Prostaglandins and your pain signals: Understanding the intricate relationship between these crucial molecules and how they shape our experience of pain. This exploration delves into the fascinating world of prostaglandins, their diverse roles in the body, and their profound impact on pain perception. We’ll uncover the mechanisms behind pain signals, the involvement of inflammation, and the remarkable ways our bodies respond to injury and discomfort.
From the basics of prostaglandin structure and synthesis to the complex interplay with other pain pathways, we’ll explore the science behind this vital biological process. We’ll examine the various types of pain, including acute and chronic, and how prostaglandins contribute to each. Furthermore, we’ll investigate the existing pain management strategies, examining both pharmacological and non-pharmacological approaches, and consider the future of research in this critical area.
Introduction to Prostaglandins
Prostaglandins are a fascinating group of lipid signaling molecules, playing crucial roles in numerous physiological processes throughout the body. They act as local hormones, affecting tissues and organs near their point of production, rather than traveling through the bloodstream like traditional hormones. Their diverse actions range from regulating inflammation and pain perception to influencing blood pressure and blood clotting.
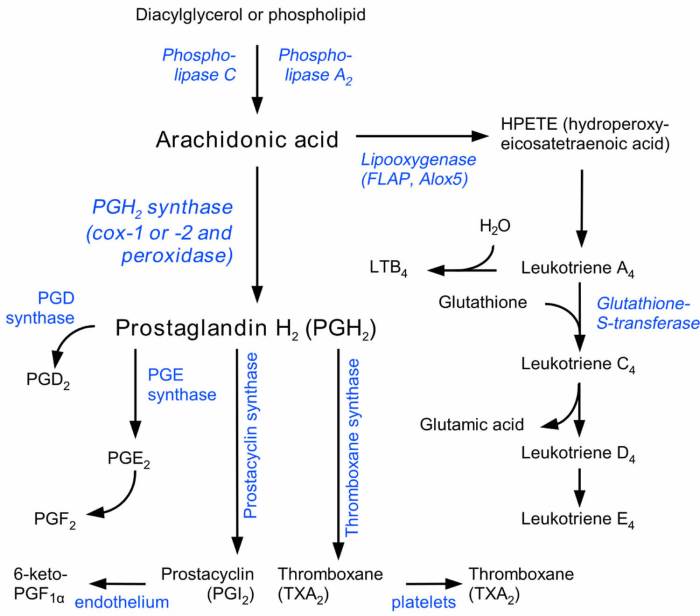
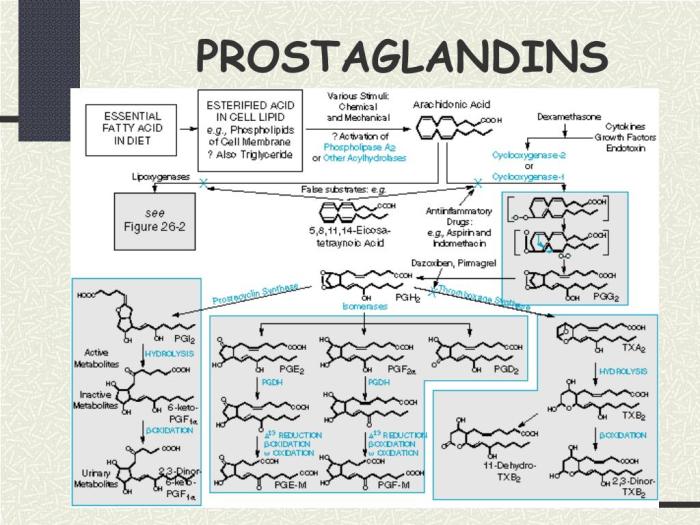
Understanding their intricate mechanisms is key to appreciating their importance in maintaining health and treating various diseases.Prostaglandins are derived from arachidonic acid, a fatty acid present in cell membranes. Their synthesis involves a complex series of enzymatic reactions, ultimately leading to the production of various prostaglandin subtypes. These subtypes have distinct structures and biological activities, highlighting the versatility of this family of molecules.
