Patch testing for contact dermatitis is a crucial diagnostic tool for identifying the specific substances causing skin reactions. This detailed guide explores the entire process, from initial preparation to interpreting results and ultimately managing the condition. We’ll delve into the science behind the testing, covering various types of patch tests, patient preparation, reading results, and treatment options.
Understanding the intricacies of patch testing is essential for both patients and healthcare professionals. This comprehensive overview will walk you through the entire process, equipping you with the knowledge to navigate this important diagnostic procedure.
Introduction to Patch Testing
Patch testing is a crucial diagnostic tool used to identify contact dermatitis, a skin condition triggered by allergic reactions to various substances. It involves exposing small areas of skin to potential allergens to determine if a reaction occurs. Understanding the process, the types of tests, and the common allergens involved is essential for both healthcare professionals and individuals concerned about skin sensitivities.Patch testing provides a definitive way to pinpoint the specific substances causing contact dermatitis.
This precision is vital for effective treatment, as avoiding the identified allergens can significantly improve symptoms and prevent future flare-ups. The results of patch testing guide treatment strategies, allowing for personalized management plans tailored to the individual’s specific sensitivities.
Types of Patch Tests
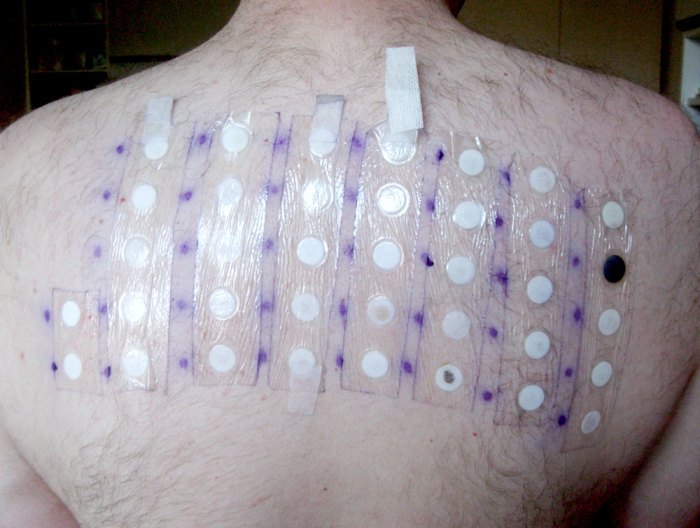
Patch testing methods are categorized by the way the allergens are applied to the skin. The most common type is the epicutaneous patch test. This involves placing small discs containing the suspected allergens on the skin, usually on the upper back, and leaving them in place for a set period, typically 48 hours to 7 days. Intradermal tests, while less common, involve injecting the allergens directly into the skin.
This method is often used to detect very potent allergens or when epicutaneous testing is inconclusive. The choice of test type depends on the specific clinical scenario and the suspected allergen.
Historical Context and Evolution
The history of patch testing reflects the advancement of dermatological diagnostics. Early methods relied on less precise exposure, often leading to inaccurate or delayed diagnoses. The evolution of patch testing has involved refining the materials used for allergen delivery, improving the standardization of the testing procedure, and broadening the range of allergens tested. This progress has led to a more accurate and efficient method for identifying the causes of contact dermatitis.
Steps in a Typical Patch Test Procedure
The process of patch testing is well-defined and involves several crucial steps. First, a detailed patient history is taken to identify potential allergens. Next, a panel of suspected allergens is selected based on the patient’s history and occupation. The selected allergens are carefully placed on the skin, usually on the back, ensuring proper technique to minimize errors.
The patient is then monitored for a set period, usually 48-72 hours and 7 days. The skin is carefully examined for any reactions.
