Physical therapy after a Jones fracture is crucial for a successful recovery. This comprehensive guide dives into the essential aspects of rehabilitation, from initial exercises to advanced functional training. We’ll explore the different phases of recovery, pain management strategies, and the use of assistive devices, ultimately empowering you with the knowledge needed to navigate this challenging but ultimately rewarding process.
Understanding the unique needs of your body after a Jones fracture is key to a swift and safe recovery. This detailed guide provides a roadmap, outlining the specific exercises, timelines, and considerations crucial for successful healing and a return to optimal function.
Introduction to Jones Fracture
A Jones fracture is a specific type of break in the fifth metatarsal bone of the foot, located near the base of the bone where it joins the midfoot. This injury, while often seemingly minor, can lead to significant pain and prolonged healing if not treated correctly. Understanding the causes, symptoms, and stages of healing is crucial for effective management and recovery.
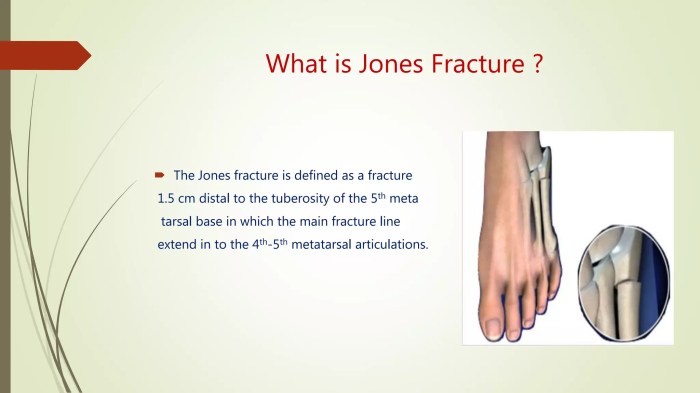
Definition of a Jones Fracture
A Jones fracture is a fracture of the base of the fifth metatarsal bone in the foot. This specific location makes it prone to delayed healing due to the unique blood supply to the region. This unique anatomy often results in the need for more extensive treatment than other types of fractures.
Typical Location and Anatomy
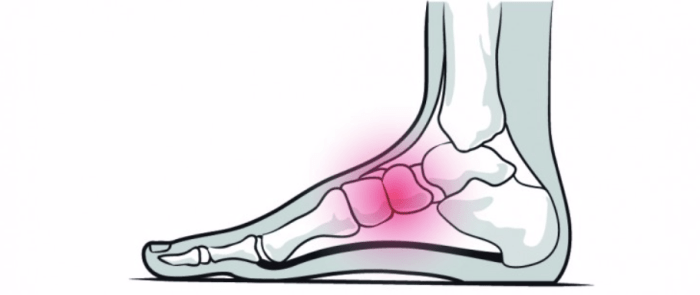
The Jones fracture occurs at the base of the fifth metatarsal bone, where it connects to the midfoot. This region is a crucial junction for the transmission of forces during weight-bearing activities. The unique anatomy of this area, characterized by a narrow blood supply to this specific section of the bone, can lead to delayed healing. The fifth metatarsal’s prominent position at the outer edge of the foot makes it susceptible to stress fractures.
Common Causes of a Jones Fracture
Jones fractures are frequently caused by sudden, forceful twisting or bending of the foot, often during sports activities. These activities may involve jumping, pivoting, or sudden changes in direction. High-impact sports like football, basketball, and tennis are particularly associated with this type of injury. Other causes may include falls or other traumatic incidents.
Common Symptoms Associated with a Jones Fracture
The hallmark symptom of a Jones fracture is pain and tenderness at the base of the fifth metatarsal bone. The pain is typically localized and may be aggravated by weight-bearing activities. Swelling, bruising, and discoloration around the affected area are also common. In some cases, patients may experience difficulty bearing weight on the affected foot. Immediate pain and tenderness are strong indicators of the potential for a Jones fracture.
Typical Stages of Healing for a Jones Fracture
The healing process for a Jones fracture can be divided into several stages.
- Initial Phase: During the initial phase, immediate medical attention is crucial to stabilize the fracture and minimize further damage. Pain management and immobilization are key to preventing further injury and allowing the healing process to begin.
- Inflammation Phase: This phase is characterized by inflammation and swelling around the fracture site. The body’s natural healing response is activated to repair the damaged tissue. This phase typically lasts several days to a few weeks.
