Nerve damage after plastic surgery is a serious concern that requires careful consideration. This comprehensive guide explores the various types of nerve damage, potential risk factors, diagnostic methods, treatment options, preventive strategies, and the lasting effects on patients. Understanding these factors is crucial for both patients and medical professionals.
Different plastic surgery procedures carry varying degrees of nerve injury risk. Factors like surgical technique, patient anatomy, and pre-operative assessments play significant roles in determining the likelihood of nerve damage. This article will delve into the complexities of each aspect, providing valuable insights for informed decision-making.
Types of Nerve Damage
Post-plastic surgery, nerve damage can manifest in various forms, impacting the patient’s recovery and well-being. Understanding these different types of damage is crucial for both patients and healthcare professionals to effectively manage the potential complications. This section delves into the specifics of peripheral neuropathy, nerve entrapment, and nerve laceration, highlighting their differences and potential symptoms.
Dealing with nerve damage after plastic surgery can be a real drag, but sometimes you just need a break from your monthly cycle. Fortunately, there are methods like using the Ortho Evra patch to skip your period, how to skip your period using the ortho evra patch. While these options can offer temporary relief, it’s crucial to remember that nerve damage recovery is a longer-term process and requires careful medical attention.
It’s all about finding what works best for your body and healing journey.
Peripheral Neuropathy
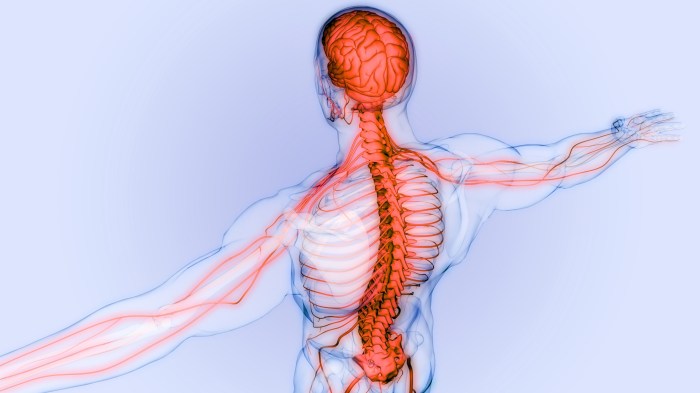
Peripheral neuropathy is a broad term encompassing damage to the peripheral nerves, which branch out from the spinal cord and brain to the rest of the body. This damage often results in a range of sensory, motor, and autonomic symptoms. The specific symptoms depend on the location and extent of the nerve damage, as well as the type of nerve affected.
Common symptoms include numbness, tingling, pain, and weakness in the affected areas. These sensations can range from mild discomfort to debilitating pain. Severity varies widely depending on the underlying cause.
Nerve Entrapment
Nerve entrapment occurs when a nerve is compressed or squeezed by surrounding tissues, such as muscles, tendons, or ligaments. This compression can be caused by a variety of factors, including scar tissue formation from the surgical procedure or pre-existing anatomical conditions. The symptoms of nerve entrapment can be similar to those of peripheral neuropathy, including pain, numbness, and tingling.
However, nerve entrapment often presents with a specific pattern of symptoms that correlate with the location of the affected nerve. For example, carpal tunnel syndrome, a common type of nerve entrapment, is characterized by pain and numbness in the hand and wrist.
Nerve Laceration
Nerve laceration involves a complete or partial tear of a nerve. This can occur during the surgical procedure itself, or as a consequence of trauma or injury in the healing phase. The symptoms of nerve laceration depend on the severity of the injury and the specific nerve affected. In some cases, a complete laceration may lead to permanent loss of function in the affected area.
Pain, altered sensation, and muscle weakness are common symptoms, potentially resulting in a loss of motor control.
