How is mono diagnosed? This question is crucial for anyone experiencing the often-misunderstood symptoms of infectious mononucleosis, commonly known as mono. This in-depth guide explores the various methods used to diagnose mono, from initial symptoms and physical examinations to laboratory tests and diagnostic criteria. We’ll break down the process step-by-step, helping you understand how healthcare professionals reach a diagnosis.
The journey to a mono diagnosis often begins with recognizing the initial symptoms. These can range from mild to severe, and sometimes mimic other illnesses. Understanding the specific symptoms and how they might present is key. This guide will delve into the different facets of the diagnostic process, allowing you to better comprehend the steps involved in determining whether or not you are suffering from mono.
We’ll also discuss potential conditions with similar symptoms, providing a clear picture of how doctors differentiate mono from other illnesses.
Initial Symptoms and Presentation
Mono, or infectious mononucleosis, often begins subtly, mimicking other common illnesses. Early detection is crucial for appropriate management and to avoid potential complications. Recognizing the initial symptoms, understanding their variations in severity, and differentiating them from other conditions like the flu is key to seeking timely medical attention.
Common Initial Symptoms
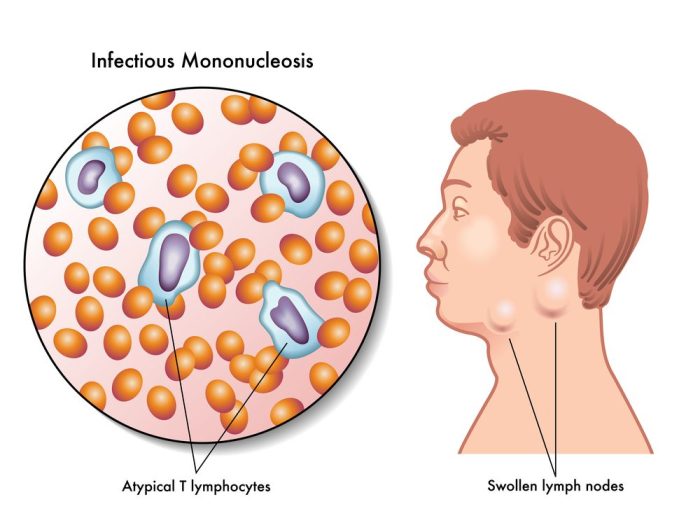
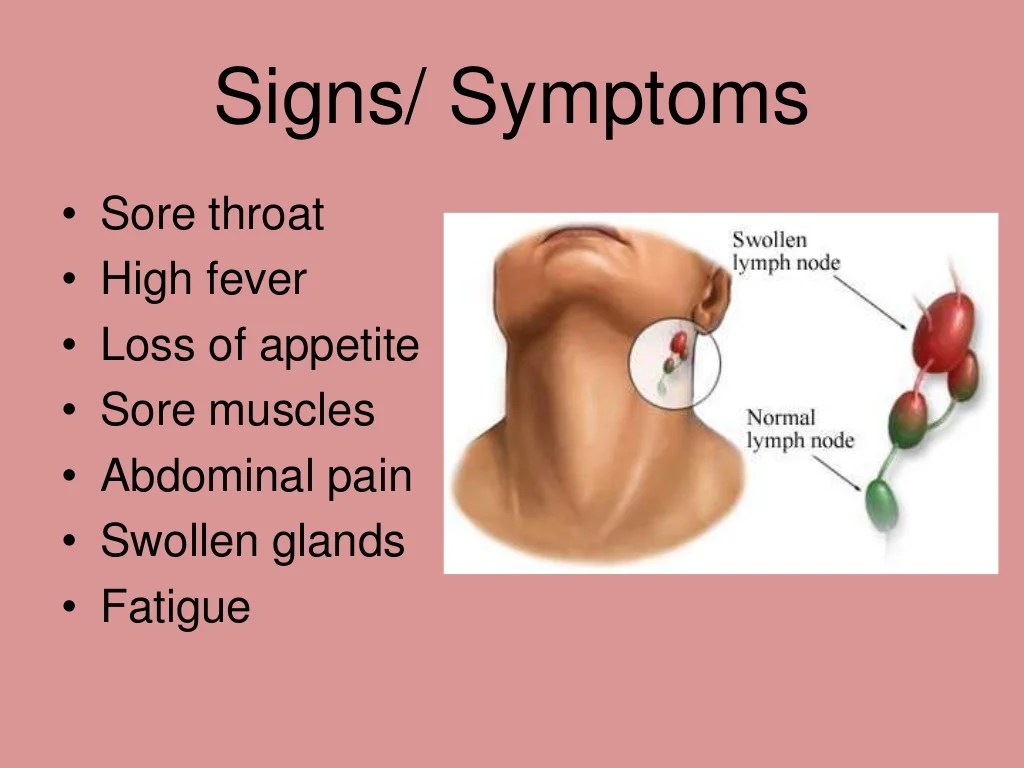
The initial symptoms of mononucleosis are often nonspecific and can be easily mistaken for other viral infections. This can delay diagnosis and appropriate treatment. Common symptoms include fatigue, fever, sore throat, and swollen lymph nodes. These symptoms typically develop gradually over several days.
