Oral bacteria colorectal cancer risk is a burgeoning area of research, exploring the unexpected link between bacteria in your mouth and the development of colorectal cancer. This connection suggests a potential pathway for disease development, potentially affecting how we understand and treat this serious illness. While the research is still evolving, early findings suggest a surprising role for oral microbes in this process.
This article delves into the potential mechanisms behind this association, exploring the types of oral bacteria involved, their metabolic activities, and the possible pathways connecting them to colorectal cancer. We’ll also examine the limitations of current research and discuss the exciting implications for future investigations.
Introduction to Oral Bacteria and Colorectal Cancer Risk
The connection between oral bacteria and colorectal cancer risk is a fascinating and rapidly evolving area of research. While the precise mechanisms are still being investigated, accumulating evidence suggests a potential link. This blog post delves into the current understanding of this association, exploring the potential pathways and the limitations of the existing research.The idea that oral bacteria could play a role in colorectal cancer development might seem surprising at first.
However, the human gut, and the microbiome within, is a complex ecosystem interacting with various parts of the body, including the mouth. The transfer of oral bacteria to the gut, and their potential impact on gut health, is now being actively explored.
Potential Mechanisms of Oral Bacteria Involvement
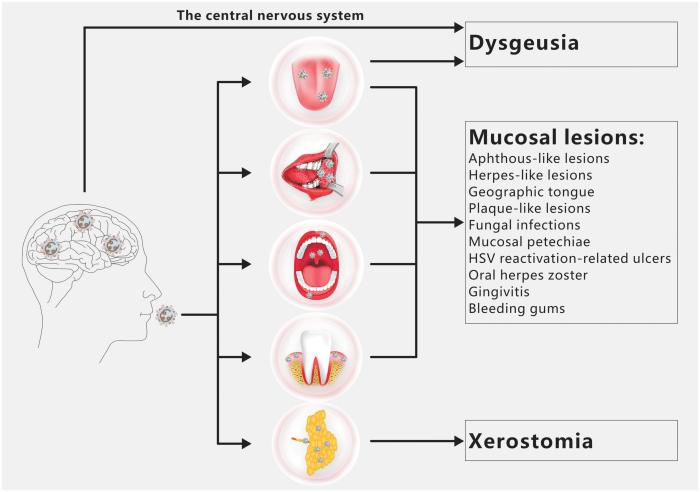
A growing body of evidence suggests that certain oral bacteria can potentially influence the development of colorectal cancer. This influence likely occurs through a complex interplay of mechanisms, including chronic inflammation, immune response modulation, and metabolic changes within the gut. For example, some oral bacteria can produce metabolites that might contribute to inflammation and cellular damage in the colon.
Historical Context of Research
Early studies focused primarily on the link between oral health and general health, often overlooking the possibility of oral bacteria impacting distant sites like the colon. The rise of advanced genomic sequencing and microbiome research has enabled more detailed investigation of the oral microbiome’s role in disease. The increasing sophistication of these tools has led to a more nuanced understanding of the interaction between oral bacteria and the gut.
Recent research suggests a fascinating link between oral bacteria and colorectal cancer risk. It’s a complex area, but some studies indicate that certain oral bacteria may play a role in the development of the disease. While exploring different asthma treatments like Flovent, Qvar, Pulmicort, Alvesco, or Asmanex, this guide might be helpful for understanding these options, the connection between oral bacteria and colorectal cancer risk remains a significant area of ongoing research.
More research is needed to fully understand this connection and potential preventative measures.
Potential Pathways Connecting Oral Bacteria to Colorectal Cancer
The specific pathways connecting oral bacteria to colorectal cancer are still being elucidated. However, several potential routes have been identified.
- Translocation: Oral bacteria can potentially be transported to the colon, where they may interact with the gut microbiota and contribute to an inflammatory environment. For example, during instances of compromised gut barrier function, bacteria may enter the colon more easily, leading to an inflammatory response.
- Metabolic Interactions: Some oral bacteria produce metabolites that can potentially influence the growth and development of colorectal cancer cells. For instance, certain metabolites may alter the gut environment, providing a more hospitable environment for cancerous cells to thrive.
- Immune System Modulation: Oral bacteria can potentially affect the immune response in the colon. Chronic inflammation associated with these bacteria may lead to an altered immune response, which in turn may contribute to the development of colorectal cancer. A weakening of the immune system’s ability to combat abnormal cells could potentially increase the likelihood of cancerous growth.
Limitations of Current Research
While promising, the research on oral bacteria and colorectal cancer is still in its early stages. Significant limitations remain.
- Causation vs. Correlation: Many studies have shown correlations between specific oral bacteria and colorectal cancer risk, but definitively proving causation remains a challenge. Further research is needed to establish a causal link.
