Medication for treating migraine is a crucial aspect of managing this debilitating condition. This guide delves into various medication types, their effectiveness, potential side effects, and patient considerations. We’ll explore everything from over-the-counter options to preventive strategies and emerging treatments, equipping you with the knowledge to make informed decisions about your migraine management.
Understanding the different types of migraine medications, their mechanisms of action, and available forms is essential. This includes a detailed look at oral, injectable, and nasal spray options, helping you to understand which might be most suitable for your needs. We’ll also discuss the effectiveness of various medications in treating different migraine subtypes and their potential side effects.
Types of Migraine Medications
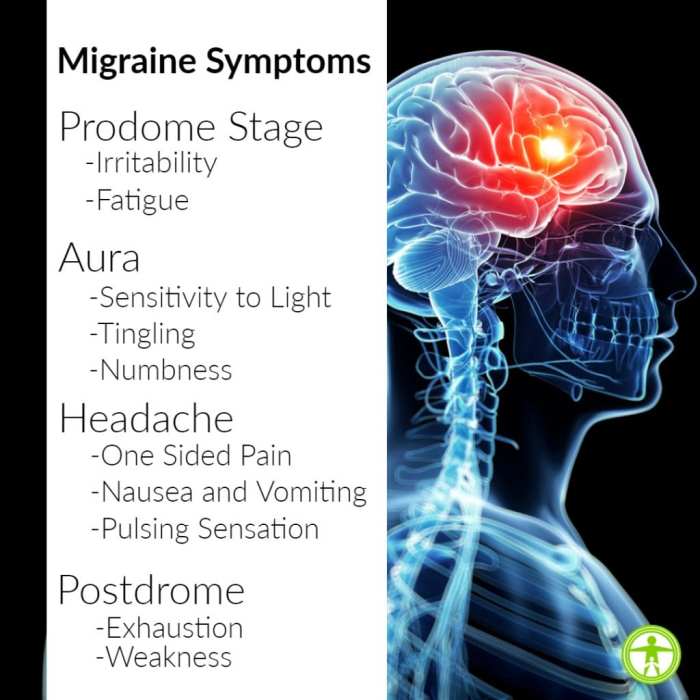
Migraines, debilitating headaches, can be effectively managed with various medications targeting different stages of the headache cycle. Understanding the different classes of drugs and their mechanisms of action can help patients and healthcare providers make informed decisions about treatment options. This section details the types of migraine medications available and their characteristics.
Finding the right medication for migraines can be a real challenge, and sometimes it takes trial and error. But, understanding your triggers is key. For example, similar to pinpointing migraine triggers, you can use ask an expert tools to track psoriasis triggers to help identify what might be causing flare-ups. This kind of detailed self-assessment can ultimately help you manage your migraine symptoms more effectively.
It’s all about connecting the dots to find relief.
Medication Classes and Mechanisms of Action
Different types of migraine medications work through various mechanisms, affecting pain pathways and inflammation in the brain. Choosing the right medication depends on individual responses and the characteristics of the migraine.
| Medication Class | Mechanism of Action | Available Forms |
|---|---|---|
| Triptans | These medications, such as sumatriptan and rizatriptan, act on specific receptors in the brain and blood vessels, constricting blood vessels and reducing inflammation. They are often effective in stopping an active migraine.
|
Oral tablets, nasal sprays, injectable solutions, and subcutaneous injections. |
| Ergot Alkaloids | Ergot alkaloids, like ergotamine and dihydroergotamine, are vasoconstrictors that reduce blood vessel dilation. They have a longer duration of action than triptans but are associated with more potential side effects. | Oral tablets, and injectable solutions. |
| Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | NSAIDs, such as ibuprofen and naproxen, reduce inflammation and pain by inhibiting cyclooxygenase enzymes. They are often used as preventative measures or to alleviate mild to moderate migraine pain. | Oral tablets, capsules, and gels. |
| CGRP Inhibitors | These newer medications, like fremanezumab and erenumab, target calcitonin gene-related peptide (CGRP), a protein implicated in migraine pain. They are administered by injection and can be effective in preventing migraine attacks. | Injectable solutions. |
| Opioids | Opioids, such as codeine and oxycodone, can provide pain relief by binding to opioid receptors in the brain, reducing the sensation of pain. However, their use is often limited due to the risk of dependency. | Oral tablets and injectable solutions. |
| Antidepressants and Anti-epileptics | Certain antidepressants and anti-epileptics, such as amitriptyline and topiramate, can be used to prevent migraines. They are often prescribed long-term to help reduce the frequency and intensity of attacks. | Oral tablets. |
Medication Forms
The form of a migraine medication can influence its absorption, onset of action, and overall effectiveness. Oral medications are convenient, but injectable or nasal spray forms may be preferred for quicker relief during a migraine attack.
