Itp and covid 19 – ITP and COVID-19: Navigating the Complexities of Immune Thrombocytopenia during a Pandemic. This post delves into the potential impacts of COVID-19 on individuals with Immune Thrombocytopenia (ITP), examining everything from health effects and treatment considerations to preventive measures and ongoing research. Understanding the intricacies of this interplay is crucial for both patients and healthcare providers.
This comprehensive guide will cover the multifaceted relationship between ITP and COVID-19. We’ll explore the unique challenges faced by individuals with ITP during a pandemic, examining potential health risks, treatment strategies, and preventive measures. We’ll also discuss the ongoing research and its limitations, and conclude with the public health implications of this complex interaction.
Impact on Individuals: Itp And Covid 19
Immune thrombocytopenia (ITP) significantly impacts an individual’s health by affecting platelet production and function. COVID-19, with its potential for severe complications, adds a layer of complexity for those with ITP. Understanding the potential interactions between these conditions is crucial for appropriate management and treatment. This section will delve into the specific health effects of COVID-19 on individuals with ITP, including the potential impact of treatments and monitoring strategies.
Potential Health Effects of COVID-19
COVID-19 can trigger a range of health effects in individuals with ITP, often varying in severity. These effects can stem from the virus itself, as well as the immune response triggered in the body. Potential complications include an increased risk of bleeding due to the already compromised platelet count. This can manifest as easy bruising, nosebleeds, or even more severe internal bleeding.
Furthermore, the inflammatory response to COVID-19 can exacerbate the existing immune system dysfunction associated with ITP.
Interactions Between COVID-19 and ITP Treatments
Certain treatments for ITP, such as corticosteroids and intravenous immunoglobulin (IVIG), can influence the body’s response to COVID-19. Corticosteroids, while potentially beneficial in managing ITP, can weaken the immune system, making individuals more susceptible to infections. The same applies to the use of immunosuppressants in managing ITP, where a compromised immune response might increase the risk of contracting and developing severe COVID-19.
However, this does not mean these treatments should be discontinued without consultation with a healthcare professional.
Severity of COVID-19 Outcomes
Studies suggest that individuals with ITP may experience a higher risk of severe COVID-19 outcomes compared to those without the condition. This is likely due to the underlying immune dysfunction and the potential for reduced platelet counts, increasing susceptibility to severe complications. This observation highlights the importance of heightened vigilance and proactive monitoring for individuals with ITP during the COVID-19 pandemic.
The severity of the outcome often depends on the individual’s overall health and the extent of the immune compromise.
Monitoring COVID-19 Symptoms
Close monitoring of COVID-19 symptoms is crucial for individuals with ITP. Symptoms like fever, cough, shortness of breath, or fatigue can quickly escalate in individuals with weakened immune systems. Early detection allows for timely intervention and management, potentially mitigating severe outcomes. Individuals with ITP should report any unusual symptoms promptly to their healthcare provider.