Types of Prostaglandins and Their Actions
Prostaglandins are categorized into different classes based on their chemical structures. These classes include prostaglandin E (PGE), prostaglandin F (PGF), prostaglandin D (PGD), prostaglandin I (PGI), and prostaglandin A (PGA). Each class exhibits unique biological actions, influencing various physiological processes.
- Prostaglandin E (PGE): This group is particularly well-known for its roles in inflammation, pain, and fever. Specific PGE subtypes, such as PGE 1 and PGE 2, contribute to vasodilation (widening of blood vessels), increasing vascular permeability (allowing fluid to leak from blood vessels into tissues), and inducing fever. These actions are crucial in the body’s response to injury or infection.
- Prostaglandin F (PGF): PGF 2α is often involved in uterine contractions during labor and menstruation. Its role in smooth muscle contraction is critical for these processes.
- Prostaglandin D (PGD): This class of prostaglandins is associated with various physiological responses, including smooth muscle contraction and inflammation. Specific subtypes play a role in allergic reactions and inflammatory conditions.
- Prostaglandin I (PGI): These prostaglandins primarily function as vasodilators, inhibiting platelet aggregation (clumping of platelets), and preventing blood clots. This anti-clotting property is crucial for maintaining healthy blood flow.
- Prostaglandin A (PGA): These are less abundant and have fewer well-defined functions compared to other classes. Their roles are still under active research.
Chemical Structure and Synthesis Pathways
Prostaglandins are cyclic compounds with a characteristic five-carbon ring structure. Their structure is critical for their biological activity.
The synthesis of prostaglandins starts with the release of arachidonic acid from cell membranes. This is catalyzed by enzymes like phospholipase A2. The released arachidonic acid is then metabolized by cyclooxygenase (COX) enzymes, which are responsible for producing various prostaglandin subtypes. Different COX isoforms (COX-1 and COX-2) contribute to the production of different prostaglandins.
Comparison of Prostaglandins
| Prostaglandin | Primary Effects | Biological Targets |
|---|---|---|
| PGE2 | Inflammation, pain, fever, vasodilation | Inflammation mediators, blood vessels, thermoregulatory centers |
| PGF2α | Uterine contractions, smooth muscle contraction | Uterus, smooth muscles |
| PGI2 | Vasodilation, inhibition of platelet aggregation | Blood vessels, platelets |
Prostaglandins and Pain Perception
Prostaglandins, a family of lipid compounds, play a crucial role in various physiological processes, including inflammation and pain. Their influence on pain perception is particularly significant, as they act as potent mediators in the body’s response to tissue damage and injury. Understanding their mechanisms of action is essential for developing effective pain management strategies.Prostaglandins act as chemical messengers, amplifying pain signals by interacting with specific receptors in nerve cells.
This interaction triggers a cascade of events that ultimately lead to the perception of pain. The extent of this amplification is closely tied to the level of inflammation present, further emphasizing the critical role of prostaglandins in the pain experience.
Prostaglandin-Mediated Pain Mechanisms
Prostaglandins exert their pain-inducing effects through specific receptors located on nerve cells. These receptors, primarily of the G protein-coupled receptor family, initiate intracellular signaling pathways that increase nerve excitability and sensitivity to noxious stimuli. The activation of these receptors leads to the release of other signaling molecules, further amplifying the pain response.
Receptors Involved in Prostaglandin-Mediated Pain
Prostaglandins primarily interact with specific receptors in the nervous system. These receptors, including the EP1, EP2, EP3, and EP4 subtypes of the prostaglandin E2 (PGE2) receptor family, play key roles in mediating pain signals. The activation of these receptors leads to changes in intracellular calcium levels, which influence nerve cell excitability. Different receptor subtypes exhibit varying sensitivities to different prostaglandins, contributing to the complexity of pain signaling.