| Symptom | Description | Severity Level |
|---|---|---|
| Fatigue | A profound sense of tiredness and lack of energy. Activities that would typically be easy can feel overwhelming. | Mild to Severe |
| Fever | Elevated body temperature. This can range from a slight increase to a high fever that requires medical attention. | Mild to Severe |
| Sore Throat | Painful or scratchy sensation in the throat, often worsened by swallowing. | Mild to Moderate |
| Swollen Lymph Nodes | Enlarged, tender lymph nodes, particularly in the neck, armpits, and groin. The swelling may be noticeable and cause discomfort. | Mild to Moderate |
| Headache | A general discomfort or pain in the head. Can vary in intensity. | Mild to Moderate |
| Muscle aches | Pain and tenderness in muscles throughout the body. | Mild to Moderate |
| Loss of appetite | Reduced desire to eat, leading to potential weight loss. | Mild to Moderate |
| Rash | A skin rash, sometimes appearing on the trunk or extremities. | Mild |
Differentiating Mono from Other Illnesses
It’s essential to differentiate mononucleosis from other similar illnesses, such as the flu, strep throat, or other viral infections. Misdiagnosis can lead to inappropriate treatment and delay in proper care. The following table highlights key differences.
| Symptom | Mononucleosis | Flu | Strep Throat |
|---|---|---|---|
| Sore Throat | Often severe, sometimes with exudates (pus on tonsils) | May be present, but typically not as severe as in mono | Severe, often with white patches on tonsils |
| Swollen Lymph Nodes | Common, especially in the neck and armpits | Less common | Uncommon |
| Fatigue | Profound and prolonged | Present, but typically less debilitating | Present, but typically not as severe |
| Fever | May be high, lasting several days | Often high, but may resolve quickly | May be present, but less common |
| Liver Involvement | Hepatosplenomegaly (enlarged liver and spleen) is common | Less common | Less common |
Distinguishing Mono from Flu-Like Symptoms
A key distinction lies in the duration and severity of symptoms. Flu-like symptoms, including fever, body aches, and fatigue, typically resolve within a week. In mononucleosis, these symptoms can persist for several weeks, sometimes extending to months. Additionally, the characteristic swollen lymph nodes and sore throat are more prominent features of mono. Furthermore, the presence of a noticeable fatigue and malaise that persists beyond the typical flu duration can suggest mononucleosis.
Diagnostic Methods
Identifying mononucleosis relies on a combination of clinical evaluation and laboratory tests. Careful consideration of symptoms, coupled with specific diagnostic tests, helps distinguish this condition from other illnesses with overlapping presentations. The accuracy and reliability of these tests are crucial for prompt and appropriate management.
Diagnosing mononucleosis (mono) often involves a combination of physical exams, blood tests, and sometimes a throat culture. While exploring the various treatment options, it’s important to consider the different brand name drugs in urology, like those for prostate issues or other conditions. Further blood tests, like a complete blood count, can help determine the presence of abnormal cells, which is crucial for accurate diagnosis.
