Palliative care vs hospice: understanding the nuances between these two approaches to end-of-life care is crucial. Palliative care focuses on improving quality of life for anyone with a serious illness, regardless of prognosis. Hospice care, on the other hand, is specifically for people with a life expectancy of six months or less, prioritizing comfort and support in their final stages.
This exploration delves into the key distinctions, eligibility criteria, goals, and care settings to help you understand when and how each approach might be beneficial.
A crucial distinction lies in the timing of care. Palliative care can be integrated into treatment at any stage of a serious illness, whereas hospice care is usually sought when curative treatment is no longer an option. The focus on symptom management is common to both, but hospice care shifts its emphasis to comfort and support during the final stages of life.
This blog post will break down the critical aspects of each, highlighting when one might be a more suitable choice than the other.
Introduction to Palliative and Hospice Care

Palliative and hospice care are crucial components of the healthcare system, providing comfort and support to individuals facing serious illnesses. They represent a compassionate approach to care, focusing on improving quality of life rather than solely on extending life. These specialized services offer comprehensive support for patients and their families, addressing physical, emotional, social, and spiritual needs.
Definitions of Palliative and Hospice Care
Palliative care is specialized medical care for people with serious illnesses. It focuses on providing relief from the symptoms and stress of the illness. It is appropriate at any age and at any stage of a serious illness and can be provided alongside curative treatment. Hospice care is a type of palliative care that focuses on the care of terminally ill patients.
It provides comfort and support for patients in their final stages of life. Hospice care emphasizes quality of life and symptom management rather than curative treatment.
Key Differences
Palliative care can be provided alongside curative treatments, whereas hospice care is for patients where curative treatment is no longer considered beneficial or desired. Palliative care can be provided at any stage of a serious illness, while hospice care is for those with a life expectancy of six months or less. A key difference lies in the focus on the trajectory of the disease and the type of care being offered.
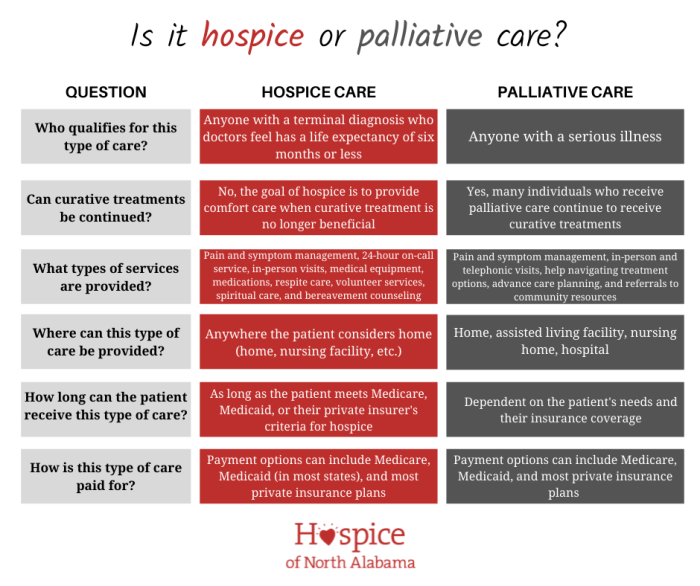
Comparison Table
| Characteristic | Palliative Care | Hospice Care |
|---|---|---|
| Eligibility Criteria | Individuals with serious illnesses, at any stage. | Individuals with a life expectancy of six months or less, as determined by a physician. |
| Focus | Symptom management, improving quality of life, and providing support for patients and families. | Providing comfort and support for the patient and family during the final stages of life. |
| Treatment Goals | Improving quality of life and managing symptoms, potentially alongside curative treatments. | Managing symptoms, providing comfort, and supporting the emotional and spiritual needs of the patient and family. |
| Duration | Can be provided throughout the course of the illness. | Typically for the duration of the patient’s life expectancy of six months or less. |
| Setting | Can be provided in hospitals, clinics, outpatient settings, or at home. | Can be provided in hospitals, skilled nursing facilities, hospice facilities, or at home. |
Eligibility Criteria and Patient Needs: Palliative Care Vs Hospice
Palliative care and hospice care, while both focusing on comfort and quality of life for individuals facing serious illness, differ significantly in their eligibility criteria and the types of support they offer. Understanding these distinctions is crucial for navigating the complex landscape of end-of-life care and making informed decisions. Choosing the right path depends heavily on individual needs and the stage of the illness.Eligibility for these programs is often based on factors like the prognosis of the illness, the patient’s overall health, and the support system available to them.