- Repair Phase: During the repair phase, the body forms new bone tissue to bridge the gap of the fracture. This phase can take several weeks to months, depending on the severity of the fracture and the individual’s healing capacity. Careful monitoring and adherence to treatment protocols are essential for successful healing.
- Remodeling Phase: The remodeling phase involves the reshaping and strengthening of the newly formed bone. This process can continue for several months or even years, and it’s crucial for long-term stability and function. Proper rehabilitation and continued monitoring are essential in this phase. The goal is to ensure the bone heals strong enough to withstand the demands of normal activity.
Physical Therapy Considerations
Recovering from a Jones fracture requires a multifaceted approach, and physical therapy plays a crucial role in restoring function and preventing long-term complications. This comprehensive process guides you through the essential aspects of physical therapy, from initial goals to advanced exercises and potential pitfalls.
Importance of Physical Therapy
Physical therapy is vital for a successful Jones fracture recovery. It helps restore strength, flexibility, and range of motion in the affected foot and ankle. Early intervention promotes healing, minimizes the risk of complications, and accelerates the return to normal activities.
Goals of Physical Therapy for Jones Fracture Recovery
The primary goals of physical therapy for a Jones fracture focus on regaining full function of the foot and ankle. This includes restoring proper gait, achieving pain-free movement, and regaining strength and stability in the affected area. Secondary goals encompass preventing complications, such as stiffness, muscle atrophy, and joint instability.
Typical Timeline for Physical Therapy
The timeline for physical therapy after a Jones fracture is variable, depending on the severity of the fracture, the patient’s individual healing response, and adherence to the prescribed regimen. Generally, the initial phase focuses on pain management and controlled mobilization. The intermediate phase emphasizes strengthening and regaining range of motion. The final phase involves advanced exercises to restore functional capacity and prepare for a return to activities.
Types of Exercises Prescribed, Physical therapy after a jones fracture
Physical therapy for a Jones fracture often involves a progressive series of exercises, tailored to the patient’s specific needs and the stage of healing. The exercises aim to improve strength, flexibility, and proprioception (the body’s awareness of its position in space).
- Initial Phase (Weeks 1-4): Exercises primarily focus on pain management and gentle mobilization. Examples include ankle pumps, toe curls, and gentle range-of-motion exercises, performed with minimal weight-bearing or resistance. This phase is critical for preventing stiffness and promoting early healing.
- Intermediate Phase (Weeks 4-8): Exercises progress to incorporate more resistance and weight-bearing. Examples include progressive resistive exercises for ankle and foot muscles, balance exercises, and controlled weight-bearing activities. This phase aims to build strength and restore mobility.
- Advanced Phase (Weeks 8-12+): Exercises focus on restoring functional capacity and preparing for a return to activities. Examples include plyometrics (jumping exercises), agility drills, and sport-specific exercises. The goal is to gradually increase the demands on the injured area and ensure a safe return to normal activity levels. An example of a progressive exercise could involve increasing the weight lifted over time or increasing the intensity of a plyometric exercise.
Comparison of Exercises Across Phases
The types and intensity of exercises vary across the different phases of recovery. The exercises are gradually progressed from low-impact, non-weight-bearing to high-impact, full-weight-bearing activities, depending on the patient’s progress and pain tolerance. A key consideration is the appropriate progression of exercises to avoid exacerbating the injury.
Role of Manual Therapy Techniques
Manual therapy techniques, such as soft tissue mobilization and joint mobilization, are sometimes used to address pain, improve range of motion, and restore function. These techniques can help reduce muscle spasms, improve joint mobility, and enhance overall healing.
Sample Rehabilitation Program
This is a sample rehabilitation program for a Jones fracture and should be adapted to individual needs. It is crucial to consult with a physical therapist for personalized recommendations.
| Phase | Exercises | Frequency |
|---|---|---|
| Initial (Weeks 1-4) | Ankle pumps, toe curls, range-of-motion exercises | 2-3 times daily |
| Intermediate (Weeks 4-8) | Resistive exercises (ankle, foot), balance exercises, controlled weight-bearing | 2-3 times daily |
| Advanced (Weeks 8-12+) | Plyometrics, agility drills, sport-specific exercises | 2-3 times daily |
Common Complications
Potential complications of a Jones fracture include malunion (improper healing), nonunion (failure to heal), delayed union (slower-than-expected healing), persistent pain, and stiffness. Furthermore, complications can also include chronic ankle instability or pain.