Inflammation and Prostaglandin Production
Inflammation is a crucial component in the amplification of pain signals. The body’s response to tissue injury often involves the recruitment of immune cells and the release of inflammatory mediators, such as prostaglandins. These mediators not only contribute to the inflammatory response but also sensitize nerve endings, making them more responsive to painful stimuli. The interplay between inflammation and prostaglandin production is a crucial factor in determining the intensity and duration of pain.
Prostaglandins play a crucial role in transmitting pain signals throughout your body. When you’re dealing with digestive issues like constipation, certain foods can actually impact prostaglandin production. For example, some foods can exacerbate inflammation and affect the signals that lead to discomfort. Knowing which foods to avoid when you are constipated can significantly improve your overall well-being, and in turn, help manage those pesky pain signals.
So, if you’re looking for ways to ease your discomfort, check out this helpful guide on foods to avoid when you are constipated. Ultimately, understanding your body’s response to these foods will help you better manage those prostaglandin-related pain signals.
Prostaglandin Synthesis in Response to Tissue Injury
The synthesis of prostaglandins is a complex process initiated in response to tissue injury. The cascade begins with the release of arachidonic acid, a fatty acid precursor, from cell membranes. This is followed by the enzymatic conversion of arachidonic acid to various prostaglandins, a process that is primarily catalyzed by cyclooxygenase (COX) enzymes. The resulting prostaglandins then bind to their respective receptors, initiating the pain signaling cascade.
Key Enzymes in Prostaglandin Synthesis
- The production of prostaglandins relies heavily on the activity of cyclooxygenase (COX) enzymes. These enzymes catalyze the crucial step in converting arachidonic acid into prostaglandins. Two primary isoforms of COX enzymes exist: COX-1 and COX-2. COX-1 is constitutively expressed in various tissues, while COX-2 is induced in response to inflammation.
| Enzyme | Location | Function |
|---|---|---|
| COX-1 | Various tissues (e.g., stomach lining, kidneys) | Crucial for normal physiological functions. |
| COX-2 | Induced in inflamed tissues | Plays a key role in the inflammatory response, including pain amplification. |
COX-2 inhibitors, such as ibuprofen and naproxen, are commonly used to manage pain and inflammation by blocking the activity of COX-2.
Prostaglandins and Other Pain Mechanisms
Prostaglandins, as we’ve seen, play a significant role in the pain signaling cascade. However, they aren’t the sole players in this complex process. Other mechanisms contribute to the perception of pain, often interacting with and amplifying prostaglandin effects. Understanding these additional pathways is crucial for developing effective pain management strategies.Pain is a multifaceted experience, and its perception involves a complex interplay of various factors.
Different types of pain, ranging from acute to chronic, have distinct underlying mechanisms. This section delves into these additional pain pathways and how they relate to prostaglandin-mediated pain.
Comparison of Prostaglandin-Mediated Pain with Other Pathways
Prostaglandins are potent sensitizers of nociceptors, making them more responsive to stimuli. Other substances, such as bradykinin, histamine, and serotonin, also contribute to pain signaling. These substances can directly activate nociceptors or sensitize them, similar to prostaglandins. However, the specific mechanisms and targets differ, leading to variations in the intensity and duration of pain experienced. For instance, bradykinin is particularly implicated in the early inflammatory phase, while histamine contributes to the overall inflammatory response, both often working in concert with prostaglandins to enhance pain signals.
Types of Nociceptors Involved in Pain Signaling
Nociceptors are specialized sensory neurons that detect noxious stimuli. Several types of nociceptors exist, each responding to specific types of stimuli. Mechanical nociceptors detect pressure or tissue damage. Thermal nociceptors are activated by extreme temperatures. Polymodal nociceptors respond to a variety of stimuli, including mechanical, thermal, and chemical irritants.
The activation of these diverse nociceptors underlies the complexity of pain perception. Understanding which type of nociceptor is activated can help to tailor treatment strategies.