- Complexity of the Gut Microbiome: The human gut microbiome is incredibly complex, with numerous bacterial species interacting with each other. Identifying specific oral bacteria directly responsible for colorectal cancer development is a complex task, and many other factors might be at play.
- Variability in Study Designs: The diverse methodologies used in different studies can make it challenging to compare results and draw definitive conclusions. The lack of standardized methodologies makes it difficult to assess the reliability and generalizability of findings.
Types of Oral Bacteria and Their Potential Roles
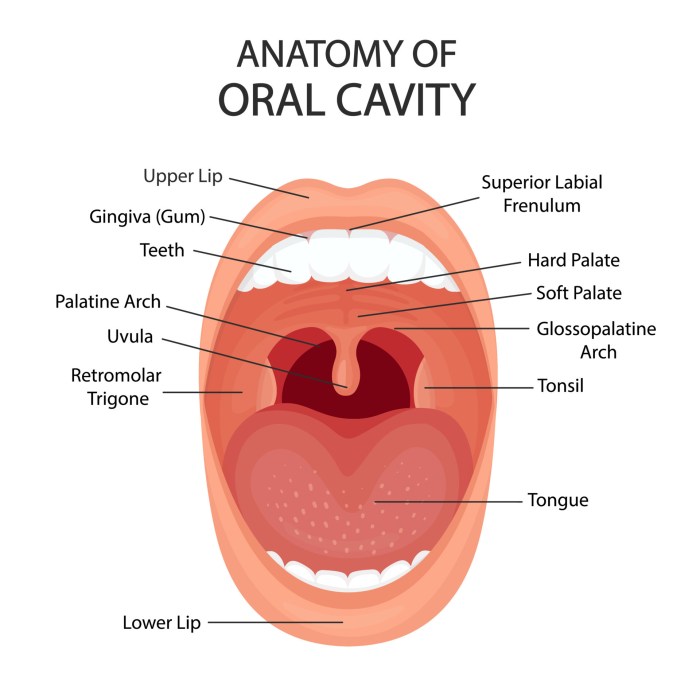
The human mouth is teeming with a diverse microbial community, a complex ecosystem of bacteria, fungi, and viruses. While many of these microorganisms are harmless or even beneficial, some have been linked to an increased risk of colorectal cancer (CRC). This section delves into the specific types of oral bacteria implicated in CRC, examining their potential roles in the disease process and the mechanisms through which they might exert their influence.
Major Types of Oral Bacteria Implicated in CRC Risk
Numerous oral bacterial species have been identified as potentially contributing factors to colorectal cancer. These bacteria, residing in the complex oral microbiome, can influence various aspects of the body, including the gut, potentially playing a role in CRC development. Key players include those belonging to the
- Fusobacterium*,
- Porphyromonas*,
- Tannerella*, and
- Prevotella* genera, amongst others.
Potential Roles of Different Oral Bacterial Species, Oral bacteria colorectal cancer risk
The potential roles of these oral bacterial species in CRC development are multifaceted and not fully understood. Some bacteria may directly interact with the intestinal lining, inducing inflammation and damaging the cellular structures of the colon. Others may produce toxins or metabolites that promote cancer development or suppress immune responses, potentially contributing to the progression of the disease. The precise mechanisms through which different bacterial species exert their effects are still being actively researched.
Recent studies show a surprising link between oral bacteria and colorectal cancer risk. It’s a complex area, but it’s thought that these bacteria might travel through the bloodstream and affect distant tissues. While a broken toe, for example, what is a broken toe is a localized issue, these oral bacteria could potentially contribute to more serious systemic health concerns.
Further research is needed to fully understand this connection, but it highlights the importance of maintaining good oral hygiene.
Specific Metabolic Activities of Oral Bacteria
The metabolic activities of oral bacteria are crucial in determining their potential role in CRC. For example,Fusobacterium nucleatum*, a prominent bacterium linked to CRC, produces metabolites like short-chain fatty acids (SCFAs), but also other molecules that could contribute to inflammation and cell damage. These metabolites can directly or indirectly influence the intestinal environment, potentially promoting the growth of cancerous cells.
Furthermore, some bacteria can alter the gut microbiome composition, influencing the balance between beneficial and harmful bacteria.
Mechanisms of Oral Bacteria-Induced Colorectal Cancer
Several possible mechanisms exist through which oral bacteria might contribute to colorectal cancer development. One prominent pathway involves the production of inflammatory molecules by these bacteria. This inflammation can damage the colon lining, creating an environment conducive to the initiation and progression of cancer. Another mechanism is the disruption of the normal gut microbiome, leading to an imbalance in the microbial community and an increased susceptibility to cancerous growth.