Effectiveness and Side Effects
Understanding how well migraine medications work and their potential side effects is crucial for choosing the right treatment. Different medications target various migraine mechanisms and exhibit varying degrees of effectiveness, speed of action, and duration of relief. Careful consideration of these factors, alongside individual responses and potential side effects, is essential for optimal migraine management.Migraine medications often differ in their ability to address specific migraine subtypes.
For instance, some drugs might be more effective in treating common migraine, while others might be better suited for the more severe and complex hemiplegic migraine. Understanding these nuances can lead to more targeted and successful treatment plans. Furthermore, the speed of onset, duration of relief, and overall symptom reduction are key factors in evaluating a medication’s efficacy.
This information helps patients tailor their treatment strategy to their specific needs and preferences.
Effectiveness Across Migraine Subtypes
Different migraine subtypes, like common migraine and hemiplegic migraine, may respond differently to various medications. Common migraine, the most prevalent type, often responds well to a range of medications, including over-the-counter analgesics and prescription medications. Hemiplegic migraine, a more severe form, usually necessitates stronger and more targeted therapies, as it can involve neurological symptoms.
Comparison of Efficacy Factors
Evaluating medications based on factors like speed of onset, duration of relief, and overall symptom reduction helps tailor treatment to individual needs. Rapid onset is crucial for immediate relief, especially in situations where a migraine attack is causing significant discomfort. The duration of relief determines how long the benefits of the medication last. Overall symptom reduction considers the comprehensive impact of the medication on the various aspects of a migraine attack.
This multifaceted approach ensures that the chosen medication effectively addresses the individual’s specific migraine experience.
Potential Side Effects
Potential side effects associated with migraine medications vary widely depending on the specific medication class. Common side effects might include nausea, dizziness, or stomach upset. Rare but potentially serious adverse reactions are also possible. Careful monitoring of potential side effects is essential during treatment.
Table of Potential Side Effects
| Medication Class | Common Side Effects | Rare Side Effects |
|---|---|---|
| Triptans | Nausea, dizziness, tingling, sensations of heat or cold | Arrhythmias, heart attack, stroke (rare but serious) |
| NSAIDs | Stomach upset, heartburn, allergic reactions | Gastrointestinal bleeding, kidney problems |
| CGRP inhibitors | Injection site reactions, headache, flushing | Serious allergic reactions, rarely infections |
| Ergotamines | Nausea, vomiting, numbness, cold or tingling sensation | Severe blood vessel constriction, heart problems |
“Always consult with a healthcare professional before starting any new medication to discuss potential benefits, risks, and appropriate dosages.”
Dosage and Administration

Understanding the appropriate dosage and administration schedule for migraine medications is crucial for effective treatment and minimizing potential side effects. Proper adherence to these guidelines can significantly improve the management of migraine episodes. It’s vital to follow your doctor’s instructions carefully, as dosage and timing can vary based on individual needs and the specific medication.Dosage ranges for migraine medications are typically tailored to the individual patient, considering factors such as age, weight, and overall health.
A doctor will take into account the severity and frequency of migraines when prescribing medications and adjusting dosages. Administration schedules are designed to maximize the effectiveness of the medication and minimize adverse reactions. Understanding the recommended timing for both preventive and acute treatment medications is key to successful migraine management.
Dosage Ranges for Different Medications
Dosage ranges for migraine medications vary widely depending on the specific medication, the patient’s age, weight, and individual response. For example, a lower dosage may be suitable for a younger patient, while a higher dosage may be necessary for a more severe or frequent migraine sufferer. Individualized treatment plans are crucial for optimal results.
Administration Schedules
The administration schedule for migraine medications varies depending on whether the medication is used for preventive or acute treatment. Preventive medications are typically taken daily to reduce the frequency and severity of migraines, whereas acute treatment medications are used to stop an ongoing migraine attack.