Both approaches are designed to enhance the patient’s experience and minimize the emotional burden on families.
Types of Patients Benefiting from Palliative Care
Palliative care is designed to improve the quality of life for anyone facing a serious illness, regardless of prognosis or life expectancy. This includes patients with conditions like cancer, heart failure, chronic obstructive pulmonary disease (COPD), Alzheimer’s disease, multiple sclerosis, and many others. Importantly, palliative care can be integrated with curative treatments, offering support and symptom management throughout the entire course of the illness.
For example, a patient undergoing chemotherapy for cancer might receive palliative care to manage side effects like nausea and fatigue, improving their overall well-being.
Types of Patients Benefiting from Hospice Care
Hospice care, on the other hand, is focused on patients with a life expectancy of six months or less, if the disease runs its normal course. It emphasizes comfort and support during the final stages of life. Patients in this stage often experience progressive decline and may require more intensive symptom management. This approach prioritizes quality of life over curative treatment.
A patient with advanced lung cancer, for instance, whose doctors estimate they have six months or less to live, would be a good candidate for hospice care.
Eligibility Criteria for Palliative Care
Palliative care is not tied to a specific prognosis and can be accessed at any point during a serious illness. A patient’s physician plays a vital role in determining eligibility. They assess the patient’s overall health status, the severity of their symptoms, and the need for supportive care, making a comprehensive judgment on the patient’s eligibility. Factors like the presence of complex symptoms (pain, breathlessness, nausea) and the need for emotional and psychological support are also considered.
Understanding palliative care versus hospice care can be tricky, especially when considering the patient’s overall health. While both focus on comfort and quality of life, palliative care can be integrated into ongoing treatment for conditions like high blood pressure, offering support alongside existing therapies. High blood pressure facts often highlight the importance of managing this condition, and that’s precisely where palliative care excels, helping patients cope with the physical and emotional impacts of this and other chronic illnesses.
Ultimately, the choice between palliative and hospice care depends on the individual’s specific needs and the progression of their condition.
Eligibility Criteria for Hospice Care
Hospice care, in contrast, is specifically designed for patients with a life expectancy of six months or less. This prognosis is determined by the patient’s physician based on their medical history, current condition, and the progression of the disease. The physician considers the patient’s condition, expected course of the illness, and the likelihood of a recovery. A formal evaluation process often involves consultations with multiple healthcare professionals.
Support Needs of Patients Undergoing Palliative Care
Patients receiving palliative care have a wide range of support needs, often spanning physical, emotional, and social domains. These needs may include symptom management (pain, nausea, shortness of breath), practical assistance with daily tasks, and emotional support for the patient and their family. For example, patients might require help with managing medications, adjusting to changes in their physical abilities, or dealing with anxieties related to their illness.
Support Needs of Patients Undergoing Hospice Care
Hospice care focuses on the holistic support of patients and their families during the final stages of life. This includes addressing physical symptoms, providing emotional and spiritual support, and facilitating meaningful connections with loved ones. Family members often need guidance on practical matters like managing caregiving responsibilities, grief counseling, and bereavement support.
Key Differences in Eligibility Requirements
| Characteristic | Palliative Care | Hospice Care |
|---|---|---|
| Life Expectancy | No specific timeframe; available at any point during a serious illness | Generally, six months or less if the disease runs its normal course |
| Treatment Focus | Supports curative treatment and improves quality of life | Focuses on comfort and quality of life during the final stages of life |
| Eligibility Determination | Determined by the patient’s physician based on their overall health and symptom management needs. | Determined by the patient’s physician based on their estimated life expectancy and the expected course of the disease. |
Goals and Treatment Approaches
Palliative and hospice care offer distinct yet interconnected approaches to support individuals facing serious illnesses. Understanding their shared and unique goals is crucial for selecting the most appropriate care pathway. Both aim to enhance quality of life, but they differ in the stage of illness they address and the duration of care provided.These care models are deeply personal and tailored to individual needs.
