Overview of West Nile virus, a mosquito-borne illness, is crucial for understanding its impact. This comprehensive guide delves into the various aspects of this viral infection, from its geographical spread and transmission methods to its symptoms, prevention strategies, and the role of public health measures. We’ll explore the science behind the virus, the human health implications, and the ongoing research efforts to combat this disease.
The virus’s geographical distribution varies, and understanding its prevalence in different regions is key. This article will cover the different forms of transmission, from the life cycle of the mosquito vector to human-to-human transmission (if applicable). We will also discuss the range of symptoms, from mild to severe, and the diagnostic methods used to identify the infection.
Introduction to West Nile Virus
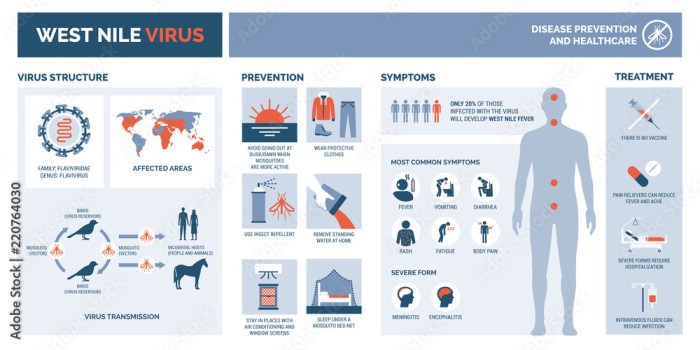
West Nile virus (WNV) is a mosquito-borne flavivirus that can cause a range of illnesses in humans, from mild symptoms to severe neurological complications. Understanding its transmission, prevalence, and historical impact is crucial for developing effective prevention strategies and managing outbreaks. This overview provides a comprehensive understanding of WNV, its impact, and its potential risks.WNV primarily affects birds, but it can also infect humans and other mammals.
The virus is transmitted to humans primarily through the bite of infected mosquitoes. Understanding the virus’s life cycle, its interactions with different hosts, and the specific mosquito species involved is essential to preventing transmission.
Geographical Distribution and Prevalence
WNV is prevalent in many parts of the world, including the Americas, Europe, Africa, and Asia. Its distribution is closely linked to the geographic range of the mosquito vectors that transmit the virus. Areas with warm climates and abundant standing water, which support mosquito breeding, are particularly susceptible to WNV outbreaks. For instance, the prevalence in the United States fluctuates annually, with certain regions experiencing more frequent outbreaks.
West Nile virus, a mosquito-borne illness, has been making headlines. Understanding how our immune systems respond to various infections is key. Factors like immunity duration after COVID booster shots immunity duration after covid booster can significantly influence our overall health and response to diseases like West Nile. Fortunately, the majority of people who contract West Nile virus experience mild symptoms, but it’s crucial to stay informed and take necessary precautions.
Transmission of West Nile Virus
The primary mode of transmission is the bite of an infected mosquito. The virus multiplies in the mosquito’s salivary glands, and when the mosquito feeds on a human or animal host, it transmits the virus. The mosquito must be infected to transmit the virus; not all mosquitoes are infected. Other modes of transmission, such as blood transfusions or organ transplants, are extremely rare.
However, the risk of transmission through these routes is significantly lower than via mosquito bites.
Historical Overview of West Nile Virus Outbreaks
The first documented WNV outbreak in the Western Hemisphere occurred in the United States in 1999. The virus quickly spread across the continent, causing significant public health concerns. Subsequent outbreaks have demonstrated the virus’s adaptability and the importance of public health interventions to mitigate its impact. Understanding past outbreaks and their characteristics helps predict future patterns and develop effective control measures.