Comparison of Symptoms
| Type of Nerve Damage | Symptoms | Location |
|---|---|---|
| Peripheral Neuropathy | Numbness, tingling, pain, weakness, decreased sensation | Can affect various parts of the body |
| Nerve Entrapment | Pain, numbness, tingling, weakness, sometimes specific to the affected nerve | Usually localized to a specific area, depending on the nerve |
| Nerve Laceration | Complete loss of function in the affected area, pain, altered sensation, muscle weakness | Specific to the location of the damaged nerve |
Potential Locations of Nerve Damage After Plastic Surgery
| Surgery Type | Potential Nerve Locations | Symptoms |
|---|---|---|
| Facelift | Facial nerves (e.g., facial nerve, supraorbital nerve), nerves around the temples and jaw | Facial asymmetry, numbness, tingling, difficulty with facial expressions |
| Breast Augmentation/Reduction | Nerves around the breast tissue, pectoral nerves | Numbness, tingling, pain in the breast, chest wall, or arm |
| Rhinoplasty | Nerves around the nose and upper lip | Numbness, tingling, or pain around the nose, upper lip, or forehead |
| Liposuction | Nerves in the treated areas (e.g., abdomen, thighs, arms) | Numbness, tingling, pain, weakness in the treated areas |
| Abdominoplasty | Nerves around the abdomen, groin, and lower back | Numbness, tingling, pain, weakness in the abdomen, groin, or lower back |
Risk Factors
Understanding the potential for nerve damage after plastic surgery requires a multifaceted approach. While the artistry of plastic surgery aims to enhance beauty and well-being, the delicate nature of nerves necessitates careful consideration of various factors that can increase the risk of complications. This section will delve into these risk factors, emphasizing the importance of pre-operative assessment and the impact of surgical technique on nerve integrity.
Surgical Technique
Surgical technique plays a crucial role in minimizing the risk of nerve damage. Precise and meticulous dissection, avoiding unnecessary stretching or manipulation of nerves, is paramount. Experienced surgeons with a deep understanding of regional anatomy and a commitment to minimally invasive techniques are key to minimizing risk. Careful attention to tissue handling, using appropriate instruments and techniques to prevent trauma, is essential.
The surgeon’s skill and experience directly influence the likelihood of nerve injury. For example, a surgeon proficient in microvascular techniques is better equipped to handle delicate nerves in procedures like facelifts or rhinoplasties.
Patient Anatomy
Individual variations in patient anatomy significantly impact the susceptibility to nerve damage. Nerves can be situated in close proximity to the surgical field, making them vulnerable to accidental injury. The precise location and path of nerves vary from person to person, and variations in facial structure, muscle placement, and underlying anatomy can influence the risk of nerve injury during procedures.
The surgeon must carefully consider these anatomical nuances to anticipate potential risks and plan the procedure accordingly. For instance, a patient with a particularly prominent facial nerve may require a more cautious approach to avoid iatrogenic damage.
Ugh, nerve damage after plastic surgery is a real bummer. It’s often tricky to pinpoint the cause, but sometimes it can be related to complications during the procedure. Knowing if you have certain antibodies, like those measured in a ccp antibody test, can be helpful in understanding potential underlying conditions. For instance, checking out the ccp antibody test uses side effects procedure results could offer some insights.
Ultimately, a proper diagnosis and treatment plan are crucial for recovery from nerve damage, no matter the cause.
Individual Predisposition, Nerve damage after plastic surgery
Individual predisposition to nerve injury is a complex factor encompassing various elements. Underlying conditions like diabetes, poor circulation, and compromised immune systems can affect nerve healing and resilience to trauma. Furthermore, patients with a history of nerve-related issues or conditions that compromise tissue healing are inherently more vulnerable. Patients with a family history of nerve-related problems may also be at increased risk.
Pre-operative medical evaluations can help identify patients with such vulnerabilities, allowing for appropriate precautions and adjustments to the surgical plan. For example, a patient with known peripheral neuropathy might necessitate a more conservative approach to minimize any potential aggravation of their existing condition.
Pre-operative Assessments
Thorough pre-operative assessments are crucial in identifying patients at higher risk of nerve damage. A detailed medical history, including any past nerve injuries or conditions, is essential. Physiological parameters, like blood sugar levels, blood flow, and overall health, should be evaluated to assess a patient’s capacity for healing. Physical examination and diagnostic imaging, such as nerve conduction studies, can help pinpoint the precise location and course of nerves, enabling the surgeon to plan the procedure more accurately.
A thorough understanding of the patient’s individual anatomy and medical history allows the surgeon to tailor the surgical approach to minimize risk. For example, pre-operative nerve conduction studies in a patient undergoing a facelift can help identify nerves at higher risk of injury, allowing the surgeon to avoid these areas during dissection.
Comparison of Surgical Techniques and Nerve Injury Risks
| Surgical Technique | Nerve Injury Risk | Explanation |
|---|---|---|
| Traditional Facelift | Moderate | The dissection can involve manipulating nerves in close proximity, potentially leading to damage. |
| Minimally Invasive Facelift | Lower | Smaller incisions and less extensive dissection reduce the risk of nerve damage. |
| Rhinoplasty | Low | The focus is on structural manipulation, with nerves typically less exposed. |
| Breast Augmentation | Low | Nerve damage is usually a result of improper positioning of implants, not direct manipulation of nerves. |
| Liposuction | Very Low | Nerve damage is uncommon unless excessive pressure is applied. |
Symptoms and Diagnosis
Post-surgical nerve damage can manifest in various ways, impacting patients’ quality of life. Understanding the symptoms and the diagnostic methods available is crucial for prompt intervention and effective treatment. Early detection and accurate diagnosis allow for timely management, potentially minimizing long-term complications.