They prioritize patient preferences and values, ensuring the care aligns with their goals and wishes. This personalized approach emphasizes comfort, dignity, and support for patients and their families.
Figuring out palliative care versus hospice can be tricky, but essentially, palliative care focuses on comfort and symptom management for any serious illness, at any stage. Meanwhile, hospice care is specifically for people with a terminal illness, often with a life expectancy of six months or less. It’s all about providing support, but the timing and focus differ.
Just like using salt water for the face to soothe and refresh, choosing the right care path requires understanding your needs and goals, and aligning them with the services offered by each approach. Ultimately, both approaches aim to improve quality of life during challenging times.
Palliative Care Goals
Palliative care focuses on improving the quality of life for individuals facing serious illnesses, regardless of the stage of the disease or the need for curative treatment. The primary goal is to prevent and relieve suffering through the management of symptoms, such as pain, shortness of breath, nausea, and anxiety. It also addresses emotional, social, and spiritual needs.
This comprehensive approach considers the patient’s physical, psychological, and social well-being, aiming to enhance their overall quality of life.
Hospice Care Goals
Hospice care is specifically designed for individuals with a life expectancy of six months or less. The primary goal is to provide comfort and support during the final stages of life. This involves managing symptoms, providing emotional and spiritual support, and helping patients and families navigate the emotional complexities of end-of-life care. Hospice care emphasizes quality of life, but recognizes that curative treatments may no longer be appropriate or desired.
Treatment Approaches Comparison
Both palliative and hospice care utilize a range of medical interventions, therapies, and supportive services. However, their approaches differ based on the patient’s prognosis. Palliative care can be integrated into curative treatments, while hospice care focuses on comfort measures.
Common Medical Interventions
Common medical interventions in both palliative and hospice care include pain management strategies, medication adjustments to manage symptoms, and symptom-specific therapies. These approaches are often tailored to the individual patient’s needs and preferences. For instance, a patient experiencing severe pain might receive a combination of oral analgesics and potentially stronger opioid medications.
Therapies and Supportive Services
These approaches recognize the importance of addressing physical, emotional, and spiritual needs.
| Therapy/Service | Palliative Care | Hospice Care |
|---|---|---|
| Medical Management | Active participation in curative treatments while managing symptoms. | Focus on comfort measures and symptom management, with curative treatments generally ceased. |
| Pain Management | Comprehensive pain assessment and management, potentially including medications and non-pharmacological interventions. | Emphasis on effective pain control, prioritizing comfort and minimizing suffering. |
| Symptom Management | Active symptom management to improve quality of life, addressing various symptoms like shortness of breath, nausea, and fatigue. | Symptom management to maintain comfort and minimize discomfort. |
| Counseling | Support for patients and families to cope with emotional and psychological challenges. | Emotional and spiritual support for patients and families. |
| Social Work | Assistance with practical needs, such as financial resources and access to community services. | Assistance with practical needs, including financial aid, grief counseling, and support for families. |
| Spiritual Counseling | Support to address spiritual needs and concerns. | Support to address spiritual needs and concerns. |
| Physical Therapy | Maintaining mobility and function. | Maintaining comfort and dignity through physical therapy to the extent possible. |
| Occupational Therapy | Improving daily living skills. | Adapting daily living skills to the patient’s current abilities. |
| Complementary Therapies | Exploring complementary therapies to enhance comfort. | Exploring complementary therapies to enhance comfort and well-being. |
Interdisciplinary Team
A key component of both palliative and hospice care is the interdisciplinary team. This team, which includes physicians, nurses, social workers, counselors, and spiritual advisors, works collaboratively to meet the holistic needs of the patient and family. The team’s expertise ensures comprehensive care, addressing the physical, emotional, social, and spiritual dimensions of the patient’s experience. The collaborative nature of the team is critical in ensuring coordinated care, tailored to the unique needs of each patient and their family.