Preventive Medications
Preventive medications are typically taken daily to reduce the frequency and severity of migraines. This is crucial for long-term management of the condition. Examples include certain types of antidepressants, anticonvulsants, and beta-blockers. The exact dosage and schedule will vary significantly depending on the specific medication and the patient’s needs.
Acute Treatment Medications, Medication for treating migraine
Acute treatment medications are used to stop an ongoing migraine attack. These medications typically work by targeting the underlying mechanisms of the migraine. The timing of administration is critical to achieving optimal results. Triptans, NSAIDs, and opioids are common examples.
Potential Drug Interactions
It’s essential to be aware of potential drug interactions when taking migraine medications. Some medications may interfere with the effectiveness of others, or they may increase the risk of side effects. It’s vital to inform your doctor about all medications, supplements, and herbal remedies you are taking to avoid any negative interactions.
Table of Typical Dosage Ranges and Administration Methods
| Medication Type | Typical Dosage Range | Administration Method | Notes |
|---|---|---|---|
| Triptans (e.g., Sumatriptan) | 5-100mg, depending on the medication and individual needs | Oral, nasal spray, or subcutaneous injection | Use only as directed, and avoid taking multiple doses within a short period. |
| NSAIDs (e.g., Ibuprofen) | 200-800mg, depending on the medication and individual needs | Oral | Consider taking with food to reduce stomach upset. |
| Opioids (e.g., Codeine) | 15-60mg, depending on the medication and individual needs | Oral | Use with caution due to potential for dependence. |
| Preventive Medications (e.g., Topiramate) | 25-200mg daily, depending on the medication and individual needs | Oral | Dosage and timing should be determined by a healthcare professional. |
Patient Considerations and Selection
Choosing the right migraine medication is crucial for effective management. A personalized approach, considering individual patient factors, is key to achieving optimal results and minimizing potential side effects. This involves understanding the patient’s medical history, allergies, potential drug interactions, and educating them about the medication’s use and possible side effects. Effective management of any side effects is also paramount.
Patient Medical History
A thorough understanding of the patient’s medical history is essential for appropriate medication selection. Pre-existing conditions, such as hypertension, cardiovascular issues, or liver or kidney problems, can influence medication choices. For instance, a patient with a history of kidney disease might require a different dosage or a different medication altogether to avoid potential complications. Similarly, a patient with a history of bleeding disorders might need to be closely monitored for increased bleeding risk if taking certain migraine medications.
Allergies and Drug Interactions
Identifying potential allergies to specific medications is critical. A detailed allergy history, including past reactions to medications, food, or other substances, helps to prevent adverse reactions. Moreover, assessing potential drug interactions is equally important. Certain medications can interact with migraine treatments, potentially leading to unwanted side effects or reduced effectiveness. For example, some migraine medications can interact with blood thinners, potentially increasing the risk of bleeding.
A thorough medication reconciliation and review of all medications the patient is currently taking is vital.
Patient Education
Educating patients about their medication is a cornerstone of effective migraine management. Patients need clear instructions on dosage, administration, potential side effects, and when to contact their healthcare provider. This includes understanding the importance of adhering to the prescribed regimen and reporting any unusual symptoms. Comprehensive patient education materials, including written instructions, videos, and interactive sessions, should be provided to enhance understanding and promote adherence.
This proactive approach empowers patients to actively participate in their treatment.
Finding the right medication for migraine headaches can be a real challenge, isn’t it? Sometimes, seemingly unrelated health issues can affect how well migraine treatments work. For example, if you’re using a CPAP machine for sleep apnea, you might wonder if it could be contributing to your illness. It’s worth looking into potential side effects and whether or not CPAP can make you sick, as this can impact your migraine treatment response.
Checking out this resource on can cpap make me sick could offer valuable insights, which could then help you fine-tune your migraine management strategy. Ultimately, open communication with your doctor is key to finding the best migraine treatment plan for you.
Managing Medication Side Effects
Addressing potential side effects is crucial for patient adherence and satisfaction. Mild side effects, such as nausea or drowsiness, can often be managed with lifestyle adjustments, such as dietary changes or adjusting sleep schedules. More severe side effects require prompt medical intervention. Patients should be instructed to report any concerning side effects immediately to their healthcare provider.