Common Symptoms of Nerve Damage
Nerve damage after plastic surgery can present with a range of symptoms, varying in intensity and location depending on the specific nerve affected. These symptoms can often be subtle initially, making it challenging to recognize them as related to the surgery. It’s important to be aware of these signs and report them to your physician immediately.
- Pain: Pain can manifest as sharp, shooting, or dull aches, often described as burning or tingling. The location and intensity of the pain can vary significantly depending on the affected nerve. For example, facial nerve damage might cause persistent pain around the mouth or eye area, while brachial plexus damage could lead to pain radiating down the arm.
- Numbness: Numbness is characterized by a lack of sensation in the affected area. This can range from a mild prickling feeling to a complete absence of touch perception. For instance, if a nerve in the hand is damaged, the patient might experience numbness in the fingers or palm.
- Tingling: Tingling sensations, often described as pins and needles, are another common symptom. These sensations are usually intermittent and can be localized or spread across a larger area. An example might be a tingling sensation in the foot after a leg lift surgery.
- Weakness: Weakness in the affected area is a significant indicator of nerve damage. This weakness can range from a subtle decrease in strength to a complete inability to use the affected limb or muscle group. For example, weakness in the hand after hand surgery might make it difficult to grip objects.
Diagnostic Methods
Accurate diagnosis of nerve damage is essential for effective treatment. Several methods are used to evaluate nerve function and pinpoint the affected area.
- Physical Examination: A thorough physical examination is the first step in the diagnostic process. This involves assessing the patient’s range of motion, muscle strength, and sensory function in the affected area. A physical exam can reveal subtle signs of nerve damage, which may not be apparent through other methods.
- Nerve Conduction Studies (NCS): NCS measure the speed and strength of electrical signals traveling along nerves. These studies help determine if the nerve is functioning correctly and identify any areas of damage or slowing in signal transmission. A typical scenario might involve testing the nerve responsible for sensation in the arm to identify if signals are slowed down.
- Electromyography (EMG): EMG evaluates the electrical activity of muscles. This procedure helps identify if the nerves controlling the muscles are sending appropriate signals. It is often used in conjunction with NCS to confirm the presence and location of nerve damage. For example, in cases of facial paralysis, EMG can help determine the extent of nerve damage and the appropriate course of treatment.
Symptom Correlation with Affected Nerve
The following table illustrates possible correlations between common symptoms and the nerves that might be affected. It is crucial to remember that this table is not exhaustive and individual cases can vary.
| Symptom | Possible Affected Nerve | Description |
|---|---|---|
| Pain in the forearm | Radial nerve | Pain radiating down the forearm, often described as sharp or burning. |
| Numbness in the thumb and index finger | Median nerve | Loss of sensation in the thumb, index, middle, and part of the ring fingers. |
| Weakness in the hand muscles | Ulnar nerve | Difficulty gripping objects or performing fine motor tasks. |
| Tingling in the fingers | Multiple nerves (e.g., median, ulnar) | Intermittent or constant tingling sensations in the fingers. |
| Facial weakness or paralysis | Facial nerve | Inability to control facial muscles, leading to drooping or asymmetry. |
Management and Treatment
Nerve damage after plastic surgery, though often temporary, can significantly impact a patient’s recovery. Effective management and treatment are crucial for restoring function and minimizing long-term complications. The approach depends heavily on the severity and location of the injury, as well as the individual patient’s response to treatment. Early intervention is key to maximizing outcomes.Addressing nerve damage necessitates a multi-faceted strategy, encompassing medication, physical therapy, and potentially, surgical interventions.
The choice of treatment will be tailored to the specific circumstances of each patient, considering factors like the type of nerve damage, its location, and the patient’s overall health. Each approach has its own advantages and disadvantages, and the optimal strategy often involves a combination of these methods.
Medication Management
Pharmacological interventions play a supporting role in managing nerve damage. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate discomfort. In some cases, corticosteroids may be used to reduce inflammation around the affected nerve. However, their use should be carefully considered due to potential side effects, such as increased risk of infection or other complications.