Common Allergens Tested for in Patch Testing
The following table Artikels some of the common allergens frequently tested for in patch testing. It is important to note that this is not an exhaustive list, and the specific allergens tested will vary depending on the individual’s risk factors, occupational exposure, and medical history.
| Allergen Category | Examples |
|---|---|
| Preservatives | Parabens, Formaldehyde releasers |
| Metals | Nickel, Cobalt, Chromium |
| Topical Medications | Local anesthetics, Antimicrobials |
| Fragrances | Various fragrance mixes |
| Rubber | Latex |
| Dyes | Various dyes |
| Cosmetics | Certain fragrance oils, preservatives |
Patient Preparation and Procedure

Proper preparation is crucial for accurate patch test results. This involves minimizing potential confounding factors and ensuring the integrity of the test itself. The process, while seemingly straightforward, requires meticulous attention to detail to yield reliable diagnostic information. Avoiding certain substances and activities prior to the test can significantly impact the outcome. Following the prescribed steps for applying allergens and observing the test site are also vital for accurate interpretation.
Importance of Proper Patient Preparation
Patient preparation significantly influences the reliability of patch test results. Skin conditions, medications, and other factors can interfere with the test’s accuracy. For example, recent sun exposure or use of topical steroids can alter skin reactivity, potentially leading to false-positive or false-negative results. The goal is to standardize the testing environment and minimize external variables that could obscure the reaction to the allergens being tested.
Proper patient preparation involves a thorough history-taking session to identify any potential confounding factors and ensure the patient is informed about the procedure.
Steps Involved in Applying Patch Test Allergens
Applying the patch test allergens involves a precise and standardized technique. The allergens are typically dispensed onto small, adhesive patches that are then applied to specific areas of the skin. The allergens are placed in a pre-determined pattern to allow for proper visualization and evaluation of the reactions. The procedure also includes meticulous documentation of the placement of each patch, the date, and the allergen.
Accurate labeling of each patch is essential for later analysis.
Potential Factors Influencing Patch Test Results
Several factors can influence the outcome of a patch test, impacting the accuracy of the diagnosis. Skin conditions like eczema or psoriasis can affect the skin’s reaction to the allergens, potentially leading to exaggerated or diminished responses. Certain medications, such as topical corticosteroids, can suppress the immune response, potentially masking an allergic reaction. Furthermore, the patient’s overall health status, including any concurrent illnesses or recent infections, can also affect the test results.
Environmental factors like sun exposure and skin irritants can also impact the test’s reliability. The timing of the test in relation to other treatments is also important.
Common Locations for Patch Testing Application
Patch tests are typically applied to specific areas of the skin, with standardized locations used for consistent results. The back is a common site due to its large surface area and relative uniformity. The upper back, avoiding bony prominences, is the most frequent choice. This ensures the allergens are exposed to similar skin conditions throughout the test area.
Additional sites may be considered depending on the patient’s anatomy and specific circumstances.
Ever wondered about patch testing for contact dermatitis? It’s a crucial step for identifying skin irritants. Finding out what’s causing your skin issues is key, and sometimes, simple things like the ingredients in your skincare routine can be culprits. Have you considered using salt water for the face? salt water for the face might sound strange, but it can be a soothing and potentially helpful approach.
Regardless, patch testing remains a vital diagnostic tool in pinpointing the specific triggers, helping you craft a personalized skincare strategy to avoid future flare-ups.
Comparison of Patch Test Application Methods
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Finn Chamber Technique | Allergens are placed in small chambers, typically on the back. | Provides a controlled environment for the allergen. | May cause some discomfort. |
| Open Application Technique | Allergens are placed directly onto the skin, usually on the back. | Simpler application method. | Potential for skin irritation. |
This table illustrates the key differences between two common methods of patch test application. Each method has advantages and disadvantages that should be considered by the clinician.
Precautions and Contraindications
Certain precautions and contraindications are essential for safe and effective patch testing. Skin conditions that could interfere with the test, such as open wounds or active infections, should be considered. The presence of a history of severe reactions to patch testing is also a significant contraindication. Patients should be informed about the potential for skin irritation and instructed to avoid scratching the test site.
Patients must be advised about the possibility of allergic reactions, even minor ones, and the importance of promptly reporting any adverse effects to the healthcare provider.
Reading and Interpreting Results
Deciphering the results of patch testing is crucial for accurate diagnosis and effective management of contact dermatitis. A skilled clinician meticulously examines the reaction sites, comparing them to a standardized scale. This meticulous process helps distinguish between harmless reactions and those indicative of a specific allergic response.The interpretation process is not simply a matter of looking at the skin; it involves understanding the context of the test, the patient’s history, and the potential allergens.