Ultimately, a doctor will piece together these elements to confirm a mono diagnosis.
Common Diagnostic Tests
Several laboratory tests are commonly used to diagnose infectious mononucleosis (IM). These tests provide valuable insights into the presence and characteristics of the infection. The choice of test often depends on the availability of resources and the clinical presentation.
- Complete Blood Count (CBC): A CBC is a fundamental blood test that provides a comprehensive overview of the blood’s cellular components. It assesses red blood cell count, white blood cell count, and platelet count. This test is crucial for identifying potential abnormalities associated with IM, such as lymphocytosis (an elevated white blood cell count with a high percentage of lymphocytes).
No specific preparation is required for this test, though fasting is often recommended for other blood tests performed concurrently.
- Monospot Test: The Monospot test is a rapid, screening test used to detect heterophile antibodies. These antibodies are produced in response to certain viral infections, including Epstein-Barr virus (EBV), the primary cause of IM. The test involves mixing a patient’s serum with sheep or horse red blood cells. A positive result indicates the presence of heterophile antibodies, strongly suggesting IM.
No specific preparation is needed before this test. A false-negative result can occur early in the infection, or in individuals with weakened immune systems.
- EBV-Specific Antibody Tests: These tests directly detect antibodies specific to EBV. These tests, such as IgG and IgM antibody tests, offer a more definitive diagnosis, especially when the Monospot test is negative or inconclusive. These tests analyze the presence and type of EBV-specific antibodies in the blood, offering more information on the infection’s stage. There is no specific preparation for these tests, but similar guidelines to other blood tests might apply.
Accuracy and Limitations of Tests
The accuracy of diagnostic tests varies, with each test having inherent limitations. Understanding these limitations is critical in interpreting the results and making an informed diagnosis. The Monospot test, while rapid and inexpensive, can produce false-negative results early in the infection. EBV-specific antibody tests, though more specific, can be more expensive and take longer to obtain results.
Figuring out if you’ve got mono isn’t always straightforward. Doctors often look at symptoms like fatigue, sore throat, and swollen lymph nodes. Blood tests are usually key to confirm the diagnosis, checking for the presence of specific antibodies. While dealing with these symptoms, you might also consider techniques like scar tissue massage and management, which can help with any lingering discomfort.
Ultimately, a healthcare professional is best equipped to diagnose mono and recommend the most suitable treatment plan.
| Diagnostic Test | Sensitivity | Specificity | Limitations |
|---|---|---|---|
| Monospot | 80-90% | 90-95% | Can be false-negative early in infection, may not differentiate between EBV and other viruses |
| EBV-specific antibody tests | 95-98% | 95-99% | More expensive, may take longer to obtain results, does not definitively exclude other viral causes |
| CBC | Variable, depends on specific abnormality | Not directly diagnostic for IM | Does not definitively identify IM; other conditions can cause similar abnormalities |
Differentiating Mononucleosis from Other Conditions
Similar symptoms can be present in other illnesses. The diagnostic process includes careful consideration of the patient’s complete medical history, physical examination findings, and laboratory test results. The combination of these factors helps rule out other potential causes, such as cytomegalovirus (CMV) infection, influenza, or other viral infections. The EBV-specific antibody tests are particularly valuable in distinguishing IM from other conditions that may exhibit overlapping symptoms.
Physical Examination
A crucial part of diagnosing mononucleosis is a thorough physical examination. This involves a systematic assessment of the patient’s overall health, focusing on specific signs and symptoms that might indicate the presence of the infection. Physicians carefully evaluate various aspects, from vital signs to specific areas affected by the illness, to aid in distinguishing mononucleosis from other conditions.The physical examination plays a vital role in identifying subtle clues that could point towards mononucleosis.
By evaluating the patient’s physical presentation, physicians can gather important information that might not be apparent from initial symptoms alone. This examination complements other diagnostic methods, contributing to a more comprehensive understanding of the patient’s condition.
