Paroxysmal nocturnal hemoglobinuria symptoms encompass a range of debilitating effects stemming from a rare blood disorder. Understanding the diverse ways this condition manifests is crucial for diagnosis and effective management.
This comprehensive guide delves into the various symptoms associated with paroxysmal nocturnal hemoglobinuria, exploring their causes, impacts on different body systems, and potential severity. We’ll examine the common symptoms, including those related to hemolysis, thrombosis, and organ damage, offering a clear and detailed picture of this complex disease.
Introduction to Paroxysmal Nocturnal Hemoglobinuria (PNH)

Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, and potentially life-threatening blood disorder characterized by the destruction of red blood cells. This destruction occurs due to an underlying genetic defect that affects the production of certain proteins crucial for protecting red blood cells from the complement system. Understanding the mechanisms behind PNH is critical for diagnosis and treatment strategies.The complement system is a complex cascade of proteins in the blood that plays a vital role in the immune response, including the destruction of pathogens.
In healthy individuals, red blood cells are protected from the complement system by certain membrane proteins. However, in PNH, these protective proteins are missing or defective in a subset of red blood cells, leading to their premature destruction.Genetic defects associated with PNH are primarily mutations in the PIG-A gene. This gene encodes for an enzyme crucial for the synthesis of certain membrane proteins on red blood cells.
Mutations in PIG-A lead to the absence or malfunction of these proteins, making red blood cells vulnerable to complement-mediated lysis. These genetic abnormalities are acquired, not inherited, and the precise mechanisms of how these mutations arise remain largely unknown.
Comparison of PNH with Other Hemolytic Anemias
A crucial aspect of understanding PNH involves differentiating it from other hemolytic anemias. While all hemolytic anemias involve the premature destruction of red blood cells, the underlying causes and mechanisms vary. The following table highlights some key differences:
| Feature | PNH | Autoimmune Hemolytic Anemia (AIHA) | Hereditary Spherocytosis | Sickle Cell Anemia |
|---|---|---|---|---|
| Underlying Mechanism | Defective complement regulatory proteins on red blood cells due to PIG-A gene mutation. | Antibodies targeting red blood cells. | Defective red blood cell membrane proteins causing abnormal shape. | Abnormal hemoglobin leading to red blood cell rigidity and distortion. |
| Genetic Basis | Acquired somatic mutation in the PIG-A gene. | Variable, often related to immune system dysregulation. | Inherited mutations in genes encoding red blood cell membrane proteins. | Inherited mutations in the beta-globin gene. |
| Symptoms | Hemoglobinuria (especially at night), fatigue, anemia, abdominal pain, and potential complications like thrombosis. | Fatigue, jaundice, anemia, and potential complications like splenomegaly. | Jaundice, anemia, and potential complications like gallstones. | Pain crises, anemia, organ damage, and infections. |
| Treatment | Supportive care, blood transfusions, eculizumab (complement inhibitor), and other therapies. | Immunosuppressants, corticosteroids, and blood transfusions. | Splenectomy, folate supplementation, and blood transfusions. | Hydroxyurea, blood transfusions, and pain management. |
This table demonstrates the key differences in the underlying mechanisms, genetic basis, symptoms, and treatment approaches for various hemolytic anemias, emphasizing the unique nature of PNH. Each condition requires a tailored approach to diagnosis and management.
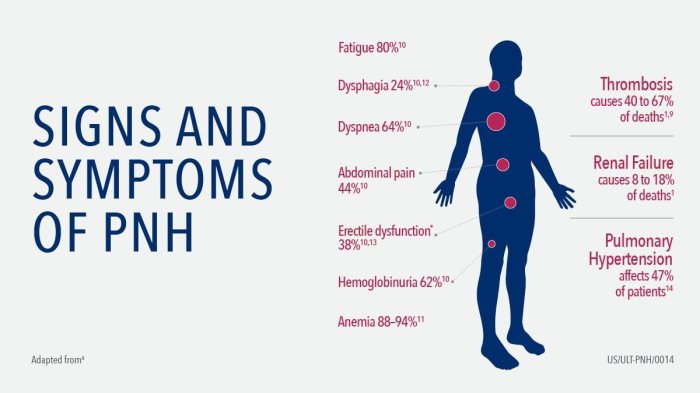
Common Symptoms of PNH
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare, chronic blood disorder characterized by the destruction of red blood cells. This destruction leads to a variety of symptoms, impacting various body systems. Understanding these symptoms is crucial for early diagnosis and effective management of the disease.