Additionally, bacterial products can potentially promote DNA damage and cellular transformation, directly affecting the genetic stability of colon cells.
Recent studies are showing a surprising link between oral bacteria and colorectal cancer risk. It’s a fascinating area of research, but it’s also important to remember that other factors play a role. For example, muscle and joint pain with thyroid disease muscle and joint pain with thyroid disease can be a significant health concern, but it’s not directly connected to oral bacteria impacting colorectal cancer.
Ultimately, maintaining good oral hygiene likely contributes to overall health and reducing the risk of various diseases, including colorectal cancer.
Table: Oral Bacteria, Potential Roles, and Relevant Research
| Bacteria Type | Potential Role | Research Findings |
|---|---|---|
| *Fusobacterium nucleatum* | Promotes inflammation, DNA damage, and disruption of the gut microbiome. | Numerous studies have shown a strong correlation between
|
| *Porphyromonas gingivalis* | Contributes to chronic inflammation, potentially increasing the risk of colorectal cancer. | Research suggests a link betweenP. gingivalis* and CRC development, possibly through the production of toxins and inflammatory mediators. |
| *Tannerella forsythia* | May promote inflammation and disrupt the gut microbiome balance. | Studies have explored the presence ofT. forsythia* in CRC tissue and its potential role in colorectal carcinogenesis. Further research is needed to fully elucidate its effects. |
| *Prevotella intermedia* | Potentially implicated in inflammation and altered gut microbiome composition. | Studies have observed an association betweenP. intermedia* and colorectal cancer. More investigation is necessary to confirm the causal link. |
Mechanisms of Action: Oral Bacteria Colorectal Cancer Risk
The journey from oral bacteria to colorectal cancer is a complex one, involving multiple steps and interactions within the body. While the exact mechanisms are still being investigated, mounting evidence suggests a crucial role for these bacteria in the development of this disease. This section delves into the ways oral bacteria might contribute to colorectal cancer, exploring the inflammatory response, bacterial metabolites, and their interplay with the gut microbiome.
Inflammation and the Immune Response
Oral bacteria can trigger an inflammatory response in the gut, even if they don’t directly colonize the colon. This inflammatory reaction can lead to chronic inflammation, a significant risk factor for colorectal cancer. Chronic inflammation creates a cellular environment that is conducive to DNA damage and uncontrolled cell growth. The immune system, attempting to control this response, can also play a part in the disease progression.
Dysregulation of the immune system, leading to a chronic inflammatory state, is a key factor in many cancers.
Bacterial Metabolites and Toxins
Certain oral bacteria produce metabolites and toxins that can damage the colon lining. These substances can cause DNA damage, increase cell proliferation, and disrupt the normal cellular processes that regulate growth and repair. For instance, some bacteria produce genotoxins, which directly interact with DNA, increasing the risk of mutations that can lead to cancer. Furthermore, certain bacterial metabolites can alter the gut environment, making it more susceptible to the harmful effects of other factors.
Interaction with the Gut Microbiome
Oral bacteria may influence the gut microbiome’s composition and function. The gut microbiome plays a critical role in digestion, immune regulation, and overall health. An imbalance in this microbiome, known as dysbiosis, can increase the risk of various diseases, including colorectal cancer. Oral bacteria may contribute to dysbiosis by altering the balance of beneficial and harmful bacteria in the gut, creating an environment conducive to the growth of cancer-promoting bacteria.
A healthy microbiome can be viewed as a vital first line of defense against various health issues.
Comparison of Mechanisms
| Bacteria Type | Mechanism | Impact on Gut |
|---|---|---|
| Porphyromonas gingivalis | Produces genotoxins, leading to DNA damage and inflammation. May also alter the gut microbiome’s composition by stimulating inflammatory responses. | Increased inflammation, potentially promoting dysbiosis, and creating a potentially cancerous environment. |
| Fusobacterium nucleatum | Associated with increased colorectal cancer risk. May promote inflammation and activate oncogenic pathways. Evidence suggests it may disrupt normal gut homeostasis. | Increased inflammation, potentially contributing to dysbiosis, and creating a potentially cancerous environment. |
| Aggregatibacter actinomycetemcomitans | May contribute to inflammation and potentially influence the gut microbiome. | Increased inflammation, potentially promoting dysbiosis, and potentially creating a potentially cancerous environment. |
Final Conclusion
In conclusion, the link between oral bacteria and colorectal cancer risk presents a compelling area of investigation. The intricate interplay between oral microbes and the gut microbiome, along with potential inflammatory responses and bacterial metabolites, deserves further exploration. While more research is needed, this connection highlights a potential avenue for early detection and prevention strategies. Future studies are crucial to fully understand the complexities of this relationship and translate these findings into practical applications.




