Heel pain when walking can be debilitating, disrupting your daily activities and making even simple movements uncomfortable. This post delves into the various causes, from the common plantar fasciitis to other potential conditions. We’ll explore how to diagnose the source of your discomfort, discuss treatment options, and offer prevention strategies to keep your feet happy and healthy.
Understanding the specific symptoms and risk factors associated with each condition is key to effectively managing heel pain. This article will provide a comprehensive overview, including detailed explanations, practical advice, and helpful tables to aid in your understanding.
Causes of Heel Pain When Walking
Heel pain when walking can be a debilitating issue, impacting daily activities and quality of life. Understanding the underlying causes is crucial for effective treatment and prevention. This detailed exploration will cover common causes, their symptoms, and associated risk factors.Heel pain often stems from overuse, improper footwear, or biomechanical issues. Identifying the root cause allows for targeted interventions to alleviate pain and restore normal function.
Proper diagnosis and management are essential to prevent long-term complications.
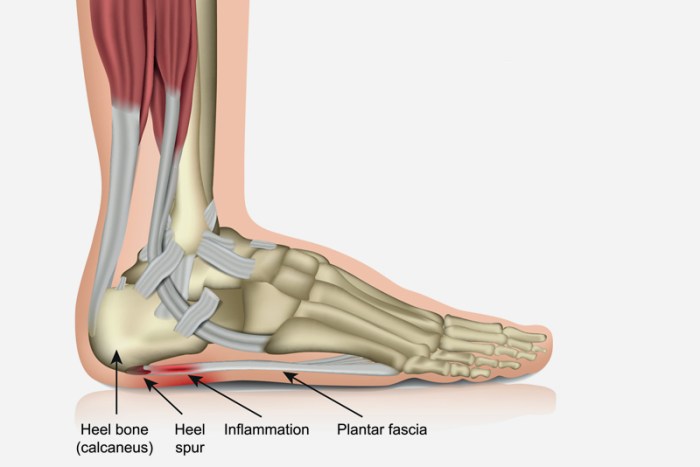
Plantar Fasciitis
Plantar fasciitis is a common cause of heel pain, characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot. The pain typically manifests as stiffness and tenderness in the heel and arch, often worse in the morning or after periods of rest. Activities like walking, running, or standing for extended periods can exacerbate the discomfort.
| Condition | Symptoms | Risk Factors |
|---|---|---|
| Plantar Fasciitis | Pain in the heel and arch, worse in the morning or after periods of rest; stiffness and tenderness; pain that increases with activity. | Overuse, flat feet, high arches, tight calf muscles, improper footwear (shoes with insufficient arch support), prolonged standing or walking, obesity, and certain sports (e.g., running). |
| Heel Spurs | A bony growth on the heel bone; pain that can radiate to the arch; pain that is worse when bearing weight. | Plantar fasciitis, overuse, tight calf muscles, flat feet, improper footwear (shoes with insufficient arch support), and biomechanical problems. |
| Achilles Tendinitis | Pain and tenderness in the back of the heel; stiffness and swelling; pain that worsens with activity. | Overuse, tight calf muscles, improper footwear (shoes with insufficient heel support), biomechanical issues, and certain sports (e.g., running). |
| Other Potential Conditions | Pain in the heel area that may be accompanied by numbness or tingling; pain that may be localized or spread out; pain that may vary in intensity. | Trauma, stress fractures, arthritis, bursitis, and nerve impingement; may also be associated with underlying medical conditions. |
Heel Spurs
Heel spurs are bony growths that develop on the heel bone. They are often associated with plantar fasciitis, as the repetitive stress and strain can cause calcium deposits to form. Symptoms typically include pain that radiates to the arch, particularly when bearing weight. This condition is often a result of chronic strain on the plantar fascia.
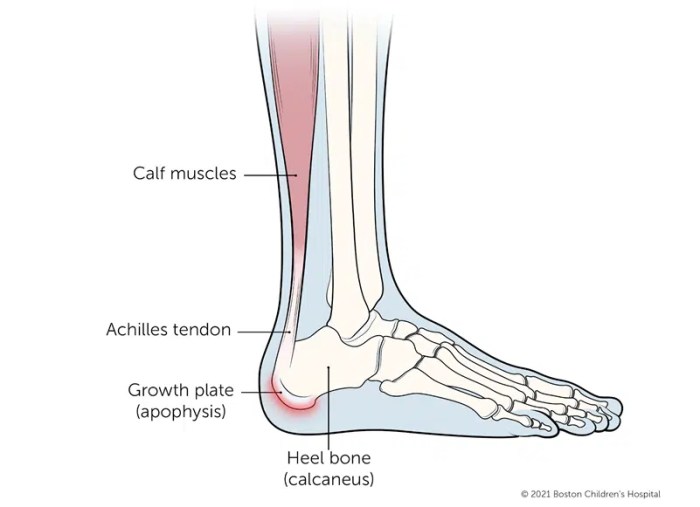
Achilles Tendinitis
Achilles tendinitis involves inflammation of the Achilles tendon, a thick band of tissue connecting the calf muscles to the heel bone. Symptoms often include pain and tenderness in the back of the heel, which worsens with activity. Stiffness and swelling may also be present. Overuse, particularly in sports requiring repetitive jumping or running, is a significant risk factor.