Symptoms Categorized by Body System
PNH’s diverse impact on the body is reflected in the wide range of symptoms experienced by individuals. This section categorizes symptoms based on the affected body system, providing a clearer picture of the disease’s multifaceted nature.
Paroxysmal nocturnal hemoglobinuria (PNH) symptoms can be surprisingly varied, impacting everything from fatigue to painful urination. While exploring natural remedies for various health concerns, some research suggests ashwagandha for erectile dysfunction ashwagandha for erectile dysfunction might offer potential benefits. However, it’s crucial to remember that PNH requires proper medical diagnosis and management, and should not be treated with alternative remedies alone.
| Body System | Common Symptoms | Pathophysiology |
|---|---|---|
| Blood | Hemoglobinuria (especially at night), Anemia, Fatigue, Pallor | The destruction of red blood cells releases hemoglobin into the bloodstream. This hemoglobin, when concentrated in urine, results in hemoglobinuria. Anemia arises from the reduced red blood cell count. Fatigue and pallor are symptoms of decreased oxygen-carrying capacity of the blood. |
| Kidneys | Dark urine, Frequent urination, Kidney damage (in severe cases) | Hemoglobinuria, the presence of hemoglobin in urine, leads to dark urine. Increased hemoglobin filtration by the kidneys can strain the organ, potentially causing damage in advanced cases. Increased urination is a potential symptom due to the kidneys’ response to the excess hemoglobin. |
| Liver | Hepatosplenomegaly (enlarged liver and spleen), Jaundice | The increased destruction of red blood cells can lead to an accumulation of bilirubin, a byproduct of hemoglobin breakdown. This can result in jaundice, a yellowing of the skin and eyes. The liver and spleen, which play a role in filtering and processing blood, may become enlarged in response to the increased workload. |
| Gastrointestinal | Abdominal pain, Nausea, Vomiting | The exact mechanisms behind these symptoms in PNH are not fully understood, but some believe that they may be related to the effects of the disease on the liver and spleen, or possibly inflammatory processes. |
| Cardiovascular | Heart failure (in severe cases), Hypertension | The chronic hemolytic anemia in PNH can lead to a reduced blood volume. The body’s compensatory mechanisms to maintain blood pressure can lead to increased blood pressure. Severe cases can eventually cause heart failure. |
Less Common, But Important Symptoms
While the symptoms described above are more frequent, some individuals may experience less common yet important manifestations of PNH. These symptoms, though less prevalent, should not be overlooked as they may signal disease progression or complications.
- Leg ulcers
- Venous thrombosis (blood clots in the veins)
- Aplastic anemia (in severe cases)
- Bone pain
- Frequent infections
Symptom Severity and Disease Stage Correlation
The severity of PNH symptoms can vary significantly among individuals and even within the same individual over time. Factors like the stage of the disease and the presence of complications play a role in symptom intensity.
| Symptom | Mild Stage | Moderate Stage | Severe Stage |
|---|---|---|---|
| Hemoglobinuria | Occasional, mild darkening of urine | Frequent and pronounced darkening of urine | Almost constant and severe darkening of urine |
| Anemia | Mild fatigue, occasional shortness of breath | Significant fatigue, shortness of breath with exertion | Severe fatigue, shortness of breath at rest, significant pallor |
| Thrombosis | Absent or infrequent | Occasional occurrence | Frequent and potentially life-threatening |
Symptoms Related to Hemolysis
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare blood disorder characterized by the destruction of red blood cells. This process, known as hemolysis, leads to a cascade of symptoms that significantly impact a person’s well-being. Understanding the specific symptoms related to hemolysis is crucial for proper diagnosis and management of PNH.Hemolysis in PNH is a direct consequence of the abnormal red blood cells’ inability to withstand the normal stresses of the circulatory system.