How Physical Therapy Prevents Complications
Physical therapy helps prevent complications by addressing the underlying causes of these issues. It promotes proper healing, strengthens supporting muscles, improves range of motion, and enhances joint stability, thus minimizing the risk of complications.
Early Phase of Physical Therapy
The initial phase of physical therapy after a Jones fracture focuses on restoring the foot and ankle’s range of motion, promoting healthy blood circulation, and strengthening the surrounding muscles. This early stage is crucial for preventing complications and setting the stage for a successful recovery. It involves gentle, controlled exercises that progressively increase in intensity and complexity as healing progresses.
Range of Motion Exercises
Restoring full range of motion is essential to prevent stiffness and maintain joint mobility. Early exercises should be pain-free and gradually increase the arc of motion. These initial movements are designed to gently encourage the joint to move through its full range. This early focus helps prevent adhesions and scar tissue formation, which can restrict motion later.
- Gentle ankle circles: Slowly rotate the ankle in both clockwise and counter-clockwise directions. Start with small circles and gradually increase the size as tolerated. This exercise helps lubricate the joint and improves flexibility.
- Foot flexion and extension: Point your toes towards the floor (plantar flexion) and then lift your toes up towards your shin (dorsiflexion). These exercises are vital for regaining normal foot function. Start with small repetitions and gradually increase the range of motion.
- Toe spreads and gathers: Spread your toes apart and then bring them together. This helps maintain the integrity of the small muscles in the foot and enhances the overall flexibility.
Blood Circulation Exercises
Promoting blood circulation helps deliver essential nutrients to the healing bone and surrounding tissues. Increased blood flow also aids in reducing swelling and preventing stiffness.
- Ankle pumps: Slowly pump your foot up and down, flexing and extending your ankle. This action encourages blood flow and reduces swelling. Perform this exercise several times a day for short periods.
- Foot and ankle elevation: Elevating the injured foot above the heart helps reduce swelling and promotes venous return. This simple yet effective exercise is vital in the early stages of recovery.
- Gentle massage: With the guidance of your physical therapist, gentle massage can help stimulate blood circulation in the affected area. Always follow the therapist’s instructions.
Strengthening Exercises
Strengthening the muscles surrounding the ankle and foot is crucial for preventing further injury and supporting the healing bone. These exercises should be performed slowly and controlled to avoid straining the injured area.
- Theraband exercises: Using a resistance band, perform exercises such as ankle plantar flexion and dorsiflexion. This builds strength in the surrounding muscles, preventing weakness and improving stability.
- Toe curls: Lift and curl your toes against a towel or resistance band. This exercise targets the intrinsic foot muscles and helps regain strength and control.
- Marble pick-up exercises: Use a small bowl and marbles to practice picking up marbles with your toes. This exercise is a fun and effective way to improve the strength of the toes and intrinsic foot muscles.
Summary of Early Phase Exercises
| Exercise | Description | Sets | Reps |
|---|---|---|---|
| Ankle Circles | Rotating the ankle clockwise and counter-clockwise | 2 | 10-15 each direction |
| Foot Flexion/Extension | Pointing toes down and up | 2 | 10-15 repetitions |
| Toe Spreads/Gathers | Spread and gather toes | 2 | 10-15 repetitions |
| Ankle Pumps | Pumping the ankle up and down | 3 | 10-15 repetitions |
| Foot/Ankle Elevation | Elevating the foot above the heart | 3 | 15-20 minutes |
| Theraband Exercises | Ankle plantar/dorsiflexion with resistance | 2 | 10-15 repetitions |
| Toe Curls | Lifting and curling toes | 2 | 10-15 repetitions |
| Marble Pick-up | Picking up marbles with toes | 2 | 10-15 repetitions |
Intermediate Phase of Physical Therapy
The intermediate phase of physical therapy for a Jones fracture focuses on building strength and endurance in the injured foot and ankle, while progressively reintroducing functional movements. This phase builds upon the foundation established in the early phase, gradually increasing the intensity and complexity of exercises. This period is crucial for regaining optimal function and preventing future problems.