Symptom Management for ITP Patients with COVID-19
| Symptom | Severity | Recommended Action | Notes |
|---|---|---|---|
| Fever | Mild to moderate | Monitor closely, maintain hydration, use over-the-counter fever reducers (with doctor’s approval) | Persistent or high fever warrants immediate medical attention. |
| Cough | Mild to severe | Stay home, use a face mask, avoid close contact with others | Severe cough or difficulty breathing requires urgent medical evaluation. |
| Shortness of Breath | Mild to severe | Seek immediate medical attention. | This is a serious symptom and may indicate respiratory distress. |
| Fatigue | Mild to severe | Rest and maintain adequate nutrition | Severe fatigue can be a sign of more severe illness. |
| Bleeding | Mild to severe | Seek immediate medical attention. Apply pressure to any bleeding site. | Any unusual bleeding warrants prompt medical evaluation. |
Treatment Considerations
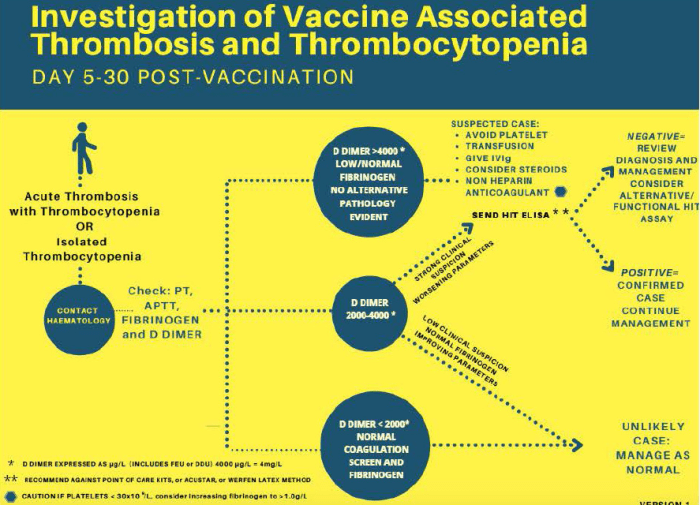
Navigating COVID-19 treatment in patients with Immune Thrombocytopenia (ITP) requires careful consideration of the interplay between the virus and the underlying condition. The delicate balance of immune system suppression needed to combat COVID-19 can exacerbate the bleeding risks inherent in ITP. This necessitates a nuanced approach to treatment protocols, taking into account the individual’s specific ITP characteristics and COVID-19 severity.Managing COVID-19 in ITP patients necessitates a comprehensive strategy that goes beyond simply treating the infection.
The primary goal is to control viral replication while minimizing the risk of bleeding complications stemming from ITP. This requires close monitoring of platelet counts and prompt intervention when necessary.
Challenges in Managing COVID-19 in ITP Patients
ITP patients face unique challenges in managing COVID-19. The delicate nature of their immune system, already compromised by the condition, necessitates a cautious approach to antiviral treatments. Furthermore, certain treatments for COVID-19 can potentially suppress platelet production, further exacerbating the bleeding risk. The risk of bleeding complications from both the virus and treatment necessitates vigilant monitoring and proactive management.
Strategies for Optimizing COVID-19 Treatment Protocols
Effective treatment strategies for COVID-19 in ITP patients require a multi-faceted approach. Early diagnosis and close monitoring are crucial. The use of antiviral medications should be carefully evaluated, considering the individual’s platelet count and bleeding risk. In cases of severe COVID-19, consideration should be given to the use of convalescent plasma therapy, with careful monitoring of the patient’s response.
A tailored treatment plan is essential to minimize adverse effects and maximize the patient’s recovery.
Recent research on ITP and COVID-19 is fascinating, but honestly, I’ve been more focused on my smoothie game lately. Adding bananas to berry smoothies, for example, can significantly boost the potassium and sweetness, a simple yet effective way to get a nutritious and delicious treat. adding bananas to berry smoothies is a great way to diversify your smoothie recipes.
Back to the science, though – the connection between ITP and COVID-19 is still being explored, and I’m hoping for more clarity soon.
Comparison of COVID-19 Treatment Options
Different treatment options for COVID-19 vary in their mechanism of action and potential side effects. Monoclonal antibodies, for instance, target specific viral proteins, while antiviral medications like remdesivir interfere with viral replication. The choice of treatment will depend on the severity of the COVID-19 infection, the patient’s overall health, and the presence of other comorbidities. In patients with ITP, the potential for bleeding complications necessitates a careful evaluation of the risks and benefits of each option.
Potential Adverse Effects of COVID-19 Treatments in ITP Patients
Certain COVID-19 treatments can have adverse effects on patients with ITP. For example, some antiviral medications can suppress platelet production, leading to further thrombocytopenia. Furthermore, the inflammatory response triggered by the infection can exacerbate bleeding, especially in patients with pre-existing low platelet counts. Careful monitoring of platelet counts and proactive management of any bleeding episodes are essential.