The resulting breakdown of these cells releases hemoglobin, a protein responsible for carrying oxygen throughout the body, into the bloodstream. This, in turn, triggers a series of physiological responses that manifest as various symptoms.
Hemoglobinuria: The Connection Between Hemolysis and Urine
The breakdown of red blood cells releases hemoglobin into the bloodstream. Normally, the kidneys filter out and recycle hemoglobin. However, in PNH, the excessive amount of hemoglobin overwhelms the kidneys’ filtering capacity. This leads to hemoglobin spilling into the urine, resulting in a characteristic reddish-brown or dark brown discoloration. This condition is known as hemoglobinuria, and it is often more noticeable at night.
Symptoms Associated with Anemia
Hemolysis in PNH significantly reduces the number of red blood cells, resulting in anemia. The symptoms of anemia are due to the body’s reduced ability to carry oxygen to the tissues. These symptoms may include fatigue, weakness, shortness of breath, pale skin, and dizziness. The severity of these symptoms can vary depending on the extent of hemolysis and the individual’s overall health.
Comparing and Contrasting Hemolysis Symptoms in PNH with Other Forms
While hemolysis is a common thread in various blood disorders, the specific symptoms and their presentation can differ. In PNH, the episodic nature of hemoglobinuria, often occurring at night, and the characteristic reddish-brown or dark brown urine are key distinguishing factors. Other forms of hemolysis may not exhibit these nocturnal patterns or distinct urine coloration. Furthermore, PNH-related anemia often presents with a constellation of symptoms, including the aforementioned fatigue, weakness, and shortness of breath, which are common to many forms of anemia.
A comprehensive medical evaluation is crucial to differentiate the specific cause of hemolysis.
Jaundice in PNH-Related Hemolysis, Paroxysmal nocturnal hemoglobinuria symptoms
Jaundice, a yellowing of the skin and eyes, is a consequence of the accumulation of bilirubin, a byproduct of hemoglobin breakdown. In PNH, the rapid rate of hemolysis leads to a buildup of bilirubin, which can manifest as jaundice. The intensity of jaundice depends on the rate of hemolysis and the individual’s overall health. Individuals with PNH may experience varying degrees of jaundice, from a subtle yellowing to a more pronounced discoloration.
Symptoms Related to Thrombosis
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare blood disorder characterized by the destruction of red blood cells. Beyond the hemolytic symptoms, individuals with PNH face a significantly increased risk of developing blood clots, or thrombosis. This heightened risk stems from abnormalities in the lining of blood vessels and the clotting factors within the blood itself. Understanding the potential locations and types of thrombosis in PNH is crucial for early diagnosis and appropriate management.The abnormal blood cells in PNH can contribute to a hypercoagulable state.
This means the blood is more prone to forming clots, which can lead to serious complications if not addressed promptly. This increased risk of thrombosis is a significant factor in the overall management of PNH and must be considered alongside the hemolytic symptoms.
Experiencing unusual symptoms like fatigue and dark urine could be a sign of paroxysmal nocturnal hemoglobinuria (PNH). Understanding your health insurance, like knowing you need to pay your deductible before receiving care, paying deductible before receiving care , is crucial for navigating medical costs. This can help you prepare for potential expenses related to PNH diagnosis and treatment.
Managing PNH requires careful planning and a proactive approach to healthcare.
Potential Locations for Thrombosis
The risk of thrombosis in PNH isn’t uniform across all blood vessels. Certain areas are more susceptible to clot formation than others, due to a combination of factors including blood flow patterns and the potential for endothelial damage. Understanding these locations helps healthcare professionals identify potential issues early and tailor treatment accordingly.
