Lower left back pain can be a debilitating issue, impacting daily life and requiring careful attention. This comprehensive guide delves into the complexities of this common complaint, exploring the potential causes, symptoms, diagnostic considerations, treatment options, and preventative strategies. We’ll examine the various anatomical structures that could be involved, from muscles and ligaments to discs and nerves, and discuss the mechanisms that lead to pain.
From understanding the difference between acute and chronic pain to exploring the role of lifestyle modifications in pain management, this in-depth look will equip you with the knowledge to navigate this challenging health concern.
Causes of Lower Left Back Pain

Lower left back pain can be a debilitating condition, impacting daily life and requiring careful investigation to pinpoint the underlying cause. Understanding the various potential sources of this pain is crucial for effective diagnosis and treatment. This exploration delves into the diverse anatomical structures that can be involved and the mechanisms through which injury or irritation might occur.Lower left back pain can stem from a wide range of factors, ranging from simple muscle strains to more complex conditions.
Careful evaluation, including a detailed medical history and physical examination, is essential to determine the specific cause. Accurate diagnosis allows for targeted treatment, maximizing the chances of successful pain management and recovery.
Anatomical Structures Involved
Several anatomical structures in the lower left back region can be implicated in pain. These include muscles, ligaments, tendons, nerves, discs, and the bony structures of the spine. Understanding the intricate interplay of these structures is key to comprehending the possible mechanisms behind the pain.
- Muscles: The muscles of the lower back, including the quadratus lumborum, psoas major, and erector spinae, play a crucial role in spinal stability and movement. Strains, sprains, or overuse can lead to pain and discomfort in the lower left back.
- Ligaments: Ligaments connect bones and provide stability to joints. Sprains of the ligaments supporting the spine, especially those in the lower lumbar region, can cause significant pain, often accompanied by stiffness and limited range of motion.
- Tendons: Tendons connect muscles to bones. Tendinopathy, or inflammation of tendons, can be a source of pain in the lower left back, often triggered by repetitive movements or overuse.
- Nerves: The sciatic nerve, and its branches, can be compressed or irritated by various conditions, leading to pain radiating down the leg (sciatica). This can be a particularly common cause of lower left back pain, especially in the lower left quadrant.
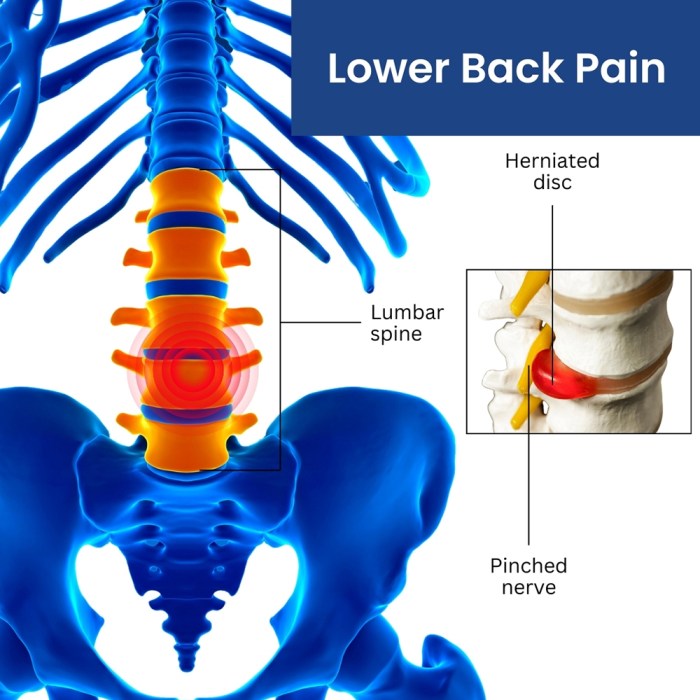
- Intervertebral Discs: Degeneration, herniation, or bulging of the intervertebral discs can compress or irritate nearby nerves, resulting in lower back pain. The location of the disc problem will often determine the location of the pain.
- Bony Structures: Spinal stenosis, a narrowing of the spinal canal, can put pressure on the nerves. Osteoarthritis or other spinal conditions can also contribute to lower left back pain.
Mechanisms of Injury or Irritation
The mechanisms responsible for injury or irritation vary based on the specific anatomical structure involved. Understanding these mechanisms can help clinicians tailor diagnostic and treatment strategies.
- Muscle Strains: Sudden or forceful movements, lifting heavy objects, or prolonged periods of poor posture can strain the muscles of the lower back. This often leads to acute pain that subsides with rest and appropriate treatment.
- Ligament Sprains: Similar to muscle strains, ligament sprains are typically caused by sudden or excessive forces on the spine, potentially due to falls or twisting motions.
- Nerve Compression: Conditions like herniated discs, spinal stenosis, or tumors can compress nerves in the lower back region, resulting in radiating pain down the leg.
- Disc Degeneration: Age-related changes, improper lifting techniques, or repetitive movements can lead to disc degeneration and subsequent pain. This is more prevalent in individuals with pre-existing conditions.
Comparison of Symptoms
| Cause | Symptoms | Possible Risk Factors | Diagnostic Considerations |
|---|---|---|---|
| Muscle Strain | Localized pain, stiffness, muscle spasms, limited range of motion | Repetitive movements, improper lifting, poor posture | Physical examination, imaging (X-ray or MRI) may not be necessary |
| Herniated Disc | Lower back pain radiating to the buttock or leg, numbness, tingling, weakness in the leg | Age, lifting heavy objects, repetitive movements, poor posture | Neurological examination, MRI to assess disc condition |
| Spinal Stenosis | Lower back pain, especially with activity, numbness, tingling in legs, worse when standing or walking | Age, genetics, previous back injuries | Physical examination, MRI to visualize spinal canal narrowing |
| Osteoarthritis | Chronic, dull aching pain, stiffness, especially in the morning, limited range of motion | Age, genetics, previous back injuries, obesity | Physical examination, X-rays to assess for joint space narrowing |
Acute vs. Chronic Lower Left Back Pain
Distinguishing between acute and chronic lower left back pain is critical for effective management. Acute pain typically lasts for a few days to a few weeks, while chronic pain persists for longer than three months. The underlying causes and treatment approaches can differ significantly.
Symptoms and Associated Factors
Lower left back pain can manifest in various ways, impacting daily life and well-being. Understanding the symptoms and associated factors is crucial for accurate diagnosis and effective management. This section delves into the common symptoms, the influence of intensity and duration on the underlying cause, and factors that can exacerbate or alleviate the discomfort.The experience of lower left back pain varies significantly from person to person, depending on the specific cause.
Some individuals might experience mild, intermittent discomfort, while others face debilitating, persistent pain. Understanding these variations is vital in determining the appropriate course of treatment.
Common Symptoms, Lower left back pain
Lower left back pain often presents with sensory symptoms such as pain, tingling, and numbness. The pain may be localized to the lower left back or radiate to other areas, like the buttocks, groin, or even the leg. Tingling and numbness can accompany the pain, affecting sensation in the affected area. Motor symptoms, such as weakness or loss of function in the leg muscles, can also be present.
In certain cases, autonomic symptoms, including changes in bowel or bladder function, might occur. These symptoms can range from mild alterations to more significant issues.
Lower left back pain can be a real pain, and it’s important to figure out the cause. While sometimes it’s related to posture or overuse, it could also be connected to catching a cold. Knowing how long cold germs live on surfaces is crucial for prevention. For example, understanding that some cold viruses can linger for hours or even days on doorknobs and other common surfaces can help you avoid getting sick, and therefore help prevent the lower back pain that often accompanies illness.