Prostaglandins play a crucial role in transmitting pain signals to your brain. They’re like tiny messengers, amplifying the sensation of discomfort. Amazingly, recent breakthroughs in immunotherapy, like the ones detailed in this article about an immunotherapy drug shrinking cancer tumors without surgery immunotherapy drug shrank cancer tumors without surgery , highlight how our bodies’ complex systems can be manipulated to fight disease.
Understanding how these processes work, like the intricate prostaglandin pathways, could pave the way for even more effective pain management strategies in the future.
Role of Other Inflammatory Mediators in Pain Perception
Inflammatory mediators, besides prostaglandins, further contribute to pain perception. These substances act in concert to amplify the pain response. Histamine, for example, increases vascular permeability, allowing other inflammatory mediators to reach the site of injury. Bradykinin, a potent vasodilator, contributes to the inflammatory response and directly stimulates nociceptors. The combined effects of these mediators contribute to the overall intensity and duration of pain, often exacerbating the pain response.
Acute and Chronic Pain and Prostaglandins
Acute pain serves as a protective mechanism, signaling tissue damage. Prostaglandins play a key role in the initiation and amplification of acute pain signals, typically lasting for a short duration. Chronic pain, however, persists for an extended period, often beyond the healing process. While prostaglandins contribute to acute pain, their role in chronic pain is more complex and often involves other mechanisms, such as nerve sensitization and altered neuronal activity.
In chronic pain conditions, prostaglandins may contribute to ongoing inflammation and sensitization, thus maintaining the pain signal.
Pain Receptors and Their Stimuli
| Pain Receptor Type | Stimulus |
|---|---|
| Mechanical Nociceptors | Pressure, stretching, pinching |
| Thermal Nociceptors | Extreme heat or cold |
| Polymodal Nociceptors | Mechanical, thermal, or chemical stimuli |
The table above summarizes the various types of pain receptors and the corresponding stimuli that activate them. This classification highlights the diverse nature of pain stimuli and the corresponding pain responses.
Prostaglandin-related Pain Management
Managing pain stemming from prostaglandin activity is a crucial aspect of modern medicine. Understanding how prostaglandins contribute to pain allows for targeted interventions. Effective pain management strategies often involve inhibiting prostaglandin synthesis or blocking their effects on pain receptors. This approach, while highly effective, necessitates careful consideration of potential side effects.
Common Pain Relievers Targeting Prostaglandins
Various over-the-counter and prescription medications effectively manage pain by interfering with prostaglandin production or action. These drugs fall into categories based on their mechanism of action.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, are frequently used for mild to moderate pain relief. They primarily inhibit the enzyme cyclooxygenase (COX), which is crucial for prostaglandin synthesis. This inhibition reduces prostaglandin production, thereby decreasing inflammation and pain.
- COX-2 inhibitors: Certain NSAIDs, like celecoxib, selectively target COX-2, the enzyme responsible for producing prostaglandins involved in inflammation. This selectivity aims to minimize gastrointestinal side effects often associated with traditional NSAIDs that inhibit both COX-1 and COX-2.
- Acetaminophen (Paracetamol): While not a true NSAID, acetaminophen works through a different mechanism to reduce pain and fever. It is thought to act on the central nervous system, inhibiting the formation of prostaglandins in the brain, thus reducing the perception of pain.
Mechanism of Action of Pain Relievers
The diverse pain relievers function through different pathways to control prostaglandin activity. This precise targeting allows for more effective pain relief with reduced side effects.
- NSAIDs: These drugs inhibit the enzyme cyclooxygenase (COX), which is vital for the production of prostaglandins. By blocking COX, NSAIDs effectively reduce the synthesis of prostaglandins responsible for pain and inflammation.
- COX-2 Inhibitors: These drugs, as their name suggests, specifically target the COX-2 enzyme. This selective inhibition minimizes the side effects often associated with NSAIDs that affect both COX-1 and COX-2. The reduced effect on COX-1, which is involved in the lining of the stomach, minimizes the risk of ulcers and other gastrointestinal issues.