Exercises to Increase Strength and Endurance
The exercises in this phase aim to improve the strength and endurance of the muscles surrounding the ankle and foot. Progressive resistance is key to achieving optimal results. Exercises should be performed with controlled movements, focusing on proper form and avoiding pain.
Recovering from a Jones fracture often involves a dedicated physical therapy regimen. Strengthening exercises and careful mobility are key, but sometimes, alongside this, you might need to consider medication for pain management. To understand when prescription drugs might be helpful for heart health issues, check out this expert advice on the topic: ask an expert when should prescription drugs be used to heart disease.
Ultimately, the right physical therapy approach after a Jones fracture focuses on restoring function and strength safely, often guided by a medical professional.
- Calf Raises: This exercise targets the calf muscles, which are essential for ankle stability and propulsion during walking. Start with seated calf raises, progressing to standing calf raises with varying levels of resistance, such as using weights or resistance bands. Gradually increase the number of repetitions and sets.
- Ankle Pumps: These exercises help improve range of motion and circulation in the ankle. Begin with gentle circles and pumps, gradually increasing the intensity and range of motion. Focus on maintaining proper alignment and avoiding excessive twisting or bending.
- Toe Raises: These exercises strengthen the intrinsic muscles of the foot, which support balance and movement. Begin with simple toe raises, gradually progressing to toe curls and raises with resistance.
- Isometric Exercises: These exercises involve holding a static contraction of the muscles without movement. Examples include holding a contraction of the foot and ankle muscles for set periods. Isometric exercises are important for strengthening the muscles without putting excessive stress on the healing fracture.
Examples of Functional Exercises
Functional exercises mimic real-life activities, helping the patient regain the ability to perform daily tasks safely and efficiently.
- Heel Raises on a Stair: This exercise mimics the motion of ascending and descending stairs, building strength and endurance for functional movements. Gradually increase the height of the step to challenge the muscles more.
- Standing on One Leg: This exercise improves balance and coordination. Start with short durations and progress to longer durations as balance improves. Adding a resistance band or weight can further challenge the muscles.
- Single-Leg Stepping: This exercise mimics a common movement, enhancing balance and stability. Start with shorter steps and gradually increase the distance and height of the steps. Maintain a controlled and slow motion.
Exercises to Restore Balance and Coordination
Restoring balance and coordination is crucial for preventing falls and ensuring safe mobility.
- Balance Board Exercises: Balance boards provide an unstable surface, forcing the body to work harder to maintain balance. Begin with simple exercises like standing on the board and gradually progress to more challenging exercises like performing movements on the board.
- Heel-to-Toe Walks: This exercise helps improve proprioception and coordination, which are essential for walking. Focus on maintaining a slow, controlled pace and maintaining balance.
- Walking on Uneven Surfaces: This exercise enhances the body’s ability to adapt to various terrain. Start on slightly uneven surfaces and progressively increase the level of unevenness.
Intermediate Phase Exercise Table
| Exercise | Description | Sets | Reps |
|---|---|---|---|
| Calf Raises (Standing) | Lifting up onto the balls of the feet, then lowering back down. | 2-3 | 10-15 |
| Ankle Pumps | Gentle circles and pumps of the ankle joint. | 2-3 | 15-20 |
| Toe Raises | Lifting the toes off the ground, then lowering back down. | 2-3 | 10-15 |
| Single-Leg Balance | Standing on one leg, maintaining balance. | 2-3 | 30 seconds each leg |
| Heel-to-Toe Walks | Walking with each heel touching the toe in front. | 2 | 10 steps |
Advanced Phase of Physical Therapy
The advanced phase of physical therapy after a Jones fracture focuses on restoring full function and preparing you for returning to your pre-injury activity levels. This phase emphasizes progressive strengthening, sport-specific drills, and the development of crucial proprioceptive skills. Successfully navigating this stage is key to avoiding future issues and a complete recovery.This phase builds upon the foundational work of the previous stages, progressively increasing the intensity and complexity of exercises.
A tailored approach, considering your individual needs and the demands of your chosen activities, is essential. This involves working closely with your physical therapist to develop a personalized plan that gradually pushes your limits while prioritizing safety.
Returning to Pre-Injury Activity Levels
This phase involves gradually increasing the intensity and duration of exercises to prepare you for activities that require high levels of stress on the foot and ankle. This process begins with low-impact activities like walking and light jogging, and progressively incorporates more challenging movements. A key aspect of this phase is monitoring your body’s response to each activity level.