Types of Thrombosis in PNH
Thrombosis in PNH can manifest in both venous and arterial systems. Venous thrombosis is more common and typically involves deep veins, such as those in the legs. Arterial thrombosis, while less frequent, can affect arteries throughout the body, potentially leading to serious consequences.
Venous Thrombosis in PNH
Venous thrombosis in PNH most frequently occurs in the deep veins of the legs, leading to deep vein thrombosis (DVT). The symptoms of DVT can range from mild discomfort to significant pain and swelling in the affected leg. In some cases, DVT can lead to pulmonary embolism, a potentially life-threatening condition where a blood clot travels to the lungs.
Arterial Thrombosis in PNH
Arterial thrombosis in PNH can occur in various locations throughout the body, such as the heart, brain, or kidneys. The symptoms associated with arterial thrombosis depend on the affected location. For instance, arterial thrombosis in the heart can manifest as angina or a heart attack. Similarly, arterial thrombosis in the brain can lead to stroke.
Comparison to Other Blood Disorders
The risk of thrombosis in PNH is significantly higher compared to other blood disorders, such as iron deficiency anemia or sickle cell disease. The underlying mechanisms contributing to the hypercoagulability in PNH differ from other conditions, making it crucial to tailor management strategies specifically for PNH. This elevated risk necessitates more vigilant monitoring and proactive preventative measures in individuals with PNH.
Table of Potential Thrombosis Locations in PNH
| Location | Type of Thrombosis | Potential Symptoms |
|---|---|---|
| Deep veins (legs) | Deep Vein Thrombosis (DVT) | Pain, swelling, redness, warmth in the affected leg |
| Pulmonary arteries | Pulmonary Embolism (PE) | Shortness of breath, chest pain, cough, rapid heart rate |
| Arteries (heart, brain, kidneys) | Arterial Thrombosis | Angina, heart attack, stroke, kidney failure (depending on location) |
| Other locations (e.g., mesenteric veins, hepatic veins) | Venous thrombosis | Abdominal pain, jaundice, liver dysfunction (depending on location) |
Symptoms Related to the Kidney: Paroxysmal Nocturnal Hemoglobinuria Symptoms
Paroxysmal nocturnal hemoglobinuria (PNH) significantly impacts the kidneys, often leading to a range of complications. The chronic hemolysis characteristic of PNH results in increased amounts of hemoglobin being filtered by the kidneys. This puts a strain on the kidney’s filtering system, potentially leading to damage over time. Understanding these kidney-related symptoms is crucial for early diagnosis and effective management of PNH.
Impact of PNH on Kidney Function
PNH’s impact on kidney function stems from the constant breakdown of red blood cells, releasing hemoglobin into the bloodstream. The kidneys, tasked with filtering waste products, are forced to process an excess of hemoglobin. This overload can lead to a buildup of harmful substances and impair the kidney’s ability to perform its vital functions, including filtering blood, regulating blood pressure, and producing essential hormones.
Symptoms Associated with Kidney Damage in PNH
Kidney damage in PNH often manifests gradually, sometimes without noticeable symptoms in the early stages. However, as the condition progresses, various symptoms can appear. These can include:
- Proteinuria: An increased amount of protein in the urine, often detected through routine urine tests. This is a key indicator of kidney damage, as healthy kidneys filter out most proteins. Proteinuria signifies that the filtering mechanism in the kidneys is compromised.
- Hematuria: The presence of blood in the urine. This can result from damaged blood vessels in the kidneys or from the high levels of hemoglobin circulating through the system. The color of the urine can vary, from slightly reddish to dark brown or even black, depending on the severity of the condition.
- Elevated blood pressure: Kidneys play a vital role in regulating blood pressure. When kidney function is impaired, blood pressure may rise, which further strains the kidneys. This elevated pressure can lead to complications in other organs.
- Edema (swelling): Fluid retention, often evident in the legs, ankles, and feet. This swelling occurs when the kidneys are unable to effectively remove excess fluid from the body.
- Decreased urine output: A reduction in the amount of urine produced can be a sign of impaired kidney function. This is due to the kidneys’ reduced ability to filter waste products effectively.