A thorough analysis of the reactions and their severity is paramount to avoid misdiagnosis and ensure appropriate treatment for the patient.
Procedure for Reading Patch Test Results
Reading patch test results requires careful attention to detail. The process typically involves visual assessment of the reaction sites 48-72 hours after application. Each test site is evaluated individually, noting the presence or absence of a reaction. The skin reaction is graded based on predefined criteria, and the presence or absence of a positive reaction is documented.
It’s essential to meticulously record the findings, ensuring clarity and accuracy in the documentation. A consistent approach to the reading process is vital for reliable results.
Criteria for Classifying Patch Test Reactions
Patch test reactions are classified according to their appearance and extent. These classifications help determine the severity and nature of the allergic response. Various scales are used to quantify the reaction, ranging from negative to severe. The severity and the size of the reaction often correlate to the strength of the allergic response.
Examples of Positive and Negative Patch Test Reactions
A negative reaction typically presents as no visible change in the skin at the test site. The skin remains unaltered, indicating no allergic response to the specific allergen. A positive reaction, on the other hand, displays various forms, such as erythema (redness), edema (swelling), papules (small bumps), vesicles (small blisters), or bullae (larger blisters). The intensity and size of these reactions vary depending on the individual’s sensitivity and the concentration of the allergen.
- Negative Reaction: No visible reaction at the test site. The skin appears normal and unchanged compared to the surrounding areas. This indicates no allergic response to the specific allergen.
- Positive Reaction (Mild): Erythema (redness) and slight edema (swelling) are present at the test site. The reaction is confined to the area of the applied allergen patch.
- Positive Reaction (Moderate): More pronounced erythema and edema, potentially with papules (small bumps) or vesicles (small blisters) present at the test site. The reaction extends beyond the area of the applied patch.
- Positive Reaction (Severe): Significant erythema, edema, and vesicles or bullae (larger blisters) are present. The reaction might extend significantly beyond the patch site and potentially cause significant discomfort or pain.
Common Pitfalls and Errors in Interpreting Patch Test Results
Misinterpreting patch test results can lead to inaccurate diagnoses and inappropriate treatments. Common errors include overlooking subtle reactions, misjudging the size or severity of a reaction, or failing to consider the patient’s medical history. Proper training and experience are essential for accurate interpretation.
Significance of Delayed Reactions in Patch Testing
Delayed reactions, which manifest hours or days after the patch test application, can be equally important in diagnosis. These delayed reactions may not be immediately apparent and can be easily missed if the reading is performed too early. The significance lies in recognizing that the reaction might develop over time.
Table Comparing Different Classifications of Patch Test Reactions
| Classification | Description | Appearance | Significance |
|---|---|---|---|
| Negative | No visible reaction | Normal skin | No allergic response to the allergen |
| Weak Positive | Slight erythema and edema | Mild redness and swelling | Possible allergic response, but further evaluation might be needed. |
| Moderate Positive | Erythema, edema, and papules | Redness, swelling, small bumps | Stronger allergic response, potentially requiring further investigation. |
| Strong Positive | Erythema, edema, vesicles, or bullae | Redness, swelling, blisters | Significant allergic response, potentially requiring immediate action. |
Management and Follow-up
Patch testing is more than just identifying allergens; it’s a crucial step in effectively managing contact dermatitis. Understanding the results and implementing appropriate management strategies are vital for preventing flare-ups and improving patient quality of life. This section will delve into the practical aspects of managing a positive patch test result, including treatment options, patient education, and the crucial role of avoidance measures.Effective management of contact dermatitis hinges on a thorough understanding of the underlying cause.
Patch testing provides this knowledge, guiding clinicians and patients towards targeted interventions and preventative measures. This knowledge is critical for long-term control and prevention of future reactions.
Managing a Positive Patch Test Result
Understanding the positive test results is essential for developing an effective management plan. The severity of the reaction, the specific allergens identified, and the patient’s overall health must all be considered. This comprehensive approach ensures personalized care.