The efficacy of these medications varies greatly depending on the severity of the nerve damage. In some instances, they may not offer significant relief, and a more aggressive approach might be necessary.
Physical Therapy
Physical therapy is often a crucial component of nerve damage treatment after plastic surgery. It aims to restore the lost function and prevent the development of secondary complications, such as muscle atrophy or contractures. Therapeutic exercises, including range-of-motion exercises, strengthening exercises, and nerve gliding exercises, are tailored to the specific needs of each patient. The goal is to encourage the regeneration of nerve fibers and improve the re-establishment of neural pathways.
Hey everyone! Plastic surgery can sometimes lead to nerve damage, a pretty serious complication. It’s important to be aware of potential risks. While nerve damage is a distinct issue, it’s interesting to consider the parallels to viral infections like mononucleosis. Have you ever wondered if you could get mono twice? This resource dives deep into that question, and understanding immune responses to viruses might shed light on some recovery processes after surgery, too.
Ultimately, nerve damage after plastic surgery requires careful monitoring and appropriate medical care, so it’s crucial to prioritize your health.
Successful outcomes in physical therapy depend on consistent patient participation and adherence to prescribed regimens. Individualized programs are critical for maximizing benefits.
Surgical Interventions
Surgical intervention might be necessary in cases of severe nerve damage or when other treatments fail to provide adequate relief. This could involve nerve repair or grafting procedures to reconnect severed nerve fibers. Surgical options are typically reserved for more complex situations, and the decision to perform surgery must be carefully evaluated. Surgical interventions are not without risks, including the possibility of infection, scarring, or further nerve damage.
The potential benefits of surgery must be weighed against these risks. Recovery timelines after surgical interventions can be significantly longer compared to other treatments.
Treatment Modalities Comparison
| Treatment | Effectiveness | Side Effects | Recovery Time |
|---|---|---|---|
| Medication (NSAIDs, Corticosteroids) | Moderate, often helpful for pain and inflammation | Potential for gastrointestinal issues, increased risk of infection (with corticosteroids) | Variable, generally shorter than other treatments |
| Physical Therapy | High, particularly for restoring function and preventing complications | Minimal, but potential for discomfort during exercises | Variable, depending on the severity of the damage and patient adherence |
| Surgical Intervention | High in severe cases, but with potential risks | Infection, scarring, further nerve damage, prolonged recovery | Significantly longer, potentially months or even years |
Prevention Strategies: Nerve Damage After Plastic Surgery
Minimizing the risk of nerve damage during plastic surgery is paramount. A meticulous approach encompassing careful patient selection, precise surgical technique, and proactive intraoperative monitoring is crucial for achieving optimal outcomes. Understanding the potential risks and implementing preventative measures can significantly reduce the likelihood of complications.Surgical precision and a deep understanding of the delicate nerve pathways in the targeted area are essential for minimizing nerve injury.
This requires extensive pre-operative planning, practiced surgical skills, and continuous vigilance during the procedure. A proactive approach, focusing on preventative measures, is vital to protecting patient well-being and achieving favorable surgical results.
Meticulous Surgical Technique
Surgical precision is paramount in minimizing nerve damage. Experienced surgeons with a thorough understanding of the anatomy of the surgical area, coupled with precise surgical instruments and techniques, significantly reduce the likelihood of nerve trauma. Maintaining meticulous attention to detail, employing proper surgical instruments, and utilizing appropriate surgical techniques are vital for protecting nerve integrity. For example, employing meticulous dissection techniques around delicate nerve structures, such as the facial nerve in facelift procedures, is crucial to prevent inadvertent injury.
Using magnified visualization and specialized instruments for delicate tissue handling further enhance precision.
Careful Patient Selection
Preoperative evaluation is essential for identifying patients at higher risk of nerve damage. Factors such as pre-existing nerve conditions, medical history, and patient expectations play a significant role in patient selection. Understanding a patient’s medical history, including any prior nerve injuries or neurological conditions, is critical. Careful assessment of the patient’s expectations and realistic understanding of the procedure’s potential outcomes is also vital.
This includes a thorough discussion of potential risks, benefits, and alternatives, empowering the patient to make informed decisions.
Pre-operative Planning and Intraoperative Monitoring
Thorough pre-operative planning and meticulous intraoperative monitoring are critical components of minimizing nerve damage. A detailed pre-operative assessment, including detailed imaging studies (e.g., CT scans, MRIs), and a thorough understanding of the patient’s anatomy, helps surgeons prepare for the procedure. Real-time monitoring techniques, like electromyography (EMG) and nerve monitoring, are often employed during the surgery to provide immediate feedback on nerve function.