Potential Kidney-Related Complications
Progressive kidney damage in PNH can lead to serious complications, including:
- Chronic kidney disease (CKD): A gradual loss of kidney function over time, potentially progressing to end-stage renal disease (ESRD). This condition requires dialysis or kidney transplantation for survival.
- End-stage renal disease (ESRD): The final stage of CKD, characterized by the complete loss of kidney function. Individuals with ESRD require dialysis or a kidney transplant to survive.
- Hypertension (high blood pressure): As mentioned earlier, kidney dysfunction often contributes to elevated blood pressure, which can lead to cardiovascular problems.
- Anemia: Reduced red blood cell production can contribute to anemia, which is characterized by a lack of red blood cells.
Mechanisms of PNH’s Effect on Kidney Function
The mechanisms by which PNH affects kidney function are complex. The constant hemolysis releases large amounts of hemoglobin into the bloodstream. This hemoglobin overwhelms the kidneys’ filtering capacity, causing oxidative stress and inflammation within the kidney tissue. The subsequent damage compromises the glomeruli, the tiny filtering units within the kidneys, leading to proteinuria and hematuria.
Paroxysmal nocturnal hemoglobinuria (PNH) symptoms can be surprisingly diverse, ranging from fatigue and back pain to abdominal discomfort. While dealing with these symptoms can be challenging, it’s important to remember that physical therapy after fracture, for example, can also significantly impact your overall well-being. Finding the right approach to manage PNH symptoms, whether through lifestyle adjustments or medical interventions, is key to maintaining a good quality of life.
Learning about the various treatment options, like those explored in physical therapy after fracture , is crucial for navigating this health condition effectively. The key takeaway remains: understanding PNH symptoms and treatment options is essential for effective management.
Table of Specific Kidney Problems in PNH
| Kidney Problem | Potential Severity | Description |
|---|---|---|
| Proteinuria | Mild to severe | Increased protein in the urine, indicative of kidney damage. |
| Hematuria | Mild to severe | Presence of blood in the urine, indicating damage to blood vessels in the kidneys. |
| Elevated Blood Pressure | Potentially severe | Increased blood pressure due to kidney dysfunction, contributing to cardiovascular risk. |
| Decreased Urine Output | Mild to severe | Reduced urine production, signifying impaired kidney function. |
| Edema | Mild to severe | Fluid retention, often evident in the extremities, associated with impaired kidney function. |
Symptoms Related to the Liver
Paroxysmal nocturnal hemoglobinuria (PNH) primarily affects the red blood cells, but its impact can extend to other organs, including the liver. While liver involvement isn’t as prominent a feature as, say, the bone marrow or kidneys, it can still manifest in various ways. Understanding these manifestations is crucial for appropriate diagnosis and management of PNH.Liver dysfunction in PNH is often subtle and may not be immediately apparent.
Early detection requires careful monitoring and a high index of suspicion in patients with PNH. This can involve regular liver function tests and imaging studies, especially if other symptoms like fatigue or abdominal discomfort are present.
Impact of PNH on Liver Function
PNH can impact liver function through a combination of factors. The chronic hemolysis characteristic of PNH leads to increased oxidative stress and the accumulation of potentially harmful substances in the body. This can contribute to inflammation and damage within the liver tissue. Furthermore, the abnormal blood clotting tendencies associated with PNH may lead to the formation of blood clots within the liver’s blood vessels, further compromising its function.
Symptoms Associated with Liver Dysfunction in PNH
Several symptoms can indicate liver involvement in PNH. These symptoms may overlap with other conditions and can vary in severity. Symptoms can include fatigue, abdominal discomfort or pain, jaundice (yellowing of the skin and eyes), and an enlarged liver (hepatomegaly).
Potential Liver Complications in PNH
The potential complications of liver involvement in PNH can range from mild to severe. These include:
- Hepatomegaly: An enlarged liver, which may be detected during a physical examination or through imaging studies. This is often a sign of underlying liver damage.