Care Setting and Delivery Models
Palliative and hospice care encompass a wide range of settings and delivery models, tailored to meet the diverse needs of patients and families. Understanding these variations is crucial for ensuring appropriate and effective care. This section will explore the common settings for both types of care, the delivery models used, and the key personnel involved.Palliative care, unlike hospice, is not time-limited.
This flexibility allows for the possibility of transitioning between settings and care models as the patient’s needs evolve. This contrasts with hospice, which is typically focused on the final stages of a terminal illness.
Common Care Settings
Palliative care can be provided in various settings, accommodating different patient needs and preferences. These settings often include hospitals, clinics, and patient homes. Hospice care, however, is primarily focused on the patient’s home.
- Hospitals: In acute care settings, palliative care teams collaborate with the medical staff to manage symptoms, provide emotional support, and coordinate care, especially for patients with serious illnesses. Hospitals often have designated palliative care units or consult services to support patients facing complex medical situations.
- Clinics: Palliative care clinics offer specialized outpatient services, allowing for ongoing management of chronic conditions and symptom control. This model can provide regular checkups, medication adjustments, and counseling to patients and their families.
- Patient Homes: Home-based palliative care is a common approach, enabling patients to receive care in their familiar surroundings. This approach often involves visiting nurses, therapists, and social workers, ensuring comfort and continuity of care.
- Hospice Care Settings: Hospice care is predominantly provided in the patient’s home. This allows patients to remain in a familiar environment while receiving comprehensive support and care. While hospice care is usually home-based, there may be instances where a patient may require temporary placement in a hospice facility for specialized care or symptom management.
Delivery Models for Palliative Care
Palliative care services utilize various delivery models to cater to the diverse needs of patients. These models aim to provide comprehensive care, coordinating the efforts of different healthcare professionals.
- Consultative Model: In this model, palliative care specialists act as consultants to the primary care team. They provide expertise in symptom management and support to the patient and their family, integrating their knowledge with the ongoing care plan.
- Interdisciplinary Team Model: This model emphasizes collaboration among various healthcare professionals, including doctors, nurses, social workers, and chaplains. The team approach ensures holistic care, addressing physical, emotional, and spiritual needs.
- Integrated Model: In this approach, palliative care is seamlessly integrated into the overall healthcare system. This integration streamlines care coordination and improves communication among different providers.
Delivery Models for Hospice Care
Hospice care services focus on providing comfort and support during the final stages of a terminal illness. The delivery models for hospice care are typically designed around the patient’s home environment.
- Home-Based Care: Hospice care primarily involves visiting nurses, aides, and other support personnel to the patient’s home. This model allows patients to remain in their familiar surroundings, minimizing the disruption of their routine.
- Hospice Facilities: Some hospice programs may have designated facilities for patients who require more intensive care or specialized support. These facilities provide a supportive environment for patients and their families, offering temporary respite or specialized care.
Key Personnel
A diverse range of personnel is involved in palliative and hospice care. Their roles are crucial in ensuring the well-being of patients and their families.
- Physicians: Physicians, including oncologists, internists, and specialists, play a vital role in assessing patients’ needs, coordinating care, and managing symptoms.
- Nurses: Nurses, including registered nurses and licensed practical nurses, provide hands-on care, monitor symptoms, and educate patients and families.
- Social Workers: Social workers help patients and families navigate the emotional and practical challenges associated with illness and loss. They assist with financial resources, caregiver support, and emotional counseling.
- Chaplains/Spiritual Counselors: Chaplains or spiritual counselors offer support for patients’ spiritual and emotional needs.
- Other Personnel: Other key personnel involved in palliative and hospice care include therapists, volunteers, and administrative staff.