- Acetaminophen: The exact mechanism of action of acetaminophen remains somewhat unclear, but it is believed to affect the central nervous system by inhibiting the formation of prostaglandins within the brain. This action reduces the perception of pain.
Efficacy and Side Effects Comparison, Prostaglandins and your pain signals
Different pain relievers exhibit varying efficacy and side effect profiles. Choosing the right medication often depends on the individual’s specific needs and health conditions.
| Drug Category | Target Receptors | Efficacy | Potential Adverse Effects |
|---|---|---|---|
| NSAIDs | COX-1 and COX-2 | Generally effective for mild to moderate pain and inflammation | Gastrointestinal upset (e.g., ulcers, bleeding), kidney problems, cardiovascular risks |
| COX-2 Inhibitors | COX-2 | Effective for pain and inflammation, often with reduced gastrointestinal side effects compared to traditional NSAIDs | Increased risk of cardiovascular events in some individuals, headache, dizziness |
| Acetaminophen | Central nervous system | Effective for pain and fever reduction | Liver damage with high doses or chronic use, potentially interacting with other medications |
Non-Pharmacological Pain Management
Beyond pharmacological approaches, non-pharmacological methods can complement pain management strategies. These techniques can help reduce prostaglandin-related pain and improve overall well-being.
- Heat or cold therapy: Applying heat or cold packs to the affected area can reduce inflammation and pain. Heat promotes blood flow, which can help reduce muscle spasms, while cold therapy can reduce swelling and inflammation.
- Physical therapy: Exercises and stretches can improve flexibility, strength, and range of motion, reducing pain and stiffness associated with various conditions. This can also improve blood flow and circulation.
- Stress management techniques: Chronic stress can exacerbate pain. Practices like meditation, yoga, and deep breathing can help manage stress and reduce pain perception.
Prostaglandins in Specific Pain Conditions
Prostaglandins, those potent lipid mediators, play a crucial role in a wide array of physiological processes, including inflammation and pain. Their influence extends beyond the general inflammatory response, significantly contributing to pain experienced in various specific conditions. Understanding the interplay between prostaglandins and these conditions is essential for developing effective pain management strategies.The levels of prostaglandins often fluctuate in specific pain conditions.
These fluctuations are tightly linked to the body’s inflammatory response and the underlying mechanisms driving the pain. The precise nature of these alterations varies depending on the condition, impacting pain intensity and duration.
Prostaglandins and Arthritis
Arthritis, characterized by joint inflammation and pain, frequently involves elevated prostaglandin production. Cytokines released during the inflammatory process stimulate the production of prostaglandins, particularly PGE2. This heightened prostaglandin presence contributes to the pain, swelling, and stiffness associated with arthritis. In rheumatoid arthritis, for example, the immune system’s attack on joint tissues triggers an inflammatory cascade, increasing prostaglandin production.
Prostaglandins and Menstrual Cramps
Menstrual cramps, a common experience for many women, are often associated with increased prostaglandin levels, particularly PGF2α. These prostaglandins cause uterine contractions, and elevated levels can intensify these contractions, leading to the characteristic pain. This heightened contractility, driven by prostaglandins, can trigger pain signals, contributing to the severity of menstrual cramps.
Prostaglandins and Inflammatory Bowel Disease
Inflammatory bowel disease (IBD), encompassing conditions like Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation in the digestive tract. The inflammation triggers an increase in prostaglandin production, especially PGE2, which contributes to the pain, diarrhea, and abdominal cramping often experienced. The elevated prostaglandin levels fuel the inflammatory response in the intestinal lining, intensifying the pain and discomfort.
Clinical Relevance of Prostaglandin Activity
The clinical relevance of prostaglandin activity in these diseases lies in their direct contribution to pain and inflammation. Understanding these mechanisms allows for the development of targeted therapies. For example, inhibiting prostaglandin synthesis can effectively reduce pain and inflammation, improving the quality of life for patients with these conditions.