Comparison with Other Mosquito-Borne Illnesses
| Characteristic | West Nile Virus (WNV) | Malaria | Dengue | Zika |
|---|---|---|---|---|
| Agent | Flavivirus | Protozoan parasite | Flavivirus | Flavivirus |
| Transmission | Mosquito bite | Mosquito bite | Mosquito bite | Mosquito bite |
| Symptoms | Fever, headache, body aches, sometimes neurological complications | Fever, chills, headache, muscle aches, anemia | Fever, headache, muscle aches, rash, severe complications | Fever, rash, conjunctivitis, potential severe complications in pregnant women |
| Severity | Generally mild, but can be severe in some cases | Can be fatal if not treated | Can be fatal if not treated | Can be fatal if not treated; severe complications in pregnant women |
This table provides a concise comparison of WNV to other significant mosquito-borne diseases. Each disease has unique characteristics, symptoms, and potential severity, requiring distinct preventative and treatment approaches. This comparison highlights the importance of comprehensive public health measures in controlling the spread of these illnesses.
Symptoms and Diagnosis
West Nile Virus (WNV) infection can range from completely asymptomatic to severe neurological illness. Understanding the spectrum of symptoms and the diagnostic process is crucial for timely intervention and treatment. Early recognition is vital to prevent serious complications.
Symptom Presentation
The symptoms of WNV infection can vary greatly in severity and presentation. A significant number of people infected with WNV exhibit no symptoms at all, making it difficult to track the true prevalence of the virus. This asymptomatic nature underscores the importance of mosquito control measures.
- Mild Symptoms: Many individuals experience only mild symptoms, such as fever, headache, body aches, fatigue, and skin rash. These symptoms often resemble the flu and can last for a few days to a couple of weeks. For example, someone might experience a slight fever and headache, but otherwise feel well enough to carry on with their daily routine.
- Severe Symptoms: A smaller percentage of infected individuals develop more severe symptoms, including encephalitis (inflammation of the brain) or meningitis (inflammation of the membranes surrounding the brain and spinal cord). These neurological complications can lead to significant health issues, such as seizures, tremors, muscle weakness, confusion, disorientation, and even coma. In severe cases, permanent neurological damage can occur.
Symptom Identification
Identifying WNV symptoms is challenging, particularly in the early stages. Many symptoms are non-specific, meaning they could be indicative of various illnesses. It’s crucial to consider the possibility of WNV if a person presents with a combination of fever and neurological symptoms, especially if there’s a known risk of WNV exposure (e.g., travel to an endemic area, mosquito bites).
Diagnostic Methods
Several methods are employed to diagnose WNV infection. Blood tests are commonly used to detect the presence of WNV antibodies or viral RNA. These tests can confirm the diagnosis and distinguish WNV from other similar illnesses.
- Antibody Tests: These tests look for antibodies produced by the body’s immune system in response to the virus. Positive results indicate a past or present infection. However, the presence of antibodies does not always correlate with the severity of the illness.
- PCR Tests: Polymerase Chain Reaction (PCR) tests directly detect the genetic material of the virus in blood or cerebrospinal fluid (CSF). This method is particularly useful in the early stages of infection, when antibody levels might not be elevated. A positive PCR result strongly suggests an active WNV infection.
Timeline of Symptom Development
The timeline for symptom development following WNV infection varies. Incubation periods can range from 2 to 14 days, although most people develop symptoms within 2 to 10 days.
Comparison of Symptoms
| Symptom | West Nile Virus | Other Viral Illnesses (e.g., Flu, Chikungunya) |
|---|---|---|
| Fever | Common, often high | Common |
| Headache | Common | Common |
| Body Aches | Common | Common |
| Fatigue | Common | Common |
| Encephalitis/Meningitis | Possible, severe | Uncommon or less severe |
| Seizures | Possible, severe | Uncommon or less severe |
Note: This table provides a general comparison. Individual experiences and symptom severity can vary significantly. Consult a healthcare professional for diagnosis and treatment.
West Nile virus, unfortunately, is a prevalent concern, especially during mosquito season. Understanding the virus’s lifecycle and transmission methods is crucial. Simultaneously, it’s important to consider the possibility of an MMR booster, especially given recent discussions around the need for additional protection against preventable diseases. Learning more about this possibility can help individuals make informed decisions about their health.