Summary Table of Treatment Options
| Treatment | Potential Benefits | Potential Risks | Considerations |
|---|---|---|---|
| Antiviral Medications (e.g., Remdesivir) | Potentially inhibits viral replication | May suppress platelet production, increasing bleeding risk | Careful monitoring of platelet counts and bleeding signs; alternative treatments may be necessary if platelet count drops significantly |
| Monoclonal Antibodies | Can neutralize the virus | Potential for immune-related adverse effects, including thrombocytopenia | Assess the patient’s overall immune status; close monitoring for bleeding complications is critical |
| Convalescent Plasma Therapy | May provide passive immunity | Risk of allergic reactions; potential for transmission of other blood-borne pathogens | Careful screening of plasma donors; close monitoring for bleeding or adverse reactions |
| Supportive Care | Addresses symptoms and prevents complications | May not directly combat the virus | Essential for all patients, especially those with ITP; focuses on managing symptoms and preventing further complications. |
Preventive Measures
Navigating life with Immune Thrombocytopenia (ITP) requires careful consideration of preventative measures, especially concerning infections like COVID-19. Maintaining a robust immune system is paramount, as individuals with ITP may have a compromised immune response. This necessitates a multifaceted approach to preventing COVID-19, focusing on both general hygiene and strategies tailored to the specific needs of those with ITP.
Strategies for Maintaining Immune Health
A healthy immune system is crucial for combating infections. For individuals with ITP, proactive steps to bolster immune function are vital. These strategies include a balanced diet rich in fruits, vegetables, and lean proteins, alongside adequate sleep and stress management techniques. Regular exercise, when possible and within the limitations of the condition, contributes to overall well-being and immune function.
Supplements, such as vitamin D and zinc, may play a supportive role, but should be discussed with a healthcare professional before introduction. Avoiding smoking and excessive alcohol consumption further supports immune health.
Role of Vaccination in Preventing COVID-19
Vaccination plays a crucial role in preventing severe COVID-19 outcomes. Individuals with ITP should discuss vaccination protocols with their healthcare providers. While the specific antibody response may differ, vaccination remains a key component of preventive measures. The discussion should cover potential adjustments to the vaccination schedule or dosage, if necessary, to ensure optimal protection. This personalized approach acknowledges the unique circumstances of individuals with ITP and their potential variations in immune response.
While researching Immune Thrombocytopenia (ITP) and its connection to COVID-19, I stumbled across some fascinating facts about thyroid cancer. Did you know that certain autoimmune conditions can increase the risk of developing thyroid cancer? Learning more about these connections helps us better understand the complex interplay of various health issues, and helps in the management of ITP and COVID-19 cases.
More research into this area could shed further light on how these conditions are related, ultimately paving the way for better treatments. facts about thyroid cancer Further exploration into this area is needed to fully understand the interplay between ITP and COVID-19.
Precautions for Potential COVID-19 Exposure
Proactive measures to reduce exposure to COVID-19 are essential. These include frequent handwashing, maintaining social distancing, and wearing masks in public settings. Avoiding crowded areas and poorly ventilated spaces is advisable. For individuals with ITP, these precautions should be strictly adhered to, and the potential for exposure should be mitigated. Should exposure occur, prompt communication with a healthcare provider is critical to discuss any potential complications and necessary steps.
Examples of Precautions for Potential Exposure
When dealing with potential COVID-19 exposure, proactive measures are critical. Avoid contact with individuals showing symptoms, such as fever, cough, or difficulty breathing. If possible, maintain physical distance from individuals in potentially affected environments. Practice good hand hygiene, frequently washing hands with soap and water for at least 20 seconds. Utilizing hand sanitizer with at least 60% alcohol content when soap and water are unavailable is another vital measure.
These actions, coupled with vigilance and proactive communication with healthcare providers, significantly reduce the risk of contracting the virus.
Preventive Measures Table, Itp and covid 19
| Measure | Description | Effectiveness | Considerations |
|---|---|---|---|
| Maintaining a balanced diet | Consuming fruits, vegetables, lean proteins, and adequate hydration | Supports immune function | Important for overall health; consult with a healthcare provider for dietary recommendations. |
| Regular exercise (when appropriate) | Engaging in physical activity within the limitations of ITP | Contributes to immune function and well-being | Must be tailored to individual needs and limitations; consult with a physician. |
| Vaccination | Receiving COVID-19 vaccinations, following physician recommendations | Provides significant protection | Discuss vaccination protocols and potential adjustments with the healthcare provider. |
| Hand hygiene | Frequent handwashing and use of hand sanitizer | Reduces transmission risk | Essential for preventing infection spread. |
| Social distancing | Maintaining physical distance from others | Lowers exposure risk | Adapt to specific circumstances; consider individual needs and limitations. |
Research and Studies
Investigating the intricate relationship between Immune Thrombocytopenia (ITP) and COVID-19 is crucial for understanding their potential interplay and developing targeted interventions. While the exact mechanisms linking these conditions remain unclear, ongoing research is shedding light on potential connections. This exploration will delve into current research findings, limitations, methodologies, and areas requiring further investigation.