Prostaglandin Inhibitors in Pain Management
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage pain associated with these conditions. These drugs, such as ibuprofen and naproxen, effectively inhibit prostaglandin synthesis. By reducing prostaglandin levels, NSAIDs help alleviate pain and inflammation. Other strategies include COX-2 inhibitors, which selectively target the enzyme responsible for prostaglandin production, reducing the risk of gastrointestinal side effects sometimes associated with broader NSAID use.
Table: Pain Conditions and Prostaglandin Involvement
| Pain Condition | Prostaglandin Primarily Involved | Mechanism of Prostaglandin Involvement |
|---|---|---|
| Arthritis | PGE2 | Increased inflammatory response, stimulating pain and inflammation |
| Menstrual Cramps | PGF2α | Increased uterine contractions, leading to pain |
| Inflammatory Bowel Disease | PGE2 | Sustained inflammation in the digestive tract, causing pain and discomfort |
Future Directions and Research: Prostaglandins And Your Pain Signals
Prostaglandins, crucial mediators in pain signaling, continue to be a focus of intense research. Understanding their intricate roles in various pain pathways is paramount to developing novel and effective pain management strategies. This exploration delves into current trends, the significance of ongoing studies, and potential future directions in targeting prostaglandin activity for pain relief.Ongoing research endeavors are not only crucial for comprehending the complexity of prostaglandin-mediated pain but also for identifying novel therapeutic targets.
The potential for developing highly specific and targeted therapies to modulate prostaglandin activity holds promise for a future with more effective and less-side-effect-prone pain management options.
Current Research Trends
Current research trends in prostaglandins and pain focus on identifying specific prostaglandin subtypes and their precise roles in different pain conditions. Researchers are meticulously examining the intricate interactions between prostaglandins and other signaling molecules in the pain pathway, including neurotransmitters and cytokines. This detailed analysis aims to pinpoint specific molecular mechanisms involved in pain sensitization and transmission. This includes studying the influence of genetic variations on prostaglandin production and activity, potentially revealing personalized approaches to pain management.
Importance of Ongoing Studies
Ongoing studies on prostaglandins and pain are vital for advancing our understanding of pain mechanisms. This knowledge is essential for refining existing pain management strategies and for developing innovative therapies. The insights gained from these studies have the potential to significantly impact patient outcomes, leading to better pain relief and improved quality of life for individuals suffering from chronic pain conditions.
Understanding the role of specific prostaglandin subtypes in different pain conditions can lead to targeted therapies with fewer side effects.
Potential Future Research Directions
Future research should explore novel approaches to modulating prostaglandin activity without significantly impacting other physiological functions. One avenue involves developing highly specific inhibitors that selectively target particular prostaglandin subtypes involved in pain transmission. Another direction includes investigating the potential of non-pharmacological interventions, such as specific lifestyle changes or therapies, to influence prostaglandin production or activity. Investigating the interplay between prostaglandins and the nervous system, including studying the role of neuronal prostaglandins, is crucial for developing more comprehensive and effective pain management strategies.
Developing Novel Prostaglandin-Targeting Therapies
The potential for developing novel prostaglandin-targeting therapies rests on our ability to identify specific prostaglandin subtypes and their receptors involved in pain signaling. This requires further research into the complex interactions between prostaglandins and other pain mediators. Targeted therapies could potentially minimize side effects associated with broad-spectrum inhibitors, leading to safer and more effective pain management. Examples include the development of monoclonal antibodies targeting specific prostaglandin receptors, or the creation of enzyme inhibitors that selectively reduce prostaglandin synthesis in pain pathways.