Assessment of Vital Signs
Vital signs, including temperature, pulse, respiration rate, and blood pressure, provide essential initial information. Slight elevations in temperature, a rapid pulse, or increased respiratory rate can be indicative of an infection. However, these findings are not specific to mononucleosis and can be observed in various illnesses. It is the combination of these findings with other symptoms and physical examination details that helps narrow the diagnosis.
Lymphadenopathy
Lymphadenopathy, or swollen lymph nodes, is a common finding in mononucleosis. The examination involves palpating (feeling) various lymph node groups in the neck, armpits, and groin. Enlarged, tender lymph nodes, particularly in the posterior cervical chain, are a significant sign. Differentiating between mononucleosis-related lymphadenopathy and other causes of lymphadenopathy, such as infections or malignancies, often requires considering the patient’s overall clinical picture and other diagnostic findings.
Pharyngitis and Tonsillar Examination
Pharyngitis (sore throat) and tonsillar inflammation are frequent symptoms of mononucleosis. During the examination, physicians assess the appearance of the throat and tonsils. Significant findings include inflamed, reddened tonsils, often with exudates (pus). These findings are crucial in distinguishing mononucleosis from other viral or bacterial pharyngitis cases.
Hepatosplenomegaly
Hepatosplenomegaly, the enlargement of the liver (hepatomegaly) and spleen (splenomegaly), can occur in mononucleosis. Palpation of the abdomen is performed to assess the size and consistency of these organs. Significant findings include palpable liver or spleen edges, although this is not always present. It’s essential to note that similar findings might be present in other conditions, and careful differentiation is crucial.
Other Findings
Other findings during the physical examination can include skin rash, although this is less common. A maculopapular rash, for example, could be present in some patients. It’s important to note that such findings should be carefully evaluated in the context of other clinical symptoms and laboratory results.
Table of Physical Examination Findings in Mononucleosis
| Finding | Description | Significance |
|---|---|---|
| Lymphadenopathy (especially posterior cervical chain) | Swollen, tender lymph nodes | Suggestive of mononucleosis |
| Pharyngitis | Inflammation of the throat | Common symptom; look for exudates (pus) |
| Hepatosplenomegaly | Enlarged liver and/or spleen | Possible, but not always present |
| Skin rash | Maculopapular rash | Less common, needs careful consideration |
Importance of Thorough Physical Examination
A comprehensive physical examination is essential for a definitive diagnosis. It allows physicians to assess the patient’s overall condition and identify potential signs and symptoms, contributing to the diagnosis. The combination of physical findings with other diagnostic tests, such as blood tests, allows for a more precise evaluation and appropriate treatment plan.
Laboratory Tests
Confirming mononucleosis often involves a battery of laboratory tests, going beyond a simple physical exam. These tests help pinpoint the presence of the infection and distinguish it from other illnesses with similar symptoms. A comprehensive understanding of these tests is crucial for accurate diagnosis and appropriate treatment.
Complete Blood Count (CBC)
A CBC provides a broad overview of the blood’s cellular components. This is a valuable initial test for mononucleosis. It assesses the number of red blood cells (RBCs), white blood cells (WBCs), and platelets. Anomalies in these counts can offer clues to the underlying cause of the patient’s symptoms.
- Red Blood Cells (RBCs): Normal RBC count ranges from 4.5 to 5.5 million per microliter (µL) in men and 4.0 to 5.0 million per µL in women. A decreased RBC count could indicate anemia, a condition sometimes seen alongside mononucleosis. This is not always the case, though.
- White Blood Cells (WBCs): A normal WBC count typically falls between 4,000 and 11,000 per µL. In mononucleosis, a significant increase in lymphocytes, a type of white blood cell, is a common finding. This elevation is often quite noticeable, sometimes reaching 20,000 cells/µL.
- Platelets: Normal platelet counts range from 150,000 to 450,000 per µL. A decreased platelet count might suggest bleeding complications, though this is less common in mononucleosis.
Heterophile Antibody Test (Monospot)
The Monospot test is a rapid screening method for the presence of heterophile antibodies. These antibodies are produced by the immune system in response to certain infections, including Epstein-Barr virus (EBV), the culprit behind mononucleosis. The test typically involves mixing a patient’s serum with sheep or horse blood cells. A positive reaction, indicated by agglutination (clumping) of the red blood cells, suggests the presence of heterophile antibodies.