For a deeper dive into the potential for measles MMR boosters, check out this informative article: measles mmr booster possibility. Ultimately, staying informed about both West Nile virus and other potential health concerns is key to personal well-being.
Transmission and Prevention: Overview Of West Nile Virus

West Nile virus (WNV) poses a significant public health concern, primarily due to its transmission by mosquitoes. Understanding the intricate life cycle of these vectors and implementing effective preventive measures is crucial to minimizing the spread of this virus. Effective strategies encompass both personal protective measures and environmental modifications.Mosquitoes, the primary carriers of WNV, undergo a complex life cycle that involves several stages.
This intricate process is essential for understanding how the virus is transmitted and the effectiveness of different prevention strategies.
Mosquito Life Cycle and WNV Transmission
Mosquitoes undergo complete metamorphosis, transitioning through four distinct stages: egg, larva, pupa, and adult. The adult female mosquito is the key vector for WNV transmission. After feeding on a WNV-infected bird, the mosquito can transmit the virus to humans or other animals during its next blood meal. The virus replicates within the mosquito’s body, becoming infectious to its next host.
Different mosquito species have varying lifecycles, influenced by environmental factors like temperature and rainfall. Understanding these factors is essential for predicting and controlling mosquito populations and, consequently, WNV transmission.
Prevention Strategies, Overview of west nile virus
Effective WNV prevention relies on a multi-pronged approach targeting both mosquito populations and human exposure. These measures aim to disrupt the virus’s life cycle, preventing transmission from the mosquito to humans.
- Personal Protective Measures: Taking precautions to avoid mosquito bites is vital. This involves using insect repellents containing DEET, picaridin, or oil of lemon eucalyptus. Wearing long sleeves and pants, especially during dusk and dawn when mosquitoes are most active, can significantly reduce exposure. Eliminating standing water sources around homes and workplaces is critical in reducing mosquito breeding grounds.
So, I’ve been doing some digging on West Nile virus lately, and it’s fascinating how many different symptoms it can cause. One thing that’s been popping up in my research is how stress can sometimes manifest as skin reactions, like a rash on the face. If you’re curious about that, check out this article on stress rash on face.
While it’s important to be aware of these potential links, it’s still crucial to remember that a West Nile virus diagnosis is a complex medical issue and should always be confirmed by a doctor.
Proper use of window and door screens can prevent mosquitoes from entering homes.
- Environmental Control: Mosquito breeding sites, such as stagnant water in flowerpots, gutters, and discarded containers, are crucial targets for environmental control. Regularly emptying and cleaning these sites can significantly reduce mosquito populations. Properly maintained swimming pools and other water features can also minimize mosquito breeding. Working with local authorities and community programs to identify and eliminate mosquito breeding grounds in public spaces can be extremely effective.
Community-wide initiatives play a vital role in preventing WNV spread.
- Vaccine Development: While not a universally applied prevention strategy, vaccine development for WNV is an active area of research. Vaccines for animals, particularly birds, have demonstrated effectiveness in reducing the virus’s prevalence in wildlife populations. This indirectly affects human exposure as well.
Effectiveness Comparison
The effectiveness of different prevention strategies varies depending on the specific context. Personal protective measures are highly effective in reducing individual exposure, while environmental control is crucial for reducing overall mosquito populations. The combined use of both personal and environmental strategies provides the strongest protection against WNV transmission.
Human-to-Human Transmission
Human-to-human transmission of WNV is extremely rare. Transmission occurs primarily through the bite of an infected mosquito. While there have been isolated instances of possible transmission through blood transfusions or organ donations, the risk remains negligible compared to mosquito-borne transmission.