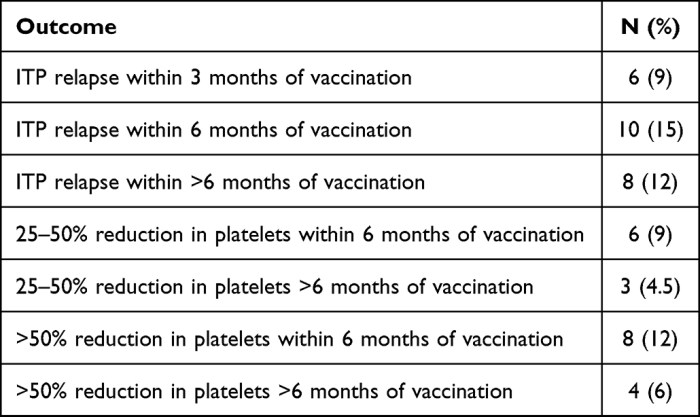
Current Research on ITP and COVID-19
Research into the connection between ITP and COVID-19 is relatively nascent. Studies have explored potential correlations, but definitive causal links are yet to be established. The limited number of cases reported with both conditions makes conclusive findings challenging. This is a key factor that influences the scope and depth of research currently available.
Limitations of Existing Research
Several limitations constrain the current understanding of the relationship between ITP and COVID-19. A primary concern is the small sample sizes in most studies. This limits the statistical power to detect subtle associations or differences. Further, the heterogeneity of ITP cases, varying in severity and underlying causes, makes it difficult to draw generalized conclusions. The lack of standardized diagnostic criteria and data collection methods across studies further hampers comparative analyses and the ability to create a comprehensive understanding of the topic.
Methodologies Employed in Studies
The methodologies used in studies investigating ITP and COVID-19 vary. Some studies have employed retrospective analyses of patient databases, comparing the characteristics of individuals with both conditions to those with only ITP or COVID-19. Others have conducted prospective cohort studies, following individuals diagnosed with both conditions over time to track outcomes. The methodologies also include case-control studies to identify potential risk factors associated with the co-occurrence of these conditions.
Areas Requiring Further Research
Future research on ITP and COVID-19 should prioritize larger, prospective studies with standardized methodologies. Such studies are needed to identify potential causal links, explore the underlying mechanisms connecting these conditions, and develop effective strategies for management and prevention. Furthermore, research should address the impact of different COVID-19 variants on ITP development or exacerbation. This includes exploring the potential role of immune dysregulation in both conditions.
I’ve been researching ITP and COVID-19 lately, and one crucial aspect that often gets overlooked is the importance of a healthy diet, especially when dealing with potential complications like hyperkalemia. A balanced diet plays a vital role in managing electrolyte imbalances, and understanding the specific dietary considerations for hyperkalemia is essential. For detailed information on a diet for managing hyperkalemia, check out this resource: diet for managing hyperkalemia.
Ultimately, a holistic approach, encompassing both medical care and dietary choices, is key to navigating the complexities of ITP and COVID-19 effectively.
Detailed analyses of immune responses and inflammatory markers in individuals with both ITP and COVID-19 are crucial.