- Significance of a Positive Test: A positive Monospot test strongly suggests mononucleosis, but it’s not definitive. Other conditions can also produce heterophile antibodies.
- Significance of a Negative Test: A negative Monospot test makes mononucleosis less likely. However, a negative result doesn’t definitively rule it out. Further testing may be necessary if the clinical presentation is suggestive of mononucleosis.
Viral Antibody Tests (EBV-specific)
These tests are used to confirm EBV infection. They detect antibodies specifically targeting the Epstein-Barr virus. This is particularly important in cases where the Monospot test is negative but mononucleosis is still suspected.
- Types of EBV-specific Antibody Tests: These tests typically measure the presence of IgM and IgG antibodies directed against various EBV antigens. The presence and relative levels of these antibodies provide clues about the stage of the infection.
- Interpretation: Elevated IgM antibodies generally indicate a recent infection, while elevated IgG antibodies suggest a past or current infection. The pattern of antibody responses helps determine if the patient is currently experiencing an acute infection or has had a past encounter with the virus.
Liver Function Tests (LFTs)
LFTs assess the health of the liver. Elevated liver enzymes are sometimes observed in mononucleosis. This is because the virus can affect liver function.
- Components Measured: LFTs measure enzymes such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT). Normal ranges for AST and ALT vary slightly depending on the lab. It’s crucial to consult the specific reference values provided by the laboratory.
- Elevated Results: Elevated AST and ALT levels in mononucleosis typically point to mild liver inflammation, a common, yet usually temporary, effect of the infection. However, more severe elevations might warrant further investigation.
| Laboratory Test | Typical Result in Mononucleosis |
|---|---|
| Complete Blood Count (CBC) | Elevated lymphocytes, sometimes elevated monocytes, potentially slightly decreased RBCs |
| Heterophile Antibody Test (Monospot) | Positive |
| Viral Antibody Tests (EBV-specific) | Elevated IgM antibodies initially, followed by elevated IgG antibodies |
| Liver Function Tests (LFTs) | Potentially elevated AST and ALT |
Diagnostic Criteria: How Is Mono Diagnosed
Establishing a diagnosis of infectious mononucleosis (IM) relies on a combination of clinical findings, physical examination results, and laboratory tests. The key is recognizing a constellation of symptoms and signs that point towards IM while systematically ruling out other potential causes. This process involves careful consideration of the patient’s history, physical examination, and laboratory test results, and understanding how these factors contribute to the diagnostic criteria.
Criteria for Establishing a Diagnosis
The diagnosis of IM is not based on a single definitive test, but rather on a pattern of evidence. Clinicians consider several factors, including the patient’s age, symptom duration, and the results of various tests. The absence of other conditions, along with the presence of characteristic symptoms, plays a crucial role in establishing a probable diagnosis.
Factors Considered in Evaluation
A comprehensive evaluation considers the patient’s presentation, including the duration and severity of symptoms. The presence of specific symptoms like fever, sore throat, fatigue, and lymphadenopathy is crucial. Physical examination findings, such as enlarged lymph nodes in the neck and other areas, contribute significantly. Furthermore, laboratory results, especially those showing atypical lymphocytes and elevated heterophile antibody titers, are essential pieces of the puzzle.
Differential Diagnosis
Recognizing and excluding other potential diagnoses is equally important. Conditions like streptococcal pharyngitis, viral pharyngitis, and other infectious or non-infectious illnesses with similar symptoms must be considered. The evaluation aims to distinguish IM from these alternatives by analyzing the specific features of each case. The presence of characteristic symptoms and findings that point away from other diagnoses, such as the absence of certain bacterial infections, plays a crucial role in reaching a definitive diagnosis.
Diagnostic Criteria and Guidelines, How is mono diagnosed
Various medical organizations and guidelines provide criteria for diagnosing IM. These criteria are often based on clinical judgment, laboratory findings, and the absence of alternative diagnoses. These guidelines help standardize the diagnostic process and ensure consistent care across different healthcare settings. For instance, the Infectious Diseases Society of America (IDSA) provides specific recommendations for the diagnosis and management of IM.