Other Potential Conditions
Beyond the three common causes, various other conditions can lead to heel pain. These may include stress fractures, arthritis, bursitis, or nerve impingement. The symptoms can range from localized pain to pain that spreads throughout the heel area, potentially accompanied by numbness or tingling. Underlying medical conditions can also contribute to heel pain. A thorough evaluation by a healthcare professional is necessary to accurately diagnose the specific cause.
Diagnosing Heel Pain
Heel pain, a common ailment, can stem from various underlying conditions. Accurate diagnosis is crucial for effective treatment and preventing further complications. Proper identification of the root cause allows for personalized care tailored to the specific needs of the individual. This often involves a multi-faceted approach combining patient history, physical examination, and potentially, imaging tests.Understanding the diagnostic process provides a clearer picture of how healthcare professionals arrive at a diagnosis and what to expect during the process.
That nagging heel pain when walking can be a real pain, literally! While I’m no doctor, I’ve noticed a correlation between poor air quality, like that from wood burning stoves, and general aches and pains. Studies suggest a link between the particulate matter emitted by the health hazards of wood burning stoves and increased inflammation throughout the body, potentially contributing to foot pain.
So, if you’re experiencing persistent heel pain, consider your indoor air quality. Maybe a humidifier or switching to a different heating source could help.
This approach allows for informed decision-making and a more proactive role in managing the pain.
Physical Examination
A thorough physical examination is a cornerstone of diagnosing heel pain. The examination begins with an assessment of the patient’s gait and range of motion. This involves observing how the individual walks, looking for any noticeable abnormalities or limping. A detailed examination of the affected area, including palpation to identify tenderness, swelling, or any visible abnormalities, follows.
This physical evaluation helps pinpoint the location and characteristics of the pain, offering crucial clues about the potential cause.
Medical History
Gathering a detailed medical history is equally important. Information about the onset, duration, and intensity of the pain, along with any aggravating or relieving factors, is essential. The patient’s activity level, recent injuries, and any underlying medical conditions are significant factors. A thorough history helps the healthcare provider narrow down potential causes and tailor the diagnostic approach.
For example, a history of recent intense exercise could suggest stress fractures.
Imaging Tests
Imaging tests, such as X-rays and MRIs, can provide crucial visual information about the structures within the heel. X-rays are useful for detecting bone fractures, spurs, or other bony abnormalities. MRIs offer a more detailed view of soft tissues, such as tendons, ligaments, and muscles, and can identify conditions like plantar fasciitis, tendonitis, or tears. The choice of imaging test often depends on the suspected cause of the pain, and the results are interpreted in conjunction with the medical history and physical examination.
Differentiating Causes
Precisely differentiating between various causes of heel pain is vital. Plantar fasciitis, a common culprit, often presents with pain that is worse in the morning or after periods of inactivity. Heel spurs, though often associated with plantar fasciitis, may not always cause pain. Stress fractures, on the other hand, might arise from overuse or repetitive stress. Each condition has its own characteristics, and differentiating between them allows for the selection of the most appropriate treatment plan.
Diagnostic Procedures
| Procedure | Purpose | Limitations |
|---|---|---|
| Physical Examination | Assess range of motion, palpate affected areas, and observe gait. | Subjectivity in assessment, may not identify all causes. |
| Medical History | Obtain details about pain onset, duration, intensity, and aggravating factors. | Reliance on patient recollection, potential for inaccuracies. |
| X-rays | Detect bone fractures, spurs, or other bony abnormalities. | May not visualize soft tissues, limited in identifying subtle issues. |
| MRIs | Provide detailed images of soft tissues, identify tendonitis, tears, or other soft tissue injuries. | More expensive, may require contrast agents, can be uncomfortable for some patients. |
Treatment Options for Heel Pain: Heel Pain When Walking
Heel pain can be a debilitating condition, significantly impacting daily activities. Fortunately, numerous treatment options are available, ranging from simple home remedies to more involved medical interventions. Understanding these options empowers individuals to take an active role in managing their pain and restoring their mobility.Effective treatment for heel pain often involves a combination of strategies, tailored to the specific cause and severity of the condition.