- Identifying the culprit allergen(s): The first step involves identifying the specific allergens that triggered the reaction. This precise identification is critical for effective avoidance strategies and treatment selection. A common example would be a patient experiencing hand dermatitis who tests positive for nickel. This knowledge allows for targeted measures to prevent further reactions.
- Implementing Avoidance Measures: Complete avoidance of the identified allergen(s) is paramount. This includes minimizing exposure to everyday items containing these substances, such as cosmetics, jewelry, and certain fabrics. This can be exemplified by someone who develops a rash from a specific type of soap; they can then avoid using that soap and discover an alternative that doesn’t cause a reaction.
- Initiating Topical Treatments: Topical corticosteroids, emollients, and antihistamines are commonly used to manage the inflammation and itching associated with contact dermatitis. These treatments help alleviate symptoms and promote healing. For instance, topical corticosteroids can effectively reduce inflammation, while emollients hydrate the skin, preventing dryness and further irritation.
- Systemic Medications (if needed): In cases of severe or widespread contact dermatitis, systemic medications like oral corticosteroids or antihistamines may be necessary to control inflammation and symptoms. The choice of systemic medication will depend on the severity of the reaction and the patient’s overall health.
Treatment Options for Contact Dermatitis
Numerous treatment options are available to manage contact dermatitis, depending on its severity and the specific allergens involved.
- Topical Corticosteroids: These are often the first-line treatment for mild to moderate contact dermatitis. They help reduce inflammation and itching. Different strengths and types of topical corticosteroids are available, allowing for a tailored approach to treatment.
- Emollients: These help moisturize and soothe dry, irritated skin. Emollients are crucial in preventing further skin damage and promoting healing. Examples include creams, lotions, and ointments.
- Antihistamines: These medications can help relieve itching. Oral antihistamines are often used in conjunction with topical treatments to provide comprehensive relief.
- Intralesional Corticosteroids: These are injected directly into the affected area for more localized treatment. This method can be particularly effective for localized, persistent lesions.
- Phototherapy: This treatment involves exposing the skin to ultraviolet light, often used in severe cases or those not responding to other treatments.
Patient Education and Follow-up
Patient education plays a critical role in managing contact dermatitis. Educating patients about the triggers, avoidance measures, and proper use of treatments is essential for long-term control. This education enables patients to actively participate in their care and prevent future flare-ups.
- Importance of Avoidance Measures: A key aspect of patient education involves highlighting the importance of avoiding the identified allergens. Detailed information on common sources of these allergens is crucial for successful avoidance.
- Regular Follow-up Appointments: Regular check-ups with a dermatologist or allergist are necessary to monitor the effectiveness of treatment and adjust the management plan as needed. This helps ensure that the treatment is appropriate and effective.
Role of Avoidance Measures
Avoiding contact with the identified allergens is the cornerstone of managing contact dermatitis. This proactive approach prevents further irritation and allows the skin to heal. By understanding the allergens and the products containing them, patients can minimize exposure and prevent future reactions.
- Identifying Sources of Allergens: This involves identifying everyday items, cosmetics, and environmental factors that contain the identified allergens. This is essential to avoid exposure. For instance, a patient with a nickel allergy needs to be mindful of jewelry, watches, and other metal items.
- Product Labeling and Ingredient Lists: Understanding product labeling and ingredient lists is vital for avoiding exposure to allergens. Reading ingredient lists and avoiding products with the identified allergens is crucial.
Treatment Strategies for Different Contact Dermatitis Types
Different types of contact dermatitis may respond differently to various treatments.
| Contact Dermatitis Type | Treatment Strategies |
|---|---|
| Irritant Contact Dermatitis | Focus on barrier repair with emollients, moisturizers, and occlusive dressings. Avoidance of irritants is crucial. |
| Allergic Contact Dermatitis | Complete avoidance of the identified allergen is paramount. Topical corticosteroids, antihistamines, and potentially systemic medications may be necessary. |
| Photocontact Dermatitis | Avoidance of sunlight or UV exposure, particularly during peak hours. Topical corticosteroids and emollients. Phototherapy in severe cases. |
Special Considerations and Variations
Patch testing, while a valuable diagnostic tool, requires careful consideration of various factors to ensure accurate results and appropriate patient management. Different patient populations and underlying conditions can influence the test’s interpretation. Understanding these variations is crucial for dermatologists and allergists to provide optimal care.