So, if you’re experiencing this pain, take a look at how long do cold germs live on surfaces to learn more about hygiene practices to minimize your risk. This knowledge can help you stay healthier and reduce the chance of experiencing that pesky lower back pain.
Intensity and Duration of Pain
The intensity and duration of lower left back pain are often correlated with the underlying cause. Acute pain, typically lasting less than six weeks, is frequently associated with injuries like muscle strains or sprains. Chronic pain, lasting longer than three months, may indicate more complex conditions such as degenerative disc disease or spinal stenosis. The severity of the pain can also fluctuate, influenced by factors such as activity levels, posture, and stress.
Factors Affecting Pain
Various factors can influence the experience of lower left back pain. Some factors can worsen the pain, while others may provide relief.
Lower left back pain can be a real pain in the neck, sometimes making it hard to even breathe comfortably. While it’s often a simple issue like muscle strain, it can also be a symptom of something more serious, like certain types of cancer. Interestingly, some studies show that lung cancer survival without treatment varies greatly depending on the stage and type of cancer, which is something to consider if you’re researching potential causes of your pain.
lung cancer survival without treatment Ultimately, it’s crucial to see a doctor for a proper diagnosis and treatment plan for any persistent back pain.
Aggravating and Alleviating Factors
| Aggravating Factors | Alleviating Factors |
|---|---|
| Prolonged standing or sitting | Regular exercise, especially low-impact activities like swimming or walking |
| Lifting heavy objects | Maintaining good posture |
| Sudden movements or twisting | Applying heat or ice packs |
| Stress and anxiety | Relaxation techniques, such as yoga or meditation |
| Poor sleep posture | Using supportive pillows and mattresses |
Relationship with Systemic Conditions
Lower left back pain can sometimes be a symptom of a broader systemic issue. For instance, conditions like inflammatory arthritis, infections, or certain cancers can manifest as back pain, often accompanied by other symptoms. Identifying any accompanying symptoms or medical history is essential to determine if the back pain is a standalone issue or part of a more extensive health concern.
A thorough evaluation by a healthcare professional is necessary to rule out potential systemic causes.
Diagnostic Considerations
Pinpointing the exact cause of lower left back pain requires a systematic approach, combining a thorough patient history, physical examination, and appropriate diagnostic tests. This process aims to differentiate between various potential causes, ranging from simple muscle strains to more serious conditions. A correct diagnosis is crucial for developing an effective treatment plan tailored to the specific underlying issue.
Diagnostic Procedures for Lower Left Back Pain
A comprehensive diagnostic strategy for lower left back pain involves a stepwise approach. First, a detailed patient history is gathered, followed by a physical examination. Imaging techniques, such as X-rays, MRIs, and CT scans, may be necessary to visualize the structures within the spine. This multifaceted evaluation helps clinicians determine the source of the pain and develop a treatment plan.
Imaging Techniques in Evaluating Lower Left Back Pain
Different imaging modalities offer varying levels of detail in visualizing the spine and surrounding structures. X-rays are relatively inexpensive and readily available, providing a basic view of bone structures. They are useful for detecting fractures, dislocations, or significant bony abnormalities. MRI scans offer superior soft tissue visualization, making them valuable in assessing spinal discs, ligaments, muscles, and nerves.
They are particularly helpful in identifying herniated discs, spinal stenosis, or tumors. CT scans, on the other hand, provide detailed cross-sectional images of the spine and surrounding tissues. They are often used to assess complex fractures or bony abnormalities, and can be particularly useful in cases where detailed bone structure is needed.
Role of Physical Examination in Assessing the Source of the Pain
A comprehensive physical examination plays a critical role in evaluating lower left back pain. The examination involves assessing posture, range of motion, muscle strength, reflexes, and neurological function. Specific tests may be performed to pinpoint the source of pain, such as checking for muscle spasms, nerve impingement, or tenderness over specific structures. These findings, combined with the patient’s history, help to narrow down the potential causes of the pain and guide further diagnostic testing.