Pain, swelling, and fatigue should be addressed immediately and any increase in symptoms warrants a reduction in activity level or a temporary pause.
Sport-Specific Movements
For athletes, sport-specific movements are integrated into the advanced phase. These movements replicate the specific demands of your chosen sport, helping to restore your ability to perform crucial techniques with the necessary power and control. Examples could include jumping drills, cutting movements for basketball, or agility training for soccer. Your physical therapist will develop a plan tailored to your specific sport, carefully considering the biomechanical demands and risk factors associated with your chosen activity.
Improving Proprioception
Proprioception, or your body’s awareness of its position in space, is critical for balance and coordination. Exercises in this phase focus on challenging your body’s ability to sense its position without visual cues. Examples include single-leg balance exercises on unstable surfaces like foam pads or balance boards, and exercises that incorporate closed-kinetic chain movements. Improving proprioception reduces the risk of future injury and enhances your overall athletic performance.
Functional Training
Functional training in the advanced phase focuses on performing everyday activities, such as stairs, squatting, and rising from a chair, with the required level of strength and control. This ensures that you can seamlessly transition from physical therapy to your normal daily routine without any limitations. It is important to progressively increase the difficulty of functional tasks to maintain and build strength and stability for your everyday movements.
Recovering from a Jones fracture requires diligent physical therapy. It’s crucial to focus on regaining strength and mobility, but sometimes other health concerns can pop up during this process. Understanding risk factors like those associated with herpes, for example, can be vital to a complete recovery. Herpes causes risk factors can influence how your body responds to the therapy, so it’s important to discuss any concerns with your doctor.
The key to a successful physical therapy program after a Jones fracture is open communication and a thorough understanding of all contributing factors.
Progression of Exercises
The exercises in the advanced phase build upon those in the earlier phases. Exercises begin with simple, controlled movements and gradually progress to more complex and demanding activities. The progression is tailored to your individual needs and recovery. This systematic approach ensures you build strength and confidence gradually, minimizing the risk of re-injury.
Advanced Phase Exercises
| Exercise | Description | Sets | Reps |
|---|---|---|---|
| Single-Leg Calf Raises on Balance Pad | Perform calf raises on a balance pad, focusing on maintaining balance and control. | 3 | 10-15 per leg |
| Lateral Shuffle with Resistance Band | Perform lateral shuffles with a resistance band, focusing on lateral movement control and stability. | 2 | 10-12 per leg |
| Single-Leg Hop and Land | Perform single-leg hops and controlled landings, focusing on proper form and impact absorption. | 2 | 8-10 per leg |
| Stair Climbing with Controlled Descent | Gradually increase stair climbing with a controlled descent, focusing on maintaining balance and stability. | 2 | 10-15 repetitions |
| Sport-Specific Drills (e.g., Jumping Jacks) | Perform sport-specific drills, tailored to the individual’s needs and sport. | 2 | 10-15 repetitions |
Pain Management and Symptom Reduction: Physical Therapy After A Jones Fracture
Managing pain and symptoms is crucial for a successful recovery from a Jones fracture. Effective pain management strategies allow for increased participation in physical therapy exercises, promoting healing and restoring function. A multifaceted approach, encompassing various modalities and exercises, is essential for optimal outcomes.
Common Pain Management Strategies
Pain management during physical therapy for a Jones fracture often involves a combination of strategies. These include medication, manual therapy techniques, and the use of various modalities to reduce pain and inflammation. A patient-centered approach, tailoring interventions to individual needs, is essential for achieving optimal results.
Role of Modalities in Pain Management
Modalities play a significant role in managing pain and inflammation associated with a Jones fracture. Ice packs, for example, can effectively reduce inflammation in the acute phase, while heat can improve blood flow and reduce muscle spasms in the later stages of recovery. Careful consideration of the phase of healing is critical when choosing modalities.
Therapeutic Ultrasound
Therapeutic ultrasound uses high-frequency sound waves to promote healing. It can help reduce pain, inflammation, and swelling by increasing blood flow to the injured area. This can enhance tissue repair and facilitate a faster recovery process. The application of ultrasound needs to be carefully monitored by a physical therapist to avoid potential adverse effects.