Environmental Factors
Environmental factors play a significant role in WNV transmission. Warmer temperatures and increased rainfall often correlate with increased mosquito activity and WNV transmission rates. Factors like climate change could potentially impact the geographic range of mosquitoes carrying the virus. Understanding the interplay between environmental factors and mosquito populations is essential for effective prevention strategies.
| Personal Protective Measure | Description |
|---|---|
| Insect Repellent Use | Apply repellent containing DEET, picaridin, or oil of lemon eucalyptus, following product instructions. |
| Protective Clothing | Wear long sleeves and pants, especially during dusk and dawn. |
| Eliminate Standing Water | Empty and clean containers that hold water regularly. |
| Screen Doors and Windows | Ensure screens are in good condition and prevent mosquito entry. |
Treatment and Management
Unfortunately, there’s no specific antiviral treatment currently available to cure West Nile virus (WNV) infection. Management focuses primarily on supportive care to alleviate symptoms and complications, allowing the body’s immune system to fight the infection. This approach is particularly crucial for individuals who develop severe complications.Effective management of WNV infection hinges on early recognition of symptoms, prompt medical intervention, and appropriate supportive care.
This includes providing hydration, pain relief, and respiratory support when necessary. The healthcare provider’s role is paramount in coordinating these efforts and monitoring the patient’s response to treatment.
Available Treatments
Current medical strategies primarily focus on alleviating symptoms and supporting the body’s natural defenses. No antiviral medications directly target the virus itself. Symptomatic relief remains a key component of the management plan.
Supportive Care
Providing supportive care is essential for individuals with WNV infection. This encompasses a range of interventions aimed at alleviating symptoms and complications. It includes measures like maintaining adequate hydration, administering pain relievers, and ensuring proper nutrition. These measures are critical to helping the body’s immune system combat the infection and recover. Monitoring vital signs and providing appropriate respiratory support are also important aspects of supportive care, particularly in severe cases.
Management of Severe Cases
Severe WNV infections can lead to neurological complications such as encephalitis or meningitis. In these cases, intensive care unit (ICU) admission may be necessary. Management in severe cases involves close monitoring of vital signs, aggressive fluid management, and respiratory support, as required. The severity of the infection and the specific complications dictate the intensity and scope of care.
Role of Healthcare Providers
Healthcare providers play a critical role in the treatment and management of WNV infection. Their responsibilities include accurately diagnosing the infection, initiating appropriate supportive care, and closely monitoring patients’ responses to treatment. Effective communication between healthcare providers, patients, and their families is essential for ensuring comprehensive and coordinated care. This involves detailed discussions about the infection, potential complications, and the treatment plan.
Comparison of Treatment Approaches
| Treatment Approach | Description | Effectiveness | Limitations |
|---|---|---|---|
| Symptomatic Relief | Focuses on managing symptoms like fever, headache, and body aches using over-the-counter medications and supportive care. | Effective for mild cases. | Does not eliminate the virus. |
| Supportive Care (Hydration, Nutrition, Respiratory Support) | Provides necessary fluids, nutrients, and respiratory assistance to maintain vital functions and support the immune system. | Essential for managing both mild and severe cases. | Effectiveness varies depending on the severity of the infection and the response of the immune system. |
| Intensive Care (Severe Cases) | ICU-level care, including close monitoring, aggressive fluid management, and mechanical ventilation, for individuals with severe neurological complications. | Critical for survival in severe cases. | May not be universally successful, and depends on the patient’s overall health. |
Public Health Impact
West Nile virus (WNV) outbreaks pose significant public health challenges, impacting communities in various ways. Understanding these implications is crucial for developing effective prevention and control strategies. The severity and scope of these impacts can vary depending on factors like geographic location, population density, and the specific strain of the virus circulating.The health and economic consequences of WNV outbreaks are multifaceted, demanding comprehensive public health responses.
These responses must consider the interplay between human health, the environment, and the overall economic well-being of affected populations. Effective strategies require a multi-pronged approach that integrates public awareness, environmental management, and robust healthcare infrastructure.
Public Health Implications of WNV Outbreaks
WNV outbreaks lead to increased morbidity and mortality rates, particularly in vulnerable populations. This translates to a strain on healthcare resources and a ripple effect across various sectors. The consequences are not solely medical but extend to social and economic spheres.