Summary of Diagnostic Tests
| Diagnostic Test | Procedure | Potential Findings |
|---|---|---|
| X-ray | Low-dose radiation imaging of the spine. | Fractures, dislocations, bony abnormalities, narrowing of the spinal canal (stenosis), and arthritis. |
| MRI | Using strong magnetic fields and radio waves to create detailed images of soft tissues. | Herniated discs, spinal stenosis, tumors, ligament tears, and muscle injuries. |
| CT Scan | Using X-rays and a computer to create detailed cross-sectional images of the spine. | Complex fractures, bony tumors, spinal infections, and subtle bony abnormalities that might not be apparent on X-rays. |
Significance of a Thorough Patient History
A detailed patient history is essential in the diagnostic process. The history should include the onset, location, and duration of the pain; any associated symptoms, such as numbness, tingling, or weakness; and any relevant medical history or risk factors. The patient’s description of their activities and movements that aggravate or alleviate the pain provides valuable clues. For instance, if the pain worsens with prolonged standing or lifting, it may suggest a mechanical issue, while radiating pain might indicate nerve involvement.
A thorough history provides a foundation for evaluating potential causes and directing the diagnostic workup.
Treatment Approaches: Lower Left Back Pain
Lower left back pain can be effectively managed through a combination of conservative and interventional strategies. Understanding the underlying cause is crucial for selecting the most appropriate treatment plan. The goal is not just to alleviate pain, but also to address the root cause and prevent future episodes. Early intervention often leads to better outcomes.Effective treatment for lower left back pain involves a multifaceted approach tailored to the individual’s specific needs and the nature of their condition.
This encompasses a range of options, from simple lifestyle modifications to more intensive medical interventions. The choice of treatment often depends on the severity and duration of the pain, as well as the underlying cause.
Conservative Approaches
Conservative treatments aim to alleviate pain and improve function without resorting to invasive procedures. These approaches focus on managing the symptoms and promoting healing.
- Rest and Activity Modification: Initially, periods of rest are often recommended to allow the injured tissues to heal. However, prolonged bed rest can actually hinder recovery. Gradual resumption of activities, tailored to the individual’s tolerance, is essential. Activities that aggravate pain should be avoided or modified. This may involve changing posture, adjusting work ergonomics, or modifying daily routines.
- Physical Therapy: Physical therapy plays a vital role in restoring function and alleviating pain. A physical therapist can develop a personalized exercise program to strengthen core muscles, improve flexibility, and enhance posture. This often includes targeted stretches, strengthening exercises, and manual therapy techniques to address specific muscle imbalances and joint restrictions.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can provide temporary pain relief. Heat can help relax muscles, while cold can reduce inflammation. The use of heat or cold should be guided by a healthcare professional and should not be applied directly to the skin for extended periods.
- Lifestyle Modifications: Maintaining a healthy weight, adopting proper posture, and engaging in regular low-impact exercise are crucial for long-term pain management. Maintaining a healthy weight can significantly reduce stress on the spine. Good posture habits can prevent further strain. Regular low-impact exercise helps maintain muscle strength and flexibility, supporting spinal health.
Interventional Approaches
Interventional treatments are typically reserved for cases where conservative approaches have not been successful in alleviating pain or restoring function.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are frequently used to reduce inflammation and pain. Muscle relaxants may also be prescribed to help alleviate muscle spasms. In some cases, opioids may be considered for short-term use, but their long-term use is often discouraged due to potential side effects. A healthcare professional should carefully assess the risks and benefits of opioid use.
Medications should always be used as directed by a healthcare professional.
- Injections: Corticosteroid injections into the affected area can help reduce inflammation and pain. These injections are typically used for short-term pain relief. Other types of injections, such as nerve blocks, may be considered to target specific nerves contributing to pain.