This allows the surgeon to adjust their technique and ensure nerve integrity throughout the procedure. For example, during a breast augmentation, real-time nerve monitoring can alert the surgeon to potential nerve compression, enabling immediate adjustments to prevent injury.
Nerve-Sparing Techniques
Nerve-sparing techniques are increasingly utilized in plastic surgery to preserve the integrity of surrounding nerves. Minimizing surgical incisions and carefully dissecting around nerve structures, and employing specialized instruments to protect nerves, are examples of these techniques. These strategies aim to preserve the natural function and health of the nerves, potentially reducing the risk of long-term complications. Using micro-instruments and precise dissection techniques helps preserve nerves, preserving the patient’s natural function and appearance.
Preventative Measures for Minimizing Nerve Damage
- Thorough pre-operative evaluation, including detailed medical history, imaging studies, and patient counseling, is crucial.
- Employing meticulous surgical techniques, precise instruments, and magnified visualization, especially around critical nerve structures.
- Utilizing intraoperative nerve monitoring (e.g., electromyography, sensory evoked potentials) to detect and avoid nerve injury.
- Implementing nerve-sparing techniques, such as meticulous dissection and appropriate instrument selection, to minimize the risk of damage.
- Maintaining a high standard of surgical expertise and experience to ensure the surgeon is proficient in handling delicate nerve tissues.
- Clear communication between the surgeon and the patient, outlining potential risks and benefits of the procedure.
- Close postoperative monitoring for any signs of nerve dysfunction.
Long-Term Effects
The journey of recovery from nerve damage after plastic surgery is multifaceted and often extends beyond the initial healing period. Long-term effects can significantly impact a patient’s functional abilities and overall quality of life. Understanding these potential consequences is crucial for both patients and surgeons to proactively manage expectations and ensure optimal outcomes.Long-term nerve damage can manifest in various ways, ranging from subtle changes in sensation to debilitating functional limitations.
Factors influencing the severity and nature of these effects are numerous, and consistent follow-up care is essential to monitor and address potential complications. This section will explore the potential long-term effects, the impact on quality of life, influential factors, and the importance of ongoing support for patients.
Impact on Functional Abilities
Post-surgical nerve damage can lead to a spectrum of functional limitations. These limitations can affect daily tasks, social interactions, and overall well-being. For instance, loss of sensation in a hand or face can make tasks like eating, writing, or even simple grooming challenging. Similarly, muscle weakness or paralysis can impede mobility and independence.
Impact on Quality of Life
The impact of nerve damage on quality of life is profound. It can affect self-esteem, social interactions, and emotional well-being. Chronic pain, altered sensation, and limitations in movement can lead to feelings of frustration, isolation, and depression. These psychosocial factors are equally important to consider in the long-term management of nerve damage.
Factors Influencing Long-Term Outcome
Several factors can influence the long-term outcome of nerve damage. These include the severity of the initial injury, the location of the damaged nerve, the type of surgical procedure, and the individual’s response to treatment. Further, adherence to rehabilitation protocols, lifestyle factors, and the presence of pre-existing medical conditions can also play a role.
Importance of Long-Term Follow-Up Care
Regular follow-up appointments with a plastic surgeon and other relevant healthcare professionals are crucial. These appointments allow for ongoing monitoring of nerve function, early detection of complications, and adjustments to treatment plans as needed. Early intervention can often mitigate the severity of long-term issues and improve the patient’s overall outcome.
Case Study: Chronic Pain Following Rhinoplasty
A 30-year-old patient underwent rhinoplasty to correct a deviated nasal septum. Post-operatively, she experienced persistent numbness and tingling in the tip of her nose and surrounding area. The surgeon diagnosed a minor nerve impingement during the procedure. While initial symptoms improved with time, the patient experienced chronic pain in the same area. She required ongoing pain management and follow-up consultations with a neurologist to manage the persistent discomfort.
This case highlights the importance of recognizing subtle signs of nerve damage and providing appropriate long-term management strategies.
Last Word
In conclusion, nerve damage following plastic surgery is a multifaceted issue with significant implications for patient well-being. Understanding the potential risks, symptoms, and treatment options is essential for both patients and healthcare providers. By prioritizing meticulous surgical techniques, comprehensive pre-operative assessments, and robust post-operative care, the likelihood of nerve damage can be minimized. Ongoing research and advancements in surgical techniques will further refine our ability to prevent and treat this challenging complication.