic epilepsy requires a collaborative effort among various healthcare professionals. Neurologists, neurosurgeons, neuropsychologists, and other specialists work together to develop and implement a comprehensive treatment plan. This interdisciplinary approach ensures that patients receive the best possible care and support throughout their treatment journey. This approach helps optimize the therapeutic interventions and minimize the potential for adverse outcomes.
Support Groups
Support groups provide invaluable resources for individuals with Rolandic epilepsy and their families. These groups offer a safe space for sharing experiences, coping strategies, and emotional support. Connecting with others facing similar challenges can be empowering and help alleviate feelings of isolation. Support groups offer a valuable network for exchanging information and providing encouragement.
Common AEDs and Potential Side Effects
| AED | Potential Side Effects |
|---|---|
| Levetiracetam | Drowsiness, dizziness, fatigue, decreased appetite |
| Lamotrigine | Skin rash, nausea, dizziness, headache |
| Phenytoin | Gingival hyperplasia, skin rash, tremor, nystagmus |
| Carbamazepine | Drowsiness, dizziness, nausea, skin rash |
| Valproic acid | Weight gain, hair loss, nausea, tremor |
Management and Prognosis: Rolandic Epilepsy Symptoms Causes Diagnosis And Treatment
Living with Rolandic epilepsy requires a multifaceted approach to management. It’s not just about controlling seizures; it’s about optimizing daily life and maintaining a good quality of life. This involves a collaborative effort between the individual, their family, and medical professionals. Understanding the long-term strategies and potential impact on daily life is crucial for effective management.Managing Rolandic epilepsy involves a combination of medical interventions and lifestyle adjustments.
A personalized approach is essential, tailored to individual needs and seizure characteristics. Prognosis for individuals with Rolandic epilepsy is generally positive, especially with early diagnosis and appropriate treatment.
Long-Term Management Strategies
Effective long-term management of Rolandic epilepsy hinges on adherence to prescribed medications, regular follow-up appointments with neurologists, and meticulous monitoring of seizure frequency and severity. This proactive approach allows for early intervention if necessary, preventing the development of more complex or intractable forms of the condition. Adapting lifestyle factors to minimize seizure triggers and maximize well-being is equally important.
Impact on Daily Life and Lifestyle Adaptations
Rolandic epilepsy can significantly impact daily life, particularly if seizures are frequent or severe. Individuals may experience challenges in various aspects, including school or work performance, social interactions, and overall emotional well-being. Strategies for managing these challenges include:
- Identifying and Avoiding Triggers: Recognizing specific triggers, such as sleep deprivation, stress, or certain foods, allows individuals to proactively implement strategies to minimize their exposure. For example, maintaining a consistent sleep schedule and managing stress effectively can reduce seizure frequency.
- Maintaining a Healthy Lifestyle: Adopting a healthy diet, regular exercise, and sufficient sleep are crucial for overall well-being and seizure control. A balanced diet rich in essential nutrients can contribute to improved brain health. Regular exercise can also help manage stress and improve mood.
- Modifying Activities: Adjusting certain activities, such as strenuous exercise or exposure to specific environmental stimuli, may help reduce seizure risk. For instance, if a particular activity triggers seizures, it can be modified or avoided altogether.
Managing Stress and Anxiety
Stress and anxiety are common companions for individuals living with epilepsy. The unpredictability of seizures and the potential for social stigma can contribute to these feelings. Therefore, developing coping mechanisms for managing stress is critical.
- Stress Management Techniques: Implementing stress management techniques, such as mindfulness, meditation, deep breathing exercises, or yoga, can be very helpful in reducing anxiety levels and promoting emotional well-being. These techniques can equip individuals with tools to manage stressful situations effectively.
- Support Networks: Building a strong support network, including family, friends, and support groups, is essential for emotional well-being. Sharing experiences and connecting with others facing similar challenges can provide comfort and encouragement.
Potential for Seizure Control and Quality of Life
Seizure control is a primary goal in managing Rolandic epilepsy. With appropriate medication and lifestyle adjustments, many individuals achieve good seizure control, enabling them to lead fulfilling lives. The quality of life for individuals with Rolandic epilepsy can be significantly improved with proactive management. This includes consistent adherence to treatment plans, regular medical check-ups, and developing coping mechanisms for stress and anxiety.
Overall Prognosis
The prognosis for Rolandic epilepsy is generally favorable, especially with early diagnosis and effective treatment. Factors such as age at diagnosis, seizure frequency, and response to treatment can influence the long-term outcome. For instance, children diagnosed at a younger age and achieving good seizure control tend to have better long-term outcomes compared to adults with uncontrolled seizures. Many individuals with Rolandic epilepsy lead productive and fulfilling lives, experiencing minimal to no impact on their overall well-being.
Final Summary
In conclusion, rolandic epilepsy, while challenging, is a treatable condition. This discussion highlights the importance of early diagnosis, personalized treatment plans, and ongoing support for individuals affected by this type of epilepsy. By understanding the symptoms, causes, diagnosis, and treatment options, we can better equip ourselves to support those living with rolandic epilepsy and promote a higher quality of life.