Patch testing for contact dermatitis is crucial for identifying irritating substances. While there’s no magic bullet for skin conditions, finding the culprit can significantly improve your quality of life. Interestingly, some researchers are exploring the potential for a similar targeted approach to a type 2 diabetes cure , focusing on pinpointing specific triggers. Ultimately, meticulous patch testing remains a cornerstone in diagnosing and managing contact dermatitis effectively.
Patch Testing in Specific Populations
Factors such as age and pregnancy status significantly impact patch testing protocols. Children, for example, might have altered skin reactions compared to adults. The thinner skin of infants and young children may lead to more pronounced reactions, while the integrity of the skin barrier might be compromised in pregnant women due to hormonal changes. Special consideration needs to be given to the potential effects of pregnancy hormones on the skin’s response to allergens.
Appropriate modifications in patch test application, reading, and interpretation are essential to avoid misdiagnosis.
Challenges in Patch Testing Patients with Skin Conditions
Patients with pre-existing skin conditions, such as eczema or psoriasis, present unique challenges in patch testing. The presence of pre-existing dermatitis can obscure the distinction between the patient’s baseline condition and a potential allergic reaction. This overlap in symptoms can complicate the interpretation of results. A thorough clinical evaluation, including detailed patient history and careful observation of the skin lesions, is essential to differentiate between the patient’s baseline condition and a potential allergic contact dermatitis reaction.
The choice of patch test materials and application techniques should be tailored to the specific skin condition to minimize discomfort and maximize diagnostic accuracy.
Patch testing for contact dermatitis is all about identifying those pesky allergens causing skin reactions. Understanding what those tiny bumps and rashes mean is crucial, but sometimes, you might need to look beyond the skin’s surface. For example, your doctor might order a urinalysis to check for underlying issues, like kidney function, which could indirectly impact the health of your skin.
To learn more about interpreting those urinalysis results, check out this helpful resource: what do your urinalysis results mean. Ultimately, though, patch testing is the key to pinpointing the specific irritants causing your skin problems.
Patch Testing in Occupational Contact Dermatitis, Patch testing for contact dermatitis
Occupational contact dermatitis (OCD) is a significant concern in the workplace. Patch testing plays a crucial role in identifying the causative agents in occupational settings. A thorough assessment of the patient’s work environment and exposure to potential allergens is vital. The results of patch testing can guide preventative measures in the workplace, such as providing appropriate personal protective equipment (PPE) and modifying work procedures.
Alternative Methods for Diagnosing Contact Dermatitis
While patch testing is a cornerstone of contact dermatitis diagnosis, alternative methods exist. These include skin prick tests, intradermal tests, and in vivo exposure tests. These methods can offer additional insights or be employed in situations where patch testing is contraindicated or less feasible. However, the sensitivity and specificity of these alternative methods might differ from patch testing.
Assessing Allergic Contact Hypersensitivity
Patch testing effectively identifies the specific allergens responsible for allergic contact hypersensitivity. The results of the patch test, when combined with clinical findings and patient history, can provide a clear understanding of the underlying cause of the skin reaction. This information is essential for formulating effective management strategies and preventive measures. The results of patch testing provide a foundation for individualized management plans, including avoidance of causative agents and use of topical treatments.
Comparison of Patch Testing Methods in Different Populations
| Population | Patch Test Considerations | Alternative Methods |
|---|---|---|
| Children | Thinner skin; potential for more pronounced reactions; use of smaller concentrations of allergens; careful monitoring | Skin prick tests may be considered, but patch testing is generally preferred for more reliable results. |
| Pregnant Women | Hormonal changes may influence skin reactivity; use of lower concentrations of allergens; careful monitoring; potential for increased skin sensitivity | Skin prick tests may be considered, but patch testing is often the preferred method for evaluating potential allergens, with caution taken for potential impact on pregnancy. |
| Patients with Pre-existing Skin Conditions | Careful distinction between baseline condition and potential allergic reaction; modification of test application; thorough clinical evaluation; avoid overlaps. | Skin prick tests may be considered, but patch testing is generally preferred for detailed evaluation of potential contact allergens. |
Illustrative Cases: Patch Testing For Contact Dermatitis
Patch testing, a crucial diagnostic tool for contact dermatitis, reveals patterns in individual responses to various allergens. Understanding these patterns, through real-world examples, provides a practical application of the knowledge gained from the earlier sections on preparation, procedure, and interpretation. These cases illustrate the diagnostic significance of patch testing and highlight the importance of careful clinical assessment in conjunction with test results.
Positive Patch Test Result Case Study
A 35-year-old woman presented with a persistent, itchy rash on her hands and forearms. The rash worsened after gardening. Patch testing revealed a positive reaction to nickel sulfate, a common allergen found in jewelry and other metal objects. The patient reported wearing nickel-containing jewelry frequently. This confirmed the suspected diagnosis of contact dermatitis.
The patient was advised to avoid nickel-containing products and was prescribed topical corticosteroids for symptomatic relief. The successful management highlights the direct correlation between exposure to an allergen and the resulting dermatitis.
Negative Patch Test Result Case Study
A 42-year-old man presented with a rash on his face, which he believed was triggered by a new skincare product. Patch testing to common contact allergens, including fragrances, preservatives, and other chemicals, was negative. The patient’s symptoms improved after discontinuing the skincare product. This case demonstrates that a negative patch test result does not automatically rule out contact dermatitis, but it can indicate that the allergen is not one of the common allergens tested.
Further investigation and a thorough patient history are critical in determining the causative agent.
Importance of Proper Interpretation Case Example
A 28-year-old woman developed a rash on her wrists after using a new hand cream. Patch testing showed a weak reaction to a fragrance mix. The patient denied using any products containing fragrance before. A careful evaluation of the patient’s history revealed that the hand cream contained a fragrance ingredient not present in previous products. This case exemplifies the importance of thorough questioning of the patient’s usage history.
This helps determine the potential causative agent of the rash.
Clinical Presentation of Contact Dermatitis
Contact dermatitis manifests differently depending on the causative agent and the individual’s sensitivity. In some cases, it presents as a localized, erythematous rash with scaling and vesicles. Other cases might involve intense burning or stinging sensations. In patients with prolonged or severe exposure, the dermatitis can evolve into chronic lesions with lichenification. The clinical presentation varies based on the type of allergen and duration of exposure, emphasizing the need for a comprehensive evaluation.
Significance of Patch Testing in Differential Diagnosis
Patch testing plays a crucial role in differentiating contact dermatitis from other skin conditions. Conditions such as eczema, psoriasis, and fungal infections can mimic the appearance of contact dermatitis. Patch testing helps narrow down the possibilities by identifying specific allergens that trigger the reaction. This information is vital for appropriate management and avoiding unnecessary treatments. It allows for a precise diagnosis and ensures that the patient receives targeted therapy.
Summary Table of Illustrative Cases
| Case # | Patient Profile | Clinical Presentation | Patch Test Result | Causative Agent (if identified) | Management |
|---|---|---|---|---|---|
| 1 | 35-year-old woman, gardener | Itchy rash on hands/forearms | Positive to nickel sulfate | Nickel | Avoid nickel, topical corticosteroids |
| 2 | 42-year-old man, new skincare | Rash on face | Negative | Not among tested allergens | Discontinued skincare product |
| 3 | 28-year-old woman, hand cream | Rash on wrists | Weak reaction to fragrance mix | Fragrance ingredient in hand cream | Avoidance, topical treatment |
Equipment and Materials
Patch testing, a crucial diagnostic tool for contact dermatitis, relies on precise equipment and materials. Proper selection, storage, and handling of these items are paramount for accurate results and patient safety. The meticulous preparation and application of allergens are critical steps in the process.