Support Systems
Effective support systems are essential for both palliative and hospice care. These systems help patients and families cope with the challenges of illness and loss.
| Support System Type | Description |
|---|---|
| Emotional Support Groups | These groups provide a platform for patients and families to share experiences, offer mutual support, and cope with emotional challenges. |
| Financial Assistance Programs | These programs help patients and families with financial burdens associated with medical expenses. |
| Volunteer Programs | Volunteers provide companionship, practical assistance, and emotional support to patients and families. |
| Family Counseling | Family counseling provides guidance and support to family members navigating the challenges of a loved one’s illness. |
| Respite Care Services | Respite care allows caregivers to take breaks from their responsibilities, ensuring their own well-being while providing temporary relief for patients. |
Emotional and Spiritual Support
Navigating the complexities of serious illness, particularly in palliative and hospice care, demands a multifaceted approach that extends beyond physical treatment. Emotional and spiritual well-being play a critical role in the overall quality of life for patients and their families. This support system fosters resilience, coping mechanisms, and a sense of peace during challenging times. Understanding the nuances of these needs is essential for providing compassionate and effective care.
Importance of Emotional Support
Emotional support is paramount for patients and families facing life-limiting illnesses. The emotional toll of a diagnosis, treatment, and the eventual end-of-life journey can be profound. Providing a safe space for expressing feelings, whether grief, fear, or anxiety, is crucial. Open communication channels, empathetic listening, and validation of emotions foster a sense of connection and alleviate feelings of isolation.
For families, emotional support is equally vital, encompassing shared experiences, mutual support, and opportunities to process the challenges together.
Methods of Providing Emotional Support in Palliative Care
A range of methods contribute to providing comprehensive emotional support in palliative care. These include:
- Active listening and empathy: Creating a supportive environment where patients feel heard and understood is paramount. Non-judgmental listening and validation of emotions are key components of effective communication.
- Individual and family counseling: Professional counseling provides a structured platform for patients and families to address emotional challenges, process grief, and develop coping strategies. This may include individual sessions with the patient and/or family therapy sessions.
- Support groups: Connecting with others facing similar experiences can be tremendously helpful. Support groups offer a safe space for sharing experiences, offering mutual encouragement, and reducing feelings of isolation.
- Art therapy and music therapy: These creative outlets can provide avenues for expressing emotions and managing stress in a non-verbal way. They can be particularly helpful for patients who may find it difficult to articulate their feelings.
Methods of Providing Emotional Support in Hospice Care
In hospice care, emotional support is often intertwined with the acceptance of the end-of-life journey. Approaches focus on providing comfort and support during this final stage:
- Symptom management: Effective pain and symptom management directly impacts a patient’s emotional state. Addressing physical discomfort minimizes distress and allows for greater emotional well-being.
- Presence and companionship: The simple act of being present, offering a listening ear, and providing companionship can be incredibly powerful in easing anxieties and providing comfort.
- Family meetings: Regular meetings with families provide opportunities to address concerns, discuss goals, and foster a sense of unity and shared understanding.
- Bereavement support: Hospice care extends beyond the patient’s life to support the family during the grieving process. Offering grief counseling and support groups after the patient’s passing is essential.
Addressing Spiritual Concerns in Palliative Care
Palliative care acknowledges the diverse spiritual needs of patients. Addressing these needs can improve overall well-being and facilitate acceptance of the situation.
- Open and respectful dialogue: Creating a safe space for patients to express their spiritual beliefs and concerns is essential.
- Referral to spiritual advisors: Connecting patients with clergy, spiritual leaders, or other faith advisors can provide comfort and guidance. This may involve referring patients to chaplains or other religious professionals.
- Facilitating spiritual practices: Supporting patients in maintaining or resuming spiritual practices, such as prayer, meditation, or rituals, can offer comfort and a sense of peace.
Addressing Spiritual Concerns in Hospice Care
Hospice care recognizes the importance of spirituality in the final stages of life. Strategies focus on supporting patients in finding peace and acceptance:
- Facilitating end-of-life rituals: Respecting and facilitating cultural or religious end-of-life rituals can offer comfort and closure.
- Addressing existential questions: Providing opportunities for patients to explore and address questions about life, death, and meaning can help them find peace and acceptance.
- Promoting hope and peace: Focusing on the positive aspects of the patient’s life, providing comfort, and promoting a sense of hope and peace can help ease anxieties and encourage acceptance.