- Elevated liver enzymes: These enzymes are released into the bloodstream when liver cells are damaged. Elevated levels are a marker of potential liver dysfunction and can be detected through routine blood tests.
- Liver inflammation (hepatitis): PNH can cause inflammation in the liver tissue, potentially leading to inflammation or other forms of liver disease.
- Cirrhosis: In severe or long-standing cases of liver damage, cirrhosis, a condition characterized by scarring of the liver, may develop. This can lead to impaired liver function and a range of complications.
- Portal hypertension: Elevated blood pressure in the portal vein (a vein that carries blood from the digestive organs to the liver) can occur in advanced liver disease, potentially leading to complications such as esophageal varices (enlarged veins in the esophagus) and ascites (fluid buildup in the abdomen).
Mechanisms of PNH’s Effect on Liver Function
The exact mechanisms by which PNH affects liver function are not fully understood. However, research suggests a few key contributing factors:
- Hemolysis: The ongoing destruction of red blood cells releases harmful substances into the bloodstream, potentially damaging liver cells and leading to inflammation.
- Oxidative stress: The byproducts of hemolysis can contribute to oxidative stress, which can further damage liver cells and impair their function.
- Thrombosis: Blood clots within the liver’s blood vessels can interrupt blood flow, depriving the liver tissue of oxygen and nutrients, ultimately causing damage.
Comparison of Liver Symptoms in PNH and Other Liver Diseases
| Symptom | PNH | Other Liver Diseases (e.g., Hepatitis C, Alcoholic Liver Disease) |
|---|---|---|
| Hepatomegaly | Possible, often associated with other symptoms | Common, often associated with inflammation |
| Elevated Liver Enzymes | Possible, often as part of a larger pattern of blood abnormalities | Frequently present, indicating cellular damage |
| Jaundice | Possible, but less common than in other liver diseases | Common, particularly in severe cases |
| Abdominal Pain/Discomfort | Possible, often vague | Can be present, varying in intensity and location |
Symptoms Related to the Nervous System
Paroxysmal nocturnal hemoglobinuria (PNH) can affect various organ systems, including the nervous system. While less common than other PNH symptoms, neurological involvement can manifest in a range of ways, impacting quality of life significantly. Understanding the potential causes and symptoms is crucial for early diagnosis and appropriate management.
Potential Causes of Neurological Issues in PNH
PNH’s primary characteristic is the abnormal breakdown of red blood cells, leading to hemolysis and the release of hemoglobin into the bloodstream. This process can contribute to various neurological problems. Hemoglobin, in high concentrations, can be toxic to the nervous system. Furthermore, the underlying bone marrow defect in PNH can result in the accumulation of abnormal blood components, such as iron overload or inflammatory cytokines, which can further impact neurological function.
The presence of these abnormal blood components can lead to an inflammatory response in the body, potentially affecting the nervous system.
Symptoms Associated with Nervous System Involvement
Neurological symptoms in PNH are often subtle and may vary in severity. They can include a range of issues, affecting different parts of the nervous system. The specific symptoms and their intensity depend on the affected areas and the individual’s overall health. These symptoms are often nonspecific and can be mistaken for other conditions, making early diagnosis challenging.
Examples of Specific Neurological Symptoms
A variety of neurological symptoms can manifest in PNH. These include, but are not limited to:
- Headaches: These can be persistent or episodic and may be accompanied by other symptoms, like dizziness or visual disturbances.
- Seizures: These are characterized by abnormal electrical activity in the brain, potentially leading to temporary loss of consciousness or muscle spasms.
- Peripheral neuropathy: This condition affects the nerves in the extremities, causing numbness, tingling, pain, and weakness in the hands and feet. This is particularly common and can be debilitating.
- Cognitive impairment: This may manifest as difficulty with memory, concentration, or other cognitive functions. This may be subtle and can vary in intensity.
- Visual disturbances: These may include blurred vision, double vision, or difficulty with depth perception.