- Surgical Interventions: Surgery is typically a last resort for lower back pain. Surgical procedures may be necessary in cases of severe nerve compression, structural damage, or persistent pain that significantly impairs daily activities. The decision to pursue surgery should be made in consultation with a spine specialist and should consider the potential risks and benefits of the procedure.
Lower left back pain can sometimes be a real pain in the neck, literally! It’s often a tricky one to pinpoint, and sometimes, a surprising culprit is a bowel issue. If you’re experiencing discomfort, trying some home remedies for a potential blockage might be helpful. For instance, learning how to loosen a bowel blockage at home can be a game-changer.
Check out this helpful guide how to loosen a bowel blockage at home for tips on gentle approaches. Even if it’s not the cause, these strategies might still help alleviate the pressure and, ultimately, your lower left back pain.
Role of Medication
Medications play a significant role in managing lower back pain, especially in the short term.
- NSAIDs: Nonsteroidal anti-inflammatory drugs, such as ibuprofen and naproxen, are frequently used to reduce inflammation and pain associated with musculoskeletal conditions. These medications can effectively reduce inflammation and relieve pain.
- Muscle Relaxants: Muscle relaxants are often used to address muscle spasms that may contribute to pain and discomfort. Their effectiveness in alleviating pain can vary among individuals.
- Opioids: Opioids are sometimes prescribed for severe pain, but their use is often limited due to potential side effects and the risk of addiction. They should only be considered after careful consideration of the risks and benefits.
Prevention and Self-Care
Lower back pain, particularly in the left side, can be significantly impacted by lifestyle choices. Understanding these factors and implementing proactive strategies can significantly reduce your risk and alleviate discomfort. This section focuses on preventative measures and self-care techniques to manage and potentially prevent future episodes of lower left back pain.Taking a proactive approach to lower back health is crucial.
By addressing lifestyle factors, practicing specific exercises, and maintaining good posture, you can substantially reduce your risk of experiencing this type of pain. This involves more than just reacting to pain; it’s about actively fostering a healthier spine.
Lifestyle Factors Contributing to Risk
Maintaining a healthy weight and engaging in regular physical activity are fundamental to preventing lower back pain. Sedentary lifestyles, a lack of core strength, and poor posture can all contribute to the development of this condition. Maintaining a balanced diet and avoiding excessive weight gain or sudden weight loss are crucial. Poor posture, whether during work or leisure activities, can strain the muscles and ligaments supporting the spine, increasing the risk of pain.
Exercises and Stretches for Prevention and Relief
Regular stretching and targeted exercises are vital for maintaining spinal health and flexibility. Strengthening the core muscles, which support the spine, is paramount. These exercises not only reduce the risk of injury but also improve overall body mechanics, which are crucial in preventing pain.
- Core Strengthening Exercises: Plank variations, crunches, and bridges help build core strength. These exercises stabilize the spine and reduce strain during daily activities.
- Back Stretches: Gentle stretches targeting the lower back muscles, like hamstring stretches and spinal twists, increase flexibility and reduce muscle tension. Proper stretching helps maintain a healthy range of motion for the spine.
- Strengthening Back Muscles: Exercises like back extensions and rows strengthen the muscles supporting the spine, reducing the likelihood of injury and pain.
Maintaining Good Posture and Body Mechanics
Proper posture is essential for preventing strain on the lower back. Maintaining an upright posture during work, sitting, and standing is crucial. Avoiding slouching or hunching can significantly reduce the risk of pain. Consider using ergonomic tools, such as adjustable chairs, to support good posture in the workplace. Careful attention to body mechanics during lifting and carrying objects is equally important.
Healthy Weight and Regular Physical Activity
Maintaining a healthy weight significantly reduces the stress on the spine. Excess weight puts additional pressure on the lower back, increasing the risk of pain and injury. Regular physical activity, including cardiovascular exercise and strength training, improves overall fitness and helps maintain a healthy weight. Regular activity also strengthens the muscles that support the spine, promoting spinal health.