Support Groups for Patients and Families
A variety of support groups cater to the needs of patients and families in palliative and hospice settings. These groups provide a safe and supportive environment for shared experiences and mutual understanding.
| Type of Support Group | Description | Palliative Care | Hospice Care |
|---|---|---|---|
| Grief Support Groups | Offer a space for individuals to grieve and share experiences with others. | Yes | Yes |
| Family Support Groups | Focus on supporting families facing the challenges of a loved one’s illness. | Yes | Yes |
| Patient Support Groups | Provide a space for patients to connect with others experiencing similar conditions. | Yes | Yes |
| Spiritual Support Groups | Offer a space for individuals to discuss spiritual concerns and beliefs. | Yes | Yes |
| Peer Support Groups | Led by individuals who have similar experiences. | Yes | Yes |
Ethical Considerations and Decision Making
Navigating the complexities of end-of-life care requires careful consideration of ethical principles and patient preferences. Both palliative care and hospice care aim to enhance quality of life and support individuals and families during this challenging period. However, ethical dilemmas often arise, demanding thoughtful consideration and a commitment to shared decision-making.
Ethical Considerations in Palliative Care
Palliative care focuses on providing relief from the symptoms and stress of a serious illness at any stage. Ethical considerations in palliative care encompass the principles of beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), respect for autonomy (respecting patient choices), and justice (fair distribution of resources). A key ethical challenge lies in balancing aggressive symptom management with the potential for hastening death.
Decisions must be made with sensitivity to the patient’s values, preferences, and goals, recognizing that the patient may not always be fully capable of articulating their wishes.
Ethical Considerations in Hospice Care
Hospice care focuses on comfort and support for individuals in the final stages of a life-limiting illness. Ethical dilemmas in hospice often center on decisions about the use of life-sustaining treatments, pain management strategies, and the patient’s right to self-determination. A critical ethical aspect is ensuring that patients receive the most appropriate level of care and support, while also respecting their autonomy and the wishes of their families.
Advance Directives and Patient Preferences in Palliative Care
Advance directives, such as living wills and durable powers of attorney for healthcare, are crucial in palliative care. These documents allow patients to articulate their preferences regarding medical interventions, treatment choices, and end-of-life care, empowering them to make decisions that align with their values. Effective communication between patients, families, and healthcare providers is paramount in understanding and honoring these directives.
For example, a patient’s advance directive might specify a preference for comfort care over aggressive life-sustaining treatments, enabling healthcare professionals to respect their wishes.
Advance Directives and Patient Preferences in Hospice Care
Similar to palliative care, advance directives are essential in hospice care to guide decisions. Hospice care emphasizes the patient’s right to make choices about their care, including the timing and nature of their passing. This includes the choice of pain management strategies, the use of life-sustaining treatments, and the overall comfort and support system. Patients in hospice care, while facing the end of their lives, maintain their right to self-determination, as expressed through advance directives.
If a patient has not completed advance directives, the family and care team work collaboratively to discern the patient’s wishes based on their values and past discussions.
Challenges in End-of-Life Decision Making
Common challenges in end-of-life decision-making in both palliative and hospice care include disagreements among family members, uncertainty regarding the patient’s wishes, and the emotional distress surrounding the process. Healthcare professionals must be equipped to navigate these complex situations with empathy and sensitivity. For example, conflicting family opinions on treatment options can lead to significant emotional distress and ethical dilemmas.
Importance of Communication and Shared Decision Making
Open and honest communication between patients, families, and healthcare professionals is paramount in end-of-life decision-making. Shared decision-making fosters a collaborative approach, ensuring that decisions reflect the patient’s values and preferences. This approach involves actively listening to patients and families, providing clear information about treatment options, and collaboratively developing a plan that respects everyone’s perspectives. For example, a patient might express a desire to remain at home for their final days.
A shared decision-making process could then explore ways to provide this level of care, while also acknowledging potential challenges and developing solutions.