Impact on Healthcare Systems
WNV outbreaks place a substantial burden on healthcare systems. Hospitals and clinics face increased patient loads, requiring additional staffing, resources, and infrastructure. The need for specialized care for severe cases further complicates the situation. Diagnostic testing and treatment protocols also demand significant attention and investment. For example, during a large-scale outbreak, hospitals may experience delays in providing care for other conditions due to the surge in WNV patients.
Impact on Economic Stability
WNV outbreaks have considerable economic repercussions. Lost productivity due to illness or death of workers directly impacts businesses and the overall economy. Additionally, the cost of treatment, hospitalization, and public health interventions adds to the economic burden. For example, businesses may face reduced productivity and increased expenses related to employee absenteeism and healthcare costs associated with WNV-related illnesses.
Measures Taken by Public Health Organizations to Control WNV Outbreaks
Public health organizations employ various strategies to control WNV outbreaks. These include surveillance programs to track the virus’s spread, vector control measures to reduce mosquito populations, and public awareness campaigns to educate the community about prevention. These strategies are often tailored to the specific context of an outbreak, considering local environmental conditions and the characteristics of the affected population.
Role of Community Engagement in WNV Prevention
Community engagement plays a vital role in preventing WNV outbreaks. Public awareness campaigns, community outreach programs, and participation in vector control efforts are crucial for success. Effective communication and education empower individuals to take preventative measures, such as using mosquito repellent and eliminating mosquito breeding sites. Community involvement enhances the effectiveness of public health interventions, fostering a sense of shared responsibility in safeguarding public health.
Public Health Strategies for WNV Control
| Strategy | Description | Effectiveness |
|---|---|---|
| Surveillance | Monitoring mosquito populations, identifying infected individuals, and tracking the spread of the virus. | Essential for early detection and targeted interventions. |
| Vector Control | Eliminating mosquito breeding sites, using larvicides, and implementing mosquito abatement programs. | Proven effective in reducing mosquito populations and preventing transmission. |
| Public Awareness Campaigns | Educating the public about WNV, its symptoms, and preventative measures. | Crucial for empowering individuals to take preventative actions. |
| Early Diagnosis and Treatment | Identifying and treating infected individuals promptly to limit the severity of the illness and prevent further transmission. | Minimizes the severity of infection and hospitalizations. |
| Improved Healthcare Infrastructure | Ensuring sufficient healthcare resources to manage the influx of patients during outbreaks. | Crucial for effective management and response. |
Research and Future Directions
Unveiling the mysteries of West Nile Virus (WNV) requires a sustained commitment to research, encompassing various facets from understanding its intricate lifecycle to developing effective preventive measures and treatments. Ongoing studies are essential for anticipating future outbreaks, improving diagnostic accuracy, and ultimately safeguarding public health. This section delves into current research endeavors, potential future directions, and the crucial advancements in diagnostic techniques.
Current Research Efforts
Current research efforts surrounding WNV are multifaceted, encompassing investigations into the virus’s genetic makeup, its interaction with mosquito vectors, and the development of novel diagnostic tools. Researchers are also actively exploring strategies for preventing infection in susceptible populations and developing antiviral therapies. These endeavors are driven by the need to improve disease control and mitigate the devastating impact of WNV.
Potential Future Research Directions
Future research into WNV prevention and treatment should focus on developing more effective and accessible diagnostic tools, exploring novel antiviral therapies, and strengthening surveillance systems. The development of vaccines tailored to specific WNV strains is another promising area for future investigation. Further research into the complex interplay between WNV and its mosquito vectors could lead to innovative mosquito control strategies.
Research into the long-term effects of WNV infection on human health is also a crucial area to address.
Advancements in Diagnostic Methods
Significant advancements have been made in WNV diagnostic methods. These improvements include the development of rapid and sensitive diagnostic tests, enabling quicker identification and treatment of infected individuals. Molecular diagnostic techniques, such as polymerase chain reaction (PCR), have proven particularly valuable in detecting WNV in various biological samples. This increased diagnostic accuracy is crucial for timely intervention and preventing further transmission.