- Cerebrovascular accidents (strokes): Though less common, strokes can occur in individuals with PNH, often related to abnormal blood clotting.
Severity of Potential Neurological Symptoms
The severity of neurological symptoms in PNH can vary greatly. Some individuals may experience mild, intermittent symptoms, while others may have more severe and persistent problems. Early diagnosis and appropriate management are essential to mitigate the impact of these symptoms on quality of life.
| Symptom | Potential Severity |
|---|---|
| Headaches | Mild to moderate, potentially debilitating with frequency |
| Seizures | Potentially life-threatening, requiring immediate medical intervention |
| Peripheral neuropathy | Mild to severe, often progressive, impacting daily activities |
| Cognitive impairment | Mild to moderate, affecting daily tasks and independence |
| Visual disturbances | Mild to moderate, impacting daily activities and safety |
| Cerebrovascular accidents (strokes) | Potentially life-threatening, causing permanent neurological damage |
Symptoms Related to the Cardiovascular System
PNH’s impact on the cardiovascular system is a significant concern, as the disease can lead to various complications. The abnormal red blood cell destruction and the presence of abnormal blood clots can affect the heart and blood vessels, potentially causing serious health issues. Understanding these cardiovascular symptoms is crucial for early detection and appropriate management.
Impact of PNH on the Cardiovascular System
PNH’s effects on the cardiovascular system stem primarily from hemolysis (destruction of red blood cells) and the increased risk of thrombosis (blood clots). The ongoing destruction of red blood cells can lead to anemia, which puts a strain on the heart. Simultaneously, the tendency towards blood clots can affect blood flow to the heart and other organs, potentially causing damage.
The chronic nature of these processes can contribute to long-term cardiovascular complications.
Potential Cardiovascular Symptoms
Several cardiovascular symptoms can manifest in individuals with PNH. These symptoms may not always be directly related to the disease, but rather a consequence of the underlying condition. Understanding the possible symptoms is vital for individuals with PNH and their healthcare providers.
- Heart Failure: The heart may struggle to pump sufficient blood due to the anemia and possible accumulation of fluid in the heart’s chambers. Symptoms can include shortness of breath, fatigue, and swelling in the legs and ankles. This symptom often develops gradually and can worsen over time if not addressed promptly.
- Arrhythmias: Abnormal heart rhythms can occur due to the impact of PNH on the electrical system of the heart. These irregularities can range from mild palpitations to more serious conditions like atrial fibrillation, potentially leading to blood clots and stroke.
- Peripheral Artery Disease (PAD): Reduced blood flow to the extremities, such as the legs and feet, can result from the formation of blood clots. Symptoms include pain, numbness, and cramping in the affected limbs, especially during exertion. This can lead to poor wound healing and potential limb loss if not managed properly.
- High Blood Pressure: The chronic inflammation and clotting associated with PNH can increase blood pressure. This condition requires careful monitoring and management to prevent further complications.
Symptoms Associated with Heart-Related Issues in PNH
Heart-related issues in PNH can manifest in various ways, reflecting the strain on the cardiovascular system. These issues are frequently linked to the anemia and the increased risk of thrombosis.
- Chest Pain: Pain in the chest, often described as tightness or pressure, can be a sign of reduced blood flow to the heart muscle (ischemia). This symptom may not be directly attributable to PNH but rather to the effects of the underlying condition.
- Shortness of Breath: Difficulty breathing, particularly with exertion, is a common symptom of heart failure. This symptom arises from the heart’s inability to pump enough blood to meet the body’s needs.
- Fatigue: Persistent tiredness and weakness can be a consequence of anemia and the strain on the heart. This symptom is often non-specific and can be linked to various other medical conditions.
Potential Cardiovascular Complications in PNH
The complications of PNH affecting the cardiovascular system can vary in severity and impact. Early detection and intervention are crucial to minimize the severity of these complications.
- Myocardial Infarction (Heart Attack): A heart attack occurs when blood flow to the heart is blocked, potentially leading to permanent damage to the heart muscle. In PNH, this risk is elevated due to the increased risk of thrombosis.