Legal and Ethical Frameworks
| Area | Palliative Care | Hospice Care |
|---|---|---|
| Legal Framework | Generally guided by state laws related to healthcare decision-making, including advance directives and surrogate decision-making. | Often governed by specific hospice regulations and laws that address end-of-life care, potentially with distinct guidelines compared to general healthcare law. |
| Ethical Framework | Guided by principles of beneficence, non-maleficence, respect for autonomy, and justice, as well as ethical guidelines for healthcare professionals. | Similar ethical framework to palliative care, emphasizing the unique aspects of end-of-life care, particularly comfort and dignity. |
Cost and Funding Considerations
Navigating the financial landscape of palliative and hospice care can be daunting for patients and families. Understanding the associated costs, funding sources, and payment options is crucial for making informed decisions. This section delves into the financial realities of these vital support systems.The costs of both palliative and hospice care can vary significantly depending on the level of services required, the geographic location, and the specific needs of the patient.
These expenses can encompass a range of elements, including physician visits, medications, medical equipment, and home care services. Comprehending these factors allows for a more realistic appraisal of the financial implications involved.
Costs Associated with Palliative Care
Palliative care services are often integrated into ongoing treatment plans, and the costs can vary greatly. The costs can encompass physician visits, therapies, medications, and other medical supplies, potentially adding to existing healthcare expenses. The involvement of specialists, such as pain management specialists, can also contribute to the overall financial burden. Since palliative care isn’t a standalone entity, it’s often bundled with other healthcare services, making precise cost calculations challenging.
Costs Associated with Hospice Care
Hospice care focuses on comfort and quality of life during the final stages of a terminal illness. The costs of hospice care typically cover services like nursing care, medical equipment, medications, and bereavement counseling. These services are generally focused on easing symptoms and improving the patient’s comfort. A critical factor is the potential for significant cost reduction when compared to continuing curative treatment.
Funding Sources for Palliative Care
Funding for palliative care often originates from various sources, reflecting its integration with ongoing medical care. These may include private insurance, Medicare (for eligible patients), Medicaid, and sometimes charitable foundations or grants. The exact funding mix depends on the specific circumstances of each patient.
Funding Sources for Hospice Care
Medicare and Medicaid are the primary funding sources for hospice care, covering a significant portion of the expenses. Private insurance policies may also contribute, though coverage varies. In some cases, charitable organizations or community support groups may play a role in supporting hospice care services.
Payment Options for Palliative and Hospice Care
Numerous payment options exist for both palliative and hospice care. Patients and families should investigate their insurance coverage, including co-pays, deductibles, and out-of-pocket maximums. Medicare and Medicaid programs offer benefits, and in some instances, financial assistance programs from healthcare providers or non-profit organizations might be available.
Financial Implications for Patients and Families
The financial implications for patients and families can be significant, particularly in cases of prolonged illness or complex medical needs. Families should carefully review their insurance policies and explore potential financial assistance programs. Pre-planning can help mitigate some of these financial burdens.
Role of Insurance Coverage
Insurance coverage plays a crucial role in both palliative and hospice care. The extent of coverage depends on the type of insurance, and specific policies may have different stipulations. Understanding the nuances of insurance plans is essential for navigating the financial aspects of care.
Comparison of Costs and Funding, Palliative care vs hospice
| Characteristic | Palliative Care | Hospice Care |
|---|---|---|
| Primary Funding Sources | Private insurance, Medicare, Medicaid, charitable foundations | Medicare, Medicaid, private insurance |
| Cost Variability | Highly variable, often integrated into existing care | Generally more predictable, focused on end-of-life care |
| Payment Options | Co-pays, deductibles, out-of-pocket maximums, potential for financial assistance programs | Co-pays, deductibles, out-of-pocket maximums, financial assistance programs (Medicare/Medicaid) |
| Patient/Family Impact | Potentially adding to existing medical costs | Potential cost reduction compared to curative treatment; focuses on comfort and quality of life |
Last Recap
In conclusion, understanding the differences between palliative care and hospice care is essential for informed decision-making during challenging times. Both aim to enhance quality of life and provide support, but they do so in distinct ways. Palliative care offers comprehensive symptom management and support at any point during a serious illness, while hospice care focuses on comfort and support during the final stages of life.
By recognizing these differences, individuals and families can make the best decisions for their specific needs and circumstances.