Summary Table of Diagnostic Criteria
| Criterion | Description |
|---|---|
| Clinical Presentation | Presence of fever, sore throat, fatigue, lymphadenopathy, and/or splenomegaly |
| Physical Examination | Palpable, enlarged lymph nodes (particularly in the posterior cervical chain), possibly splenomegaly |
| Laboratory Tests | Elevated white blood cell count with atypical lymphocytes (greater than 10% atypical lymphocytes), positive heterophile antibody test (monospot test or other), and elevated liver enzymes (transaminases) in some cases. |
| Exclusion of Other Diagnoses | Careful consideration of other potential diagnoses, such as streptococcal pharyngitis or other viral infections, and ruling them out based on clinical presentation and test results. |
Differential Diagnosis
Pinpointing the exact cause of illness, especially when symptoms mimic others, is crucial for effective treatment. A crucial part of the diagnostic process for mononucleosis involves ruling out conditions with similar presentations. This differential diagnosis process meticulously compares and contrasts various possibilities to identify the most likely culprit. Accurate identification of the underlying cause is essential for appropriate management and to prevent potentially serious complications.
Conditions Mimicking Mononucleosis
Several conditions can present with similar symptoms to infectious mononucleosis (IM), making differentiation challenging. These include viral infections, bacterial infections, autoimmune diseases, and certain cancers. Careful evaluation of the patient’s medical history, physical examination, and laboratory findings are critical for accurate diagnosis.
Figuring out if you’ve got mono isn’t always straightforward. Doctors often look at your symptoms, like a sore throat or fatigue, and run some blood tests. Knowing proper crutch positioning and sizing is crucial for recovery, especially if your mobility is affected by mono. This can help you avoid further complications, and remember to check out crutch positioning and sizing for detailed information on proper techniques.
Ultimately, a healthcare professional will be the best resource to confirm a mono diagnosis and suggest the right recovery path.
Key Distinctions from Other Conditions
Distinguishing IM from other conditions hinges on specific characteristics. For instance, Epstein-Barr virus (EBV) infection, the primary cause of IM, typically manifests with a specific constellation of symptoms, including fatigue, sore throat, and swollen lymph nodes. Other conditions may have overlapping symptoms, but often lack the characteristic lymphocytosis and atypical lymphocytes seen in IM. Furthermore, specific laboratory markers, like elevated liver enzymes, can help distinguish IM from other conditions.
Diagnostic Approaches for Mimicking Conditions
The diagnostic approaches for conditions that mimic IM vary based on the suspected etiology. For instance, in cases of suspected cytomegalovirus (CMV) infection, polymerase chain reaction (PCR) testing for CMV DNA can be performed on blood or saliva samples. Similarly, if a bacterial infection is suspected, cultures and sensitivities can be performed. In cases of suspected autoimmune conditions, specific autoantibody testing may be warranted.
A comprehensive approach that incorporates various testing modalities is crucial for accurate diagnosis.
Comparison Table: Mononucleosis vs. Other Conditions
| Characteristic | Mononucleosis | Viral Hepatitis | Streptococcal Pharyngitis | Cytomegalovirus (CMV) |
|---|---|---|---|---|
| Symptoms | Fever, sore throat, fatigue, swollen lymph nodes, headache | Fever, jaundice, nausea, abdominal pain, fatigue | Sore throat, fever, headache, body aches, white spots on tonsils | Fever, fatigue, headache, malaise, possible organ involvement |
| Physical Findings | Swollen, tender lymph nodes, palatal petechiae, possible splenomegaly | Jaundice, hepatomegaly, splenomegaly (less common than in IM) | Red, inflamed throat, exudates (white spots) on tonsils, tender anterior cervical lymphadenopathy | Possible lymphadenopathy, hepatosplenomegaly, and signs of organ involvement |
| Laboratory Results | Elevated white blood cell count, atypical lymphocytes, positive heterophile antibody test (monospot) | Elevated liver enzymes (AST, ALT), possible jaundice, abnormal bilirubin levels | Elevated white blood cell count, positive rapid strep test, presence of group A beta-hemolytic streptococci | Positive CMV PCR, elevated white blood cell count (less dramatic than in IM), atypical lymphocytes (less frequent than in IM) |
How Differential Diagnosis Helps
The process of differential diagnosis is essential for narrowing down the possible causes of illness. By systematically comparing and contrasting various conditions, healthcare professionals can identify the most probable etiology. This process involves considering the patient’s history, physical examination findings, and laboratory results. The comparison allows for a focused approach to diagnosis and treatment, leading to more effective management of the patient’s condition.