Essential Equipment for Patch Testing
The accuracy and safety of patch testing depend heavily on the proper equipment. A range of tools and materials is necessary for a successful and reliable test. These include:
- Patch Test Applicators: These are used to carefully apply the allergens to the patient’s skin. Different sizes and shapes of applicators are available to accommodate various allergen types and application needs. Applicators must be sterile and designed to prevent cross-contamination.
- Allergen Containers: Secure and leak-proof containers are needed to store the allergens. These containers must be clearly labeled with the allergen name, concentration, and lot number. The containers must also maintain the allergen’s integrity and prevent degradation or contamination.
- Patch Test Adhesive Strips: These strips are used to secure the allergen-containing patches to the skin. The adhesive should be strong enough to hold the patches in place throughout the testing period but gentle enough to avoid skin irritation.
- Allergen Preparation Equipment: Depending on the type of allergen, different equipment might be needed for preparation. This can include sterile spatulas, pipettes, or other tools for accurate and safe allergen dilution.
- Sterile Gauze and Tape: Sterile gauze and hypoallergenic tape are used for wound care and securing the patches in place. These materials help maintain a sterile environment and prevent contamination.
- Gloves and Protective Apparel: Gloves and other protective clothing are essential to prevent cross-contamination and ensure the safety of both the healthcare provider and the patient. Proper hand hygiene practices should also be followed.
- Patient Documentation Forms: Proper documentation is crucial to record the test results and the patient’s history. Forms should be designed to accurately capture all relevant information, including patient details, allergen application details, and observed reactions.
Types of Allergens Used in Patch Testing
A wide array of allergens are used in patch testing. These include:
- Cosmetics: Common allergens found in cosmetics include fragrances, preservatives, and dyes.
- Metals: Nickel, cobalt, and chromium are frequent causes of allergic contact dermatitis.
- Preservatives: Parabens, formaldehyde releasers, and imidazoles are frequently encountered preservatives in products and can induce allergic reactions.
- Dyes: Certain dyes, such as paraphenylenediamine (PPD) used in hair dye, can trigger allergic reactions.
- Plant Extracts: Poison ivy, oak, and sumac are common plant allergens that can cause severe contact dermatitis.
- Pharmaceuticals: Certain medications can cause allergic contact dermatitis, and patch testing helps identify these potential allergens.
- Rubber Chemicals: Allergens found in rubber products, such as thiurams and mercaptobenzothiazole, can lead to allergic reactions.
Storage and Handling of Patch Test Materials
Proper storage and handling of patch test materials are critical for maintaining their integrity and preventing contamination.
- Allergens should be stored at the appropriate temperature and humidity to maintain their potency and stability.
- Containers should be clearly labeled with the allergen’s name, concentration, lot number, and expiration date.
- Allergens should be prepared in a sterile environment to prevent contamination and ensure accurate results.
- Strict adherence to safety protocols is essential to prevent accidental exposure to allergens.
Preparing Patch Test Allergens
Allergen preparation is a critical step in patch testing. The following procedure ensures accurate dilutions and safe application:
- Allergens are typically diluted in a suitable vehicle, such as petrolatum, to achieve the appropriate concentration.
- Accurate dilutions are essential to avoid over or under-stimulation of the skin reaction.
- Proper mixing and handling techniques are crucial to maintain the integrity of the allergen.
- Allergens should be prepared under aseptic conditions to prevent contamination.
Patch Test Materials and Their Uses
| Material | Use |
|---|---|
| Patch Test Applicators | Apply allergens to the skin |
| Allergen Containers | Store allergens |
| Patch Test Adhesive Strips | Secure allergen patches to the skin |
| Sterile Gauze | Wound care and protection |
| Allergen Preparation Equipment | Dilute and prepare allergens |
| Gloves | Prevent cross-contamination |
| Patient Documentation Forms | Record patient information and test results |
Closure
In conclusion, patch testing for contact dermatitis is a vital diagnostic and management tool. By understanding the process, from preparation and application to reading and interpreting results, individuals can effectively identify triggers and manage this condition. This guide has provided a comprehensive overview, equipping you with the knowledge to approach this important aspect of skin care with confidence.