- Stroke: A stroke results from a blockage or rupture of a blood vessel in the brain. The risk of stroke is heightened in PNH due to the increased risk of blood clots.
- Peripheral Vascular Disease: Reduced blood flow to the extremities can lead to complications such as gangrene and limb loss. This is particularly concerning in PNH due to the increased risk of blood clots.
Severity of Potential Cardiovascular Symptoms
The severity of cardiovascular symptoms in PNH can vary significantly. It is crucial to note that these symptoms can range from mild discomfort to life-threatening conditions. Regular monitoring and prompt medical intervention are essential to manage the condition effectively.
| Cardiovascular Symptom | Potential Severity |
|---|---|
| Mild chest pain | Low |
| Shortness of breath with exertion | Moderate |
| Heart failure | High |
| Stroke | High |
Symptoms Related to Bone Marrow
The bone marrow, a vital part of the hematopoietic system, is where blood cells are produced. In Paroxysmal Nocturnal Hemoglobinuria (PNH), the abnormal blood cell production and destruction processes significantly impact the bone marrow, leading to various symptoms. Understanding these effects is crucial for effective management and care.
Impact of PNH on Bone Marrow
PNH’s primary effect on the bone marrow is a disruption in the normal production of healthy blood cells. This disruption stems from the underlying genetic defect, which affects the stem cells responsible for creating red blood cells, white blood cells, and platelets. The defective stem cells are often more susceptible to damage and destruction, further hindering blood cell production.
Symptoms Associated with Bone Marrow Involvement
Bone marrow involvement in PNH often manifests as a reduction in the production of healthy blood cells. This can lead to various symptoms, ranging from mild fatigue to severe anemia and increased susceptibility to infections. The impact on blood cell counts is a crucial indicator of bone marrow function.
Potential Bone Marrow-Related Complications
Several complications can arise from the bone marrow’s compromised function in PNH. These include, but are not limited to, anemia, infections, and an increased risk of blood clots. The severity and nature of these complications can vary greatly among individuals, depending on the extent of the bone marrow damage and the overall health of the patient.
- Anemia: Reduced red blood cell production results in a lower-than-normal concentration of hemoglobin in the blood. This leads to fatigue, weakness, shortness of breath, and pale skin.
- Leukopenia: Decreased production of white blood cells can impair the immune system’s ability to fight off infections. This increases the risk of developing various types of infections.
- Thrombocytopenia: Lower platelet counts can increase the risk of bleeding, bruising, and prolonged bleeding after injuries.
- Bone Marrow Failure: In severe cases, the bone marrow’s ability to produce blood cells can completely fail, leading to aplastic anemia, a life-threatening condition.
Mechanisms of PNH Affecting Bone Marrow Function
The underlying genetic defect in PNH leads to the abnormal expression of proteins on the surface of blood stem cells. This abnormal expression makes the cells vulnerable to premature destruction by the complement system, a part of the body’s immune system. This constant destruction of stem cells disrupts the normal hematopoietic process, leading to a decrease in the production of all blood cell types.
The complement system, crucial for immune defense, mistakenly attacks and destroys the abnormal PNH blood cells, which impacts bone marrow function and blood cell production.
Symptoms Associated with Bone Marrow Suppression in PNH
Bone marrow suppression in PNH can present with a wide range of symptoms, often reflecting the reduced production of various blood cell types. These symptoms can include fatigue, pallor, easy bruising, recurrent infections, and shortness of breath. Monitoring blood counts is crucial for assessing the severity of bone marrow suppression and tailoring treatment strategies.
Closing Summary
In conclusion, paroxysmal nocturnal hemoglobinuria symptoms present a multifaceted challenge, affecting numerous bodily systems. From the initial signs of hemolysis to the potential for thrombosis and organ damage, understanding these symptoms is critical for early detection and appropriate treatment. This detailed exploration provides valuable insight into the complexities of PNH, offering a more complete picture for patients and healthcare professionals alike.