Comparison of Pain Relief Techniques
Different pain relief techniques have varying degrees of effectiveness and are suited to different stages of recovery. For example, ice is often preferred in the acute phase to reduce inflammation, while heat might be more beneficial later to improve blood flow and reduce muscle spasms. A physical therapist will determine the most appropriate approach based on the patient’s individual needs and the specific phase of healing.
Exercises to Manage Swelling
Controlling swelling is essential to facilitate healing and reduce pain. Exercises that promote lymphatic drainage, such as gentle leg elevation and specific ankle pumps, can help minimize swelling. These exercises are typically introduced gradually as tolerated and can be incorporated into the overall physical therapy program. Examples include gentle ankle circles and foot flexion/extension exercises.
Sample Pain Management Plan
Phase Modality Exercises Medications Other Considerations Acute (First 2-4 weeks) Ice packs (20 minutes on, 20 minutes off) Gentle ankle pumps, elevation Over-the-counter pain relievers (as needed) Avoid activities that aggravate pain. Subacute (4-8 weeks) Heat packs (15-20 minutes) Range-of-motion exercises, light strengthening As needed, potentially stronger pain relievers if needed Gradual increase in activity. Advanced (8+ weeks) Transcutaneous Electrical Nerve Stimulation (TENS) Functional exercises, proprioceptive training As needed, potentially stronger pain relievers if needed Focus on returning to pre-injury activities.
Note: This is a sample plan and should be tailored to the individual patient’s needs and progress by a qualified physical therapist.
Equipment and Aids
Navigating the recovery journey after a Jones fracture often involves the strategic use of assistive devices. These tools are not merely conveniences; they are crucial for managing pain, promoting healing, and preventing further injury. Understanding their proper application and the importance of careful selection is vital for a successful recovery.Proper use of assistive devices is essential to avoid complications and ensure a smooth transition back to normal activities.
The right equipment can significantly impact the healing process and minimize discomfort. Choosing appropriate footwear, for example, can prevent re-injury and promote comfort.
Assistive Devices in Rehabilitation
Assistive devices play a vital role in supporting the injured foot and ankle during the recovery process. These devices provide stability, reduce weight-bearing, and minimize strain on the healing bone, allowing for controlled movement and healing. Examples include crutches, braces, and supportive footwear. The specific device and its usage will be determined by the individual’s specific needs and the phase of their recovery.
Crutches and Other Mobility Aids
Crutches, walkers, or other mobility aids are often prescribed to reduce weight-bearing on the injured foot. These devices help prevent further stress on the fracture site while allowing the patient to maintain mobility and perform necessary daily tasks. The duration of crutch use will vary depending on the severity of the fracture and the individual’s progress. Early and correct use of these devices is crucial to avoid exacerbating the injury and potentially slowing down the recovery process.
For example, using crutches improperly can lead to strain on other joints and muscles.
Essential Items for Recovery
A well-stocked recovery kit can greatly ease the transition back to normal life. Essential items can vary depending on individual needs and the specific recovery process, but some examples include:
- Comfortable and supportive footwear (as discussed in a later section).
- Soft, supportive pillows for elevating the injured foot.
- Over-the-counter pain relievers (consult your doctor first).
- Ice packs or cold compresses for managing swelling and pain.
- A comfortable and supportive sling or wrap (as advised by your therapist).
These items are designed to aid in pain management, comfort, and overall well-being.
Proper Footwear Selection
Choosing the right footwear is paramount to the success of a Jones fracture recovery. The goal is to support the foot and ankle, minimizing stress on the healing bone while providing comfort and stability.
Recovering from a Jones fracture takes dedicated physical therapy. It’s crucial to follow a personalized plan, focusing on strengthening the foot and ankle. While focusing on physical therapy, it’s also important to consider potential breathing treatments, like those comparing Flovent, Qvar, Pulmicort, Alvesco, or Asmanex flovent qvar pulmicort alvesco or asmanex , which can be beneficial during the recovery process.
Ultimately, consistent physical therapy is key to a full recovery from a Jones fracture.
- Avoid high heels and shoes with pointed toes, as these can put undue stress on the foot.
- Opt for shoes with good arch support and a firm heel counter to maintain proper alignment.
- Consider athletic shoes, supportive sandals, or other footwear designed for comfort and support.
- Choose shoes that fit well and do not cause pressure points or rubbing.
- If your therapist recommends it, consider specialized orthotics for added support and stability.