Gaps in Knowledge and Potential Research Avenues
| Current Gaps in Knowledge | Potential Research Avenues |
|---|---|
| Precise role of specific prostaglandin subtypes in various pain conditions | Investigating the specific contributions of different prostaglandin subtypes to distinct pain conditions, including inflammatory, neuropathic, and visceral pain. |
| Identification of novel prostaglandin receptors and their signaling pathways | Screening for novel prostaglandin receptors and investigating their signaling mechanisms in pain pathways, including their interactions with other mediators. |
| Development of targeted therapies that selectively modulate prostaglandin activity | Designing and testing new drugs that specifically inhibit the activity of key prostaglandin enzymes or receptors involved in pain transmission. |
| Exploration of non-pharmacological approaches to influence prostaglandin production or activity | Investigating lifestyle factors, therapies, and dietary interventions that may impact prostaglandin production or signaling in pain pathways. |
Visual Representations
Understanding the complex interplay between prostaglandins and pain requires visual aids. These representations can clarify the intricate pathways and mechanisms involved, making the concepts more accessible and easier to grasp. Visualizations help bridge the gap between abstract scientific principles and their real-world implications, fostering a deeper understanding of how prostaglandins contribute to pain.
Prostaglandin-Pain Receptor Interaction
This flowchart depicts the interaction between prostaglandins and pain receptors. Prostaglandins bind to specific receptors on nociceptors (pain-sensitive nerve endings). This binding triggers a cascade of intracellular events, leading to the opening of ion channels, and ultimately, the generation of an action potential that transmits the pain signal to the brain. The strength of the pain signal is influenced by the concentration of prostaglandins and the specific receptor subtype involved.
+-----------------+ +-----------------+ +-----------------+
| Prostaglandin |--->| Pain Receptor |--->| Action Potential |
| (e.g., PGE2) | | (e.g., EP2) | | |
+-----------------+ +-----------------+ +-----------------+
| |
V V
Intracellular Signaling Cascade Pain Signal Transmission
Prostaglandin Types and Locations
Different prostaglandin types (e.g., PGE2, PGF2α, PGI2) are produced in various tissues throughout the body.
This graphic would illustrate these prostaglandins with color-coded labels, indicating their primary production sites (e.g., inflamed joints, stomach lining, blood vessels). The graphic would show the widespread distribution of prostaglandin production, highlighting their crucial role in multiple physiological processes.
Prostaglandin Synthesis Pathways
This diagram will showcase the key steps in prostaglandin synthesis. It will start with the initial substrate (arachidonic acid), and will clearly illustrate the roles of key enzymes, including cyclooxygenase (COX-1 and COX-2) and lipoxygenase (LOX). The diagram will visually represent the different pathways that lead to the production of various prostaglandin types. This will aid in understanding the various pathways that can be targeted for pain management.
Arachidonic Acid ---> (COX-1/COX-2) ---> Prostaglandins (e.g., PGE2, PGF2α)
Mechanisms of Action of Pain Relievers
This infographic would visually depict the mechanisms of action of common pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, and COX-2 inhibitors. The infographic would highlight how these drugs inhibit prostaglandin synthesis, specifically targeting COX enzymes. It would illustrate the effect on the overall pain signaling pathway, demonstrating how these drugs reduce pain and inflammation.
It should also include a brief explanation of the potential side effects of these drugs.
Materials for Visual Representations
| Visual Representation | Materials Required |
|---|---|
| Flowchart/Diagram of Prostaglandin-Pain Receptor Interaction | Software for creating diagrams (e.g., Lucidchart, Visio), markers, paper or digital canvas |
| Graphic of Prostaglandin Types and Locations | Software for creating diagrams, color markers, images of body parts (if applicable) |
| Schematic Diagram of Prostaglandin Synthesis Pathways | Software for creating diagrams, icons for enzymes, arrows to represent steps |
| Infographic of Pain Reliever Mechanisms | Software for creating infographics, icons for drugs, diagram elements for pain pathways |
Final Wrap-Up
In conclusion, prostaglandins are key players in our pain signaling pathways, influencing everything from inflammation to the types of pain we experience. Understanding their roles is crucial for developing more effective pain management strategies. We’ve covered the science behind prostaglandins and their involvement in pain, along with common pain relievers and future research directions. This exploration offers a comprehensive understanding of a complex biological system and its potential implications for healthcare.