Furthermore, establishing clear communication channels between the patient, their healthcare provider, and the pharmacist can facilitate proactive management and minimize any negative impacts.
Important Patient Considerations
| Patient Consideration | Explanation |
|---|---|
| Medical History | Pre-existing conditions (e.g., hypertension, cardiovascular disease, liver/kidney problems) can affect medication choices. |
| Allergies | Detailed allergy history is crucial to avoid adverse reactions. |
| Drug Interactions | Assess potential interactions with other medications the patient is taking. |
| Patient Education | Clear instructions on dosage, administration, potential side effects, and when to contact healthcare provider. |
| Side Effect Management | Strategies for managing mild side effects (e.g., lifestyle adjustments) and reporting severe side effects to healthcare provider. |
Over-the-Counter (OTC) Medications
Over-the-counter (OTC) medications are often the first line of defense against migraine pain. These readily available options can provide significant relief for many sufferers, especially for mild to moderate migraines. However, their effectiveness varies considerably, and it’s crucial to understand their limitations. Knowing which OTC medication might work best for you is essential for managing your migraine episodes.OTC pain relievers, while commonly used, aren’t a one-size-fits-all solution.
Individual responses to these medications can differ, and their efficacy can vary depending on the severity and type of migraine experienced. Understanding the mechanisms of action and potential side effects is vital for informed decision-making.
Commonly Used OTC Medications
Many over-the-counter pain relievers, such as ibuprofen and acetaminophen, are commonly used to treat migraine pain. These medications are often readily available and relatively inexpensive, making them a popular choice for many individuals. Understanding their specific mechanisms of action can help determine their effectiveness.
Finding the right medication for migraines can be a real journey, sometimes feeling like a needle in a haystack. While dealing with the throbbing pain, it’s important to be aware of other potential sleep disorders that might be intertwined. For example, some of the unusual sensations experienced during sleep paralysis can mimic migraine symptoms, leading to confusion.
If you’re experiencing unusual feelings during sleep, exploring resources like symptoms of sleep paralysis might help you understand the different possibilities and, ultimately, find the right medication for your migraine.
Mechanisms of Action and Effectiveness
Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, work by inhibiting the production of prostaglandins, which are chemicals that contribute to inflammation and pain. This anti-inflammatory action can reduce the throbbing pain associated with migraines. Acetaminophen, on the other hand, works by a different mechanism, targeting the central nervous system to reduce pain signals. Its effectiveness varies depending on the individual and the severity of the migraine.
Limitations of OTC Medications
While OTC medications can provide relief, they aren’t always effective for everyone. Some individuals may not experience sufficient pain relief, and others may experience side effects. The limitations of OTC medications often include their limited effectiveness in treating severe migraines, and the potential for adverse reactions in sensitive individuals. Additionally, some individuals may find that their effectiveness diminishes over time due to tolerance.
Comparison of Ibuprofen and Acetaminophen
| Medication | Mechanism of Action | Effectiveness | Side Effects |
|---|---|---|---|
| Ibuprofen | Inhibits prostaglandin production | Generally effective for mild to moderate migraines, particularly those associated with inflammation. | Potential for stomach upset, gastrointestinal bleeding, and allergic reactions in susceptible individuals. |
| Acetaminophen | Reduces pain signals in the central nervous system | Can be effective for some individuals with mild to moderate migraines, but often less effective than ibuprofen for migraines with inflammation. | Rare but potential for liver damage with excessive use or in individuals with pre-existing liver conditions. |
Ibuprofen tends to be more effective for migraines that involve inflammation, whereas acetaminophen may be more suitable for those without prominent inflammatory components. It’s important to consider individual tolerance and potential side effects when choosing between these two medications.
Preventive Medications: Medication For Treating Migraine
Chronic migraine sufferers often find relief through preventive medications, which aim to reduce the frequency and intensity of migraines over time. These medications work differently than acute treatments, which address an existing migraine attack. Preventive strategies are crucial for improving quality of life by minimizing the debilitating impact of chronic migraine.Preventive medications are typically prescribed when acute treatments are insufficient to manage the frequency or severity of migraine attacks.
Their long-term use helps establish a baseline of reduced migraine activity. These medications are not a cure but can significantly improve daily functioning and overall well-being for those living with chronic migraine.