Following these guidelines can prevent re-injury and ensure the foot heals properly. For example, a poorly fitted shoe can cause pressure sores, leading to further complications.
Return to Activity and Sport
Returning to sports or normal activity after a Jones fracture requires a careful and gradual approach. A multi-faceted strategy involving functional tests, exercise progressions, and a cautious return to activity is crucial to prevent re-injury and ensure a full recovery. This phased approach allows the body to adapt progressively to the stresses of activity, minimizing the risk of setbacks.The goal is to restore full strength, range of motion, and proprioception (body awareness) before resuming demanding activities.
This ensures that the fractured area has healed adequately and that the surrounding tissues are strong enough to withstand the forces involved in sports or daily activities.
Criteria for Return to Activity
The criteria for returning to sports or normal activity are multifaceted and involve more than just the absence of pain. A thorough assessment by the physical therapist considers factors such as bone healing, muscle strength, joint stability, and pain tolerance. Compliance with the prescribed exercises and adherence to the rehabilitation protocol are also crucial factors. The specific criteria will vary depending on the individual’s unique circumstances, the severity of the fracture, and the nature of the activity.
Role of Functional Tests
Functional tests are essential in evaluating readiness for returning to activity. These tests assess the patient’s ability to perform tasks that mimic the demands of their sport or daily activities. These tests gauge the functional capacity of the ankle and foot. For instance, single-leg hop tests, balance exercises on a wobble board, and agility drills assess the patient’s ability to absorb and manage forces during various activities.
A positive outcome from these tests suggests the patient can safely return to the activity.
Examples of Exercises to Assess Readiness
Several exercises can assess the patient’s readiness for a return to activity. Examples include:
- Single-leg balance exercises: These exercises assess the stability and proprioception of the ankle and foot. Variations like balancing on a foam pad or with eyes closed can progressively increase difficulty.
- Hop and jump tests: These exercises evaluate the ability of the foot and ankle to absorb impact forces. The distance and number of repetitions are progressively increased to ensure the patient can handle the impact load.
- Agility drills: These assess the patient’s ability to change direction quickly and safely. Different patterns and speeds are incorporated to evaluate the patient’s response to different movements.
- Sport-specific drills: These mimic the movements and demands of the patient’s specific sport. For instance, if the patient is a basketball player, drills involving cutting, jumping, and landing would be used.
Importance of Gradual Progression
Gradual progression is paramount in the return to activity. Rushing the process can lead to re-injury, hindering the recovery process. Starting with low-impact activities and gradually increasing the intensity and duration is key. This approach allows the body to adapt to the new demands and prevent any strain or stress that could lead to setbacks.
Common Mistakes to Avoid
Common mistakes to avoid during the return to activity include:
- Ignoring pain: Persistent pain should never be ignored. Continuing activity when pain persists can exacerbate the injury and delay recovery.
- Skipping exercises: Adhering to the prescribed exercises is essential for regaining strength and stability. Skipping sessions can hinder the progress and increase the risk of injury.
- Returning to activity too quickly: The healing process takes time, and returning to high-impact activities too early can result in re-injury.
- Not listening to the body: The body provides cues about its readiness. Ignoring these signals can lead to setbacks.
Long-Term Recommendations for Preventing Future Issues
Long-term recommendations for preventing future issues include:
- Proper warm-up and cool-down routines: These routines prepare the body for activity and help prevent injury. Including dynamic stretches before activity and static stretches after activity is recommended.
- Strength training: Maintaining strong muscles surrounding the ankle and foot is crucial in preventing re-injury. Specific exercises can be tailored to the patient’s sport and activity level.
- Proper footwear: Wearing appropriate footwear that provides adequate support and cushioning is essential to prevent future injuries. Consulting with a podiatrist or sports medicine specialist can help select the right footwear.
- Regular physical activity: Maintaining a healthy lifestyle through regular physical activity is crucial for overall well-being and can aid in preventing future injuries.
Closure
In conclusion, physical therapy after a Jones fracture is a multifaceted journey. From gentle range-of-motion exercises in the early stages to advanced functional training for a full return to activity, this process demands patience and dedication. By understanding the different phases, incorporating effective pain management, and utilizing assistive devices as needed, you can significantly improve your chances of a complete recovery and prevent future complications.
Remember, consistency and proper guidance are key throughout the entire rehabilitation process.