Summary of Key Research Findings
| Study | Findings | Methodology | Limitations |
|---|---|---|---|
| Example Study 1 (Hypothetical) | A potential correlation between COVID-19 infection and subsequent ITP onset was observed in a retrospective analysis of 500 patients. | Retrospective analysis of patient records from a hospital database. | Small sample size; potential for confounding factors; lack of standardized data collection methods. |
| Example Study 2 (Hypothetical) | No significant difference in ITP severity was observed in patients with and without a history of COVID-19 infection. | Prospective cohort study following 200 patients with ITP over a 2-year period, assessing for COVID-19 infection. | Limited follow-up duration; potential for bias in patient selection. |
Public Health Implications
COVID-19’s impact on individuals with Immune Thrombocytopenia (ITP) necessitates a nuanced public health approach. Understanding the heightened vulnerability of this population to severe COVID-19 outcomes is crucial for effective preventative measures and resource allocation. The public health implications extend beyond individual care, encompassing community-wide strategies for mitigating risks and ensuring equitable access to care.
Impact of COVID-19 on Individuals with ITP
Individuals with ITP face a heightened risk of severe COVID-19 complications due to their compromised immune systems and potential for bleeding complications. Studies have shown that individuals with ITP are more susceptible to severe respiratory illness from COVID-19. This vulnerability arises from the interplay of impaired immune function, which hinders the body’s natural defenses against the virus, and the potential for bleeding complications associated with ITP, which could exacerbate the effects of COVID-19.
Importance of Public Awareness Campaigns
Public awareness campaigns are vital for educating the public about ITP and its heightened susceptibility to COVID-19. These campaigns should emphasize the importance of vaccination, mask-wearing, social distancing, and hygiene practices for individuals with ITP and their families. Clear and accessible information about preventative measures can significantly reduce the spread of the virus and protect vulnerable populations.
Role of Healthcare Systems in Managing COVID-19 Cases
Healthcare systems play a critical role in managing COVID-19 cases in patients with ITP. Prompt diagnosis and treatment are paramount, and healthcare providers need to be prepared to address the unique needs of this population. This includes understanding the potential for increased bleeding risks and tailoring treatment strategies to minimize complications. Healthcare systems must prioritize the availability of resources, such as specialized ITP clinics and telehealth services, to ensure equitable access to care for patients with ITP during the COVID-19 pandemic.
Need for Specific Guidelines for Managing COVID-19
Specific guidelines for managing COVID-19 in individuals with ITP are essential. These guidelines should detail the appropriate use of antiviral medications, the monitoring of bleeding complications, and the management of potential respiratory distress. This requires a multidisciplinary approach involving hematologists, infectious disease specialists, and pulmonologists. The guidelines must also account for potential drug interactions and the need for close monitoring of patients with ITP.
Summary Table of Public Health Implications
| Issue | Impact | Recommendations | Resources |
|---|---|---|---|
| Heightened Vulnerability | Individuals with ITP are at increased risk of severe COVID-19 complications due to compromised immune systems and potential bleeding complications. | Prioritize vaccination, mask-wearing, social distancing, and enhanced hygiene practices for individuals with ITP. | Reliable health organizations, community-based support groups. |
| Public Awareness | Lack of awareness about the specific risks for individuals with ITP can lead to preventable complications. | Public awareness campaigns emphasizing the importance of preventative measures for those with ITP. | Government health agencies, media outlets, and healthcare professional organizations. |
| Healthcare System Capacity | Healthcare systems need to be prepared to manage COVID-19 cases in patients with ITP. | Establish specialized clinics and telehealth services for patients with ITP, and train healthcare providers to manage the unique needs of this population. | Specialized ITP clinics, medical associations, and governmental funding agencies. |
| Specific Management Guidelines | Lack of tailored guidelines for managing COVID-19 in individuals with ITP can result in inadequate treatment and increased complications. | Develop and disseminate specific guidelines for the management of COVID-19 in patients with ITP, including recommendations for antiviral medications, bleeding risk monitoring, and respiratory distress management. | Medical experts, ITP societies, and healthcare providers. |
Closing Summary
In conclusion, the interplay between ITP and COVID-19 presents a significant challenge. Careful monitoring, individualized treatment plans, and robust preventive measures are crucial. Ongoing research is essential to better understand the complex dynamics of this interaction, leading to improved patient outcomes and public health strategies. This information is intended for educational purposes only and should not be interpreted as medical advice.
Always consult with a healthcare professional for personalized guidance.