Role of Preventive Medications
Preventive medications play a vital role in managing chronic migraine by targeting the underlying mechanisms that trigger migraine attacks. By modulating these mechanisms, these medications can lessen the overall burden of migraines, enabling individuals to lead more fulfilling lives. Their effectiveness in reducing migraine frequency and intensity is a significant factor in their prescription.
Examples of Preventive Medications and Mechanisms of Action
Several classes of preventive medications are available, each with its own mechanism of action. Understanding how these medications work can help patients and healthcare providers make informed decisions.
- Tricyclic antidepressants (TCAs): These medications, like amitriptyline and nortriptyline, are often prescribed for their ability to reduce nerve sensitivity and pain transmission. Their mechanism of action involves serotonin and norepinephrine reuptake inhibition, which can help regulate the nervous system’s response to pain signals.
- Beta-blockers: These medications, like propranolol, lower blood pressure and can help prevent migraine attacks by reducing the dilation of blood vessels in the head. Their effect on the autonomic nervous system helps reduce the sensitivity of blood vessels to triggering factors.
- Anti-epileptic drugs (AEDs): Certain AEDs, such as topiramate and valproate, are used to stabilize nerve activity and reduce the frequency of migraine attacks. They work by modulating various neurotransmitter systems that contribute to migraine triggers.
- CGRP inhibitors: This newer class of medications, like erenumab and fremanezumab, directly targets calcitonin gene-related peptide (CGRP), a protein implicated in migraine pathophysiology. They inhibit CGRP’s role in inflammation and vasodilation, thereby preventing migraine attacks.
Benefits and Drawbacks of Preventive Medications
The table below summarizes the potential benefits and drawbacks of various preventive migraine medications. It’s important to consult with a healthcare professional to determine the most suitable option for individual needs.
| Medication Class | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Tricyclic antidepressants (TCAs) | Effective in reducing migraine frequency and intensity; potentially helpful for other conditions like anxiety and depression | Sedation, weight gain, dry mouth, constipation, and blurred vision; may interact with other medications |
| Beta-blockers | Effective in reducing migraine frequency and intensity; useful for other cardiovascular conditions | Fatigue, dizziness, and bradycardia (slow heart rate); may interact with other medications |
| Anti-epileptic drugs (AEDs) | Effective in reducing migraine frequency and intensity; potentially helpful for other neurological conditions | Drowsiness, dizziness, cognitive impairment, and gastrointestinal issues; may interact with other medications |
| CGRP inhibitors | Highly effective in reducing migraine frequency and intensity; fewer side effects compared to other classes | Injection-related reactions, potential for allergic reactions; relatively high cost |
Emerging Treatments
The quest for more effective and targeted migraine treatments is an ongoing endeavor. Researchers are exploring innovative approaches beyond the existing medications, with a focus on understanding the complex mechanisms driving migraine attacks. This involves investigating novel drug targets and exploring therapies that address the underlying causes of the condition.
New Medication Developments
Recent research has highlighted several promising avenues for developing new migraine medications. One area of intense focus is the identification of specific proteins and pathways involved in migraine pathophysiology. Targeting these pathways with novel drugs holds the potential to prevent or significantly reduce the severity of migraine attacks. This targeted approach aims to minimize side effects by directly impacting the mechanisms of migraine, rather than broadly affecting the entire nervous system.
Potential Future Treatment Options
Future migraine treatments might incorporate a combination of therapies. This could include medications acting on multiple pathways, potentially offering more comprehensive relief. Personalized medicine, tailoring treatments to individual patient profiles, is also emerging as a potential approach. Understanding genetic predispositions and individual responses to various medications could lead to more effective and less harmful treatments for each patient.
Emerging Therapies and Research
A significant area of research focuses on neuromodulatory therapies, such as transcranial magnetic stimulation (TMS). TMS, which delivers magnetic pulses to the brain, has shown some promise in reducing migraine frequency and intensity in preliminary studies. Other emerging therapies include targeted biologics, which aim to address specific immune responses that might contribute to migraine development.
Latest Clinical Trials and Research Findings
Clinical trials investigating novel migraine medications are often focused on efficacy and safety. Positive results from these trials, indicating reduced migraine frequency or intensity with fewer side effects, are crucial for advancing the field. These studies typically compare the new treatment to existing therapies or a placebo to establish its clinical superiority. For example, a recent trial on a novel CGRP antagonist showed a significant reduction in migraine days compared to placebo, highlighting the potential of this class of medications.
Emerging Treatments: A Summary Table
| Emerging Treatment | Mechanism of Action | Current Research Status |
|---|---|---|
| CGRP Antagonists (new formulations) | Block the release of calcitonin gene-related peptide (CGRP), a key player in migraine pain transmission. | Showing promising results in clinical trials, with ongoing studies exploring different formulations and dosages. |
| TMS | Non-invasive brain stimulation that modulates neuronal activity in the brain. | Preliminary studies suggest potential benefits in reducing migraine frequency and intensity. Further large-scale trials are needed to confirm the efficacy and safety. |
| Targeted Biologics | Intervene in specific immune responses potentially contributing to migraine. | Early-stage research is promising but requires further investigation to understand their efficacy and potential side effects. |
| Combination Therapies | Combining existing medications or novel therapies to target multiple migraine pathways. | Research is ongoing to identify optimal combinations and their effects on migraine. |
Drug Interactions and Contraindications
Understanding potential drug interactions and contraindications is crucial for safe and effective migraine treatment. Many medications interact with migraine therapies, potentially leading to adverse effects or reduced efficacy. Knowing which medications to avoid and how to manage potential complications is essential for patients to make informed decisions about their care.
Potential Drug Interactions
Several medications can interact with migraine treatments, either increasing or decreasing their effectiveness. These interactions can manifest in various ways, including altered absorption, metabolism, or excretion of the drugs. For example, some medications can inhibit the breakdown of migraine medications, leading to higher concentrations in the bloodstream and potentially more severe side effects. Conversely, some medications can accelerate the clearance of migraine drugs, reducing their therapeutic impact.
- Certain antidepressants, anti-anxiety medications, and blood pressure drugs can interact with migraine medications, altering their effectiveness or increasing the risk of side effects. For instance, MAO inhibitors (monoamine oxidase inhibitors) can interact with triptans, potentially causing severe hypertension.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, while often used for pain relief, can sometimes interfere with the absorption or efficacy of migraine-specific medications. For example, NSAIDs may reduce the absorption of triptans, decreasing their effectiveness.
- Oral contraceptives and certain herbal supplements can also interact with migraine medications. For example, some herbal remedies like St. John’s Wort can accelerate the metabolism of certain migraine medications, potentially reducing their efficacy.
Contraindications Based on Medical History
Certain medical conditions can contraindicate the use of specific migraine medications. These conditions may increase the risk of adverse effects or complications.
- Patients with cardiovascular conditions, such as uncontrolled high blood pressure, angina, or a history of stroke, should exercise caution when using triptans. Triptans can potentially exacerbate cardiovascular issues.
- Individuals with a history of severe hepatic or renal impairment may need to adjust the dosage or avoid certain migraine medications, as these conditions can affect the metabolism and excretion of these drugs. For example, some migraine medications may be contraindicated in patients with severe liver disease due to the potential for drug accumulation and toxicity.
- Patients with a history of ischemic heart disease, cerebrovascular disease, or peripheral vascular disease should avoid using triptans. These conditions increase the risk of severe cardiovascular complications with triptan use.
Consulting Healthcare Providers
Thorough consultation with a healthcare provider is essential to identify potential drug interactions and contraindications. Healthcare providers can assess individual medical histories and current medications to determine the safest and most effective treatment approach for migraines. This process helps avoid adverse interactions and ensures patient safety. Patients should disclose all medications, including over-the-counter drugs, supplements, and herbal remedies, to their healthcare providers.
Table of Common Drug Interactions and Contraindications
| Medication Category | Potential Interaction/Contraindication | Example |
|---|---|---|
| Triptans | Cardiovascular conditions (uncontrolled hypertension, angina, prior stroke), Peripheral vascular disease, ischemic heart disease | Sumatriptan may worsen angina in patients with pre-existing angina. |
| NSAIDs | Reduced absorption of triptans, potential for gastrointestinal upset | Ibuprofen may decrease the absorption of sumatriptan, making it less effective. |
| MAOIs | Increased risk of severe hypertension when combined with triptans | Combining sumatriptan with an MAOI can lead to a hypertensive crisis. |
| Certain Herbal Remedies | Accelerated metabolism of migraine medications, potentially reducing efficacy | St. John’s Wort can accelerate the metabolism of certain triptans, decreasing their effectiveness. |
Medication and Lifestyle
Migraine sufferers often find that their lifestyle plays a significant role in the frequency and severity of their headaches. Beyond the prescribed medications, incorporating healthy habits can significantly improve migraine management. This approach emphasizes a holistic strategy that complements pharmaceutical interventions.A comprehensive approach to migraine treatment recognizes the interconnectedness of lifestyle factors and medication effectiveness. By understanding and addressing lifestyle elements, individuals can actively participate in their migraine management, potentially reducing the need for frequent or high-dosage medications.
Healthy Diet for Migraine Management
A well-balanced diet can be a powerful ally in managing migraine. Certain foods and dietary patterns have been linked to migraine triggers and relief. It’s important to identify personal triggers and adjust dietary habits accordingly. Pay attention to how different foods affect your migraines.
- Avoid known triggers: Some common migraine triggers include aged cheeses, processed meats, chocolate, caffeine withdrawal, and excessive alcohol consumption. By eliminating or reducing these triggers, individuals can significantly decrease migraine frequency.
- Prioritize nutrient-rich foods: Focus on foods rich in antioxidants, vitamins, and minerals. These nutrients can support overall health and potentially reduce inflammation, which may contribute to migraine episodes.
- Hydration is key: Dehydration can trigger migraines. Maintaining adequate hydration throughout the day is essential. Carry a water bottle and sip water regularly.
Stress Management Techniques
Chronic stress is a significant migraine trigger. Developing and implementing stress management techniques is vital for effective migraine prevention and pain reduction.
- Mindfulness and meditation: Practicing mindfulness and meditation can help manage stress and anxiety, reducing the likelihood of migraine attacks. Regular practice can promote a sense of calm and emotional regulation.
- Yoga and Tai Chi: These practices combine physical postures, breathing techniques, and meditation to promote relaxation and reduce stress. They can help regulate the nervous system, leading to a decrease in migraine triggers.
- Regular exercise: Physical activity is an effective stress reliever. Regular exercise can release endorphins, which have mood-boosting and pain-relieving effects. However, exercise should be approached gradually to avoid exacerbating existing symptoms.
Importance of Regular Sleep Patterns
Adequate sleep is crucial for overall health and migraine management. Disrupted sleep patterns can significantly increase the likelihood of migraine attacks.
- Establish a consistent sleep schedule: Going to bed and waking up around the same time each day, even on weekends, can regulate the body’s natural sleep-wake cycle, leading to improved sleep quality.
- Create a relaxing bedtime routine: Establishing a calming bedtime routine, such as taking a warm bath, reading a book, or listening to soothing music, can signal to the body that it’s time to sleep.
- Optimize your sleep environment: Ensure your bedroom is dark, quiet, and cool. Use comfortable bedding and pillows to promote a restful sleep environment.
Lifestyle Changes Alongside Medication
Lifestyle changes, when combined with medication, can be a highly effective strategy for managing migraines. For example, someone might take preventive medication alongside a stress-reduction program and a healthy diet.
- Implementing these changes gradually: Introduce new lifestyle habits gradually to avoid overwhelming yourself. Small, consistent changes are more sustainable and less likely to cause setbacks.
- Creating a support system: Sharing your journey with friends, family, or a support group can provide encouragement and accountability.
- Consulting with a healthcare professional: It’s crucial to consult with a healthcare provider before making significant lifestyle changes, especially if you have underlying health conditions.
Lifestyle Recommendations to Complement Migraine Medication
By integrating these recommendations into daily life, individuals can further enhance the effectiveness of their migraine medication.
- Regular physical activity: Engage in regular physical activity, such as brisk walking, swimming, or cycling, to improve overall well-being and reduce stress.
- Mindfulness techniques: Practice mindfulness techniques, such as meditation or deep breathing exercises, to manage stress and promote relaxation.
- Adequate hydration: Maintain adequate hydration by drinking plenty of water throughout the day.
Final Review
In conclusion, managing migraines effectively often requires a multifaceted approach. Medication plays a vital role, but lifestyle factors like diet, stress management, and sleep hygiene are equally important. This guide has provided a comprehensive overview of medication options, from common over-the-counter remedies to emerging therapies. Remember, open communication with your healthcare provider is key to developing a personalized migraine management plan.