Additional Considerations
Beyond the standard diagnostic procedures, several crucial factors can significantly influence the diagnosis of infectious mononucleosis (IM). A thorough understanding of the patient’s background, lifestyle, and recent exposures is vital in distinguishing IM from other potential illnesses. This holistic approach allows for a more accurate diagnosis and appropriate management.Patient history, encompassing various aspects of their life, plays a pivotal role in the diagnostic process.
Considering the patient’s age, lifestyle choices, and recent exposures provides context for the symptoms and helps to rule out alternative diagnoses. This nuanced approach often leads to a more precise and timely determination of the underlying cause.
Patient History in Mononucleosis Diagnosis
A comprehensive patient history is essential for evaluating the potential for mononucleosis. This includes details about recent illnesses, travel history, and contact with individuals exhibiting similar symptoms. By piecing together these elements, clinicians can gain valuable insights into the possible causes of the patient’s condition.
Importance of Age, Lifestyle, and Exposures
The patient’s age significantly impacts the likelihood of different diagnoses. For example, in younger individuals, the likelihood of IM is often higher compared to older adults. Furthermore, lifestyle factors such as frequent contact with others or participation in sports can offer clues regarding potential exposures to infectious agents. Recent travel history and exposure to individuals with known infections are crucial elements to consider.
Detailed Medical History for Ruling Out Other Causes
A detailed medical history is critical for differentiating mononucleosis from other conditions that may present with similar symptoms. This includes inquiries about previous illnesses, allergies, medications, and any underlying medical conditions. Thorough exploration of the patient’s health history allows for a more comprehensive evaluation, ensuring that all potential causes are explored and excluded before arriving at a definitive diagnosis.
Table of Considerations Based on Patient Characteristics
| Patient Characteristic | Potential Implications | Example |
|---|---|---|
| Age (young adult) | Increased likelihood of IM, potentially less severe presentation of other illnesses. | A 19-year-old college student experiencing fatigue and sore throat. |
| Age (elderly) | Lower probability of IM, higher risk of other conditions with overlapping symptoms. | A 70-year-old individual with similar symptoms may have a different underlying cause, such as a viral infection or a pre-existing condition. |
| Recent travel to endemic areas | Increased risk of infection from specific pathogens. | A patient returning from a region known for high Epstein-Barr virus prevalence. |
| Recent contact with individuals exhibiting similar symptoms | Strong possibility of contagious illness transmission. | A student who recently participated in a sports event with several infected individuals. |
| Known exposure to specific infectious agents | Indicates a probable cause of illness, such as exposure to EBV. | A patient who reports close contact with someone confirmed to have IM. |
Evaluating Factors in the Context of Mononucleosis Diagnosis
When evaluating these factors in the context of IM diagnosis, clinicians should meticulously consider each aspect of the patient’s history. For instance, if a patient reports recent contact with someone diagnosed with IM, the likelihood of infection increases significantly. This information should be integrated with the physical examination findings and laboratory test results to formulate a comprehensive and accurate diagnosis.
Last Recap
In conclusion, diagnosing mononucleosis requires a multifaceted approach. From careful observation of initial symptoms to a thorough physical exam, and various laboratory tests, the process is designed to accurately identify the presence of mono and rule out similar conditions. Understanding the diagnostic criteria, the differential diagnosis process, and additional factors like patient history, helps healthcare providers make informed decisions.
This guide has provided a comprehensive overview of how mono is diagnosed, empowering you with knowledge to navigate this process with greater understanding.