Challenges and Opportunities in WNV Research
Challenges in WNV research include the complex interactions between the virus, mosquito vectors, and the environment. Funding limitations can hinder progress, as well as the difficulty in conducting large-scale field studies. However, opportunities abound. Improved surveillance systems and enhanced collaboration among researchers and public health organizations offer a powerful approach to address these challenges. The development of novel diagnostic techniques and the discovery of new antiviral therapies are significant opportunities for future advancements.
Timeline of Key WNV Research Milestones
- 1999: Initial outbreak in the United States highlighted the need for WNV research.
- 2000s: Extensive research focused on understanding WNV transmission, identifying high-risk populations, and developing diagnostic tools.
- 2010s: Development of more rapid and accurate diagnostic methods, along with studies on the long-term health effects of WNV infection.
- Present: Continued research into antiviral therapies, vaccine development, and improved surveillance strategies.
Current Research Funding
| Funding Source | Estimated Funding (USD) | Year |
|---|---|---|
| National Institutes of Health (NIH) | Variable, but significant | 2020-2023 |
| Centers for Disease Control and Prevention (CDC) | Variable, but substantial | 2020-2023 |
| Other Governmental Agencies | Variable | 2020-2023 |
| Non-profit Organizations | Variable, but significant in some cases | 2020-2023 |
Note: Precise figures for funding are not consistently publicly available.
Illustrative Information
Understanding the intricacies of West Nile virus involves delving into its life cycle, the environments where mosquitoes thrive, the characteristics of the mosquito vector itself, and the precise mechanisms of transmission. This section provides a detailed exploration of these key elements.
West Nile Virus Lifecycle
The West Nile virus life cycle is a complex interplay between the virus, the mosquito vector, and the vertebrate host. The virus replicates within the mosquito, often with minimal effect on the insect’s health, yet with profound implications for human and animal health. Mosquitoes acquire the virus when they feed on infected birds. Once the virus replicates in the mosquito’s gut, it spreads to other tissues, including the salivary glands.
When the mosquito bites another vertebrate, it transmits the virus through its saliva. The virus then replicates within the vertebrate’s central nervous system or other tissues, depending on the host.
Mosquito Breeding Grounds
Mosquitoes require standing water for breeding. Identifying and eliminating these breeding grounds is a critical aspect of mosquito control and West Nile virus prevention. Common breeding sites include discarded containers, flower pots, clogged gutters, and even puddles in yards or parks. These seemingly insignificant sources of water can quickly become breeding grounds for vast numbers of mosquitoes.
Properly maintaining and cleaning these areas can significantly reduce the mosquito population. Emptying and cleaning containers regularly, maintaining proper drainage, and ensuring water does not stagnate in yards or parks are vital steps in reducing mosquito populations.
Mosquito Anatomical Features
The mosquito, as a vector, possesses specific anatomical features that facilitate its role in transmitting the virus. The mosquito’s proboscis, a long, slender mouthpart, is adapted for piercing skin and sucking blood. This proboscis is equipped with sensory structures that enable the mosquito to detect potential hosts. The mosquito’s ability to fly and its small size contribute to its widespread distribution and ease of movement.
These features allow the mosquito to efficiently locate and feed on vertebrate hosts, increasing the risk of transmitting pathogens.
Transmission Process
The West Nile virus transmission process involves a specific sequence of events. The mosquito acquires the virus when it feeds on an infected bird. The virus then replicates within the mosquito’s body, often without causing noticeable harm to the insect. When the mosquito feeds on a human or other vertebrate host, it injects its saliva, which may contain the virus.
The virus then enters the bloodstream and can replicate within the host, potentially causing illness. Understanding this transmission process is crucial for implementing effective preventative measures and control strategies.
Final Thoughts
In conclusion, West Nile virus poses a significant public health concern. Understanding its transmission, symptoms, and prevention strategies is crucial for mitigating its impact. The ongoing research and public health initiatives play a vital role in controlling the spread and improving outcomes for those affected. By working together, we can improve our understanding and response to this mosquito-borne illness.