Preventative Measures, Effectiveness, and Potential Side Effects
| Preventive Measure | Effectiveness | Potential Side Effects |
|---|---|---|
| Maintaining a healthy weight | High. Reduces stress on the spine. | Requires dietary changes and consistent exercise. Potential for emotional distress if not approached gradually and supported. |
| Regular physical activity | High. Strengthens supporting muscles and improves flexibility. | May cause minor muscle soreness initially. Proper warm-up and cool-down are essential. |
| Proper posture | High. Reduces strain on the spine. | Requires conscious effort and may require ergonomic adjustments. |
| Core strengthening exercises | High. Stabilizes the spine and improves support. | May cause minor muscle soreness initially. Proper form is crucial to avoid injury. |
| Back stretches | Moderate to High. Improves flexibility and reduces tension. | May cause discomfort if not performed correctly. Consult a physical therapist for guidance. |
Illustrative Case Studies (No Images)
Understanding lower left back pain requires analyzing diverse patient presentations. Case studies offer valuable insights into the diagnostic process, treatment options, and the importance of a thorough patient history. These examples highlight the complexity of this condition and emphasize the crucial role of patient education in achieving optimal outcomes.
Case Study 1: Mechanical Lumbar Strain
This case involves a 35-year-old female office worker experiencing sudden onset lower left back pain after lifting a heavy box. Symptoms included sharp, localized pain radiating to the left buttock, aggravated by movement and relieved by rest. She reported no prior back issues.Diagnostic workup included a physical examination, which revealed tenderness to palpation over the left lumbar paraspinal muscles.
Radiographic imaging (X-rays) showed no fractures or dislocations. The diagnosis was a mechanical lumbar strain.The treatment plan focused on conservative management: rest, ice application, over-the-counter pain relievers, and physical therapy. Exercises focused on core strengthening and lumbar stabilization were prescribed. Patient education emphasized proper lifting techniques, posture correction, and the importance of gradual return to activity.
Case Study 2: Lumbar Radiculopathy
A 62-year-old male construction worker presented with progressive lower left back pain accompanied by numbness and tingling radiating down his left leg. The pain was described as a burning sensation, worse at night. He had a history of osteoarthritis.Diagnostic workup included a detailed neurological examination, which revealed diminished reflexes in the left lower extremity. Magnetic resonance imaging (MRI) showed a herniated disc impinging on the left L5 nerve root.
The diagnosis was lumbar radiculopathy.The treatment plan involved a combination of medication (e.g., pain relievers, anti-inflammatory drugs, and potentially corticosteroids), physical therapy focusing on nerve gliding exercises, and possibly surgical intervention (discectomy) if conservative measures failed. Patient education emphasized the importance of medication adherence, the potential for long-term management, and the need for regular follow-up appointments.
Case Study 3: The Importance of a Thorough History
A 48-year-old female teacher presented with persistent lower left back pain, gradually worsening over several months. She reported a history of stress, anxiety, and recent job-related pressures. While the pain was consistent with other cases, her emotional factors were notable.Diagnostic workup initially focused on common musculoskeletal issues. However, a detailed history revealed significant stress and anxiety. Psychological factors were recognized as contributing to the pain experience.The treatment plan incorporated physical therapy, stress management techniques (e.g., relaxation exercises, mindfulness), and counseling to address the emotional component.
Patient education focused on the interconnectedness of physical and emotional well-being, emphasizing the importance of managing stress and anxiety in the context of her pain.
Last Recap
In conclusion, lower left back pain is a multifaceted issue demanding a thorough understanding of potential causes, symptoms, diagnostic procedures, and treatment approaches. By recognizing the various factors involved, from anatomical structures to lifestyle choices, individuals can work towards effective pain management and prevention. This guide provides a roadmap to understanding and addressing this common complaint.