Addressing the underlying issue, whether it’s plantar fasciitis, heel spurs, or another cause, is crucial for long-term relief. This often involves a multi-faceted approach that may include both conservative and, in some cases, surgical interventions.
Conservative Treatments
Conservative treatments for heel pain aim to alleviate symptoms without resorting to surgery. These methods typically focus on reducing inflammation, improving flexibility, and providing support to the affected area. They are generally the first line of treatment for most cases of heel pain.
- Stretching Exercises: Regular stretching is essential for improving flexibility in the plantar fascia and surrounding muscles. Consistent stretching can help reduce tightness and pain, making walking and other activities more comfortable. A structured stretching routine can significantly improve symptoms and prevent recurrence.
- Icing: Applying ice packs to the heel for 15-20 minutes several times a day can help reduce inflammation and pain. This is particularly effective in the acute phase of heel pain. Proper icing technique and frequency are key to maximizing the benefits and minimizing discomfort.
- Supportive Footwear: Choosing appropriate footwear is critical for managing heel pain. Shoes with good arch support and cushioning can help distribute pressure more evenly across the foot, reducing strain on the plantar fascia. Properly fitted shoes can make a significant difference in alleviating pain and discomfort.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce pain and inflammation. However, it’s essential to follow the recommended dosage and consult a healthcare professional if symptoms persist or worsen.
- Physical Therapy: A physical therapist can design a personalized exercise program to strengthen the muscles supporting the arch of the foot. These exercises can improve flexibility, reduce pain, and improve overall foot function. A physical therapist can also advise on appropriate stretches and exercises.
Creating a Step-by-Step Stretching Guide for Heel Pain
A consistent stretching routine can significantly alleviate heel pain. The following example Artikels a simple but effective stretching routine. Remember to consult with a healthcare professional or physical therapist before starting any new exercise program.
- Heel Raises: Stand with feet shoulder-width apart. Slowly raise up onto your toes, hold for a few seconds, and then lower your heels back down. Repeat 10-15 times.
- Plantar Fascia Stretch (Wall Stretch): Stand facing a wall, with one leg slightly behind the other. Lean forward until you feel a stretch in the arch of your front foot. Hold for 30 seconds and repeat 3-4 times.
- Towel Stretch: Sit on the floor with legs extended. Loop a towel around the ball of one foot and gently pull towards you, keeping your knee straight. Hold for 30 seconds and repeat 3-4 times.
- Foot Massage: Gently massage the bottom of your foot using your fingers, focusing on the arch and heel area. This can improve blood circulation and reduce muscle tension.
Examples of Supportive Footwear
Proper footwear plays a crucial role in managing heel pain. Supportive shoes provide cushioning and arch support, reducing stress on the plantar fascia. Examples of suitable footwear include:
| Shoe Type | Description |
|---|---|
| Running Shoes with good arch support | Designed with cushioning and arch support for impact absorption and proper alignment. |
| Walking Shoes with orthotics | Offer targeted support and cushioning, especially helpful for those with existing foot conditions. |
| High-top sneakers | Provide excellent ankle support, potentially beneficial for those experiencing heel pain related to ankle instability. |
Prevention Strategies for Heel Pain
Heel pain, a common ailment, can significantly impact daily life. Fortunately, proactive measures can dramatically reduce the risk of developing or exacerbating heel pain. Understanding the factors contributing to heel pain and implementing preventive strategies are key to maintaining a healthy and active lifestyle.Proper foot mechanics, footwear selection, and targeted exercise routines are essential components of a comprehensive preventative approach.
Consistent implementation of these strategies can help to maintain healthy foot structure and function, mitigating the risk of developing painful conditions.
Foot Mechanics and Posture
Maintaining good foot mechanics and posture during daily activities is crucial for preventing heel pain. This involves conscious awareness of how your feet and body align during movement and rest. Activities like standing for extended periods, walking on uneven surfaces, or wearing ill-fitting shoes can negatively impact foot alignment and contribute to heel pain. Regular stretching exercises, particularly focusing on the calf muscles, can help maintain flexibility and reduce strain on the heel.
Also, mindful posture, maintaining a straight spine and balanced weight distribution, significantly contributes to preventing heel pain. Awareness of proper foot alignment when walking, running, or standing, and maintaining good posture are crucial.
Dealing with heel pain when walking can be a real drag, right? It can make even the simplest activities feel impossible. Sometimes, natural remedies like certain herbal supplements might help alleviate some of the discomfort. For example, discovering more about herbs like St. John’s Wort could potentially offer some insights into natural ways to manage pain, especially when considering its potential role in reducing inflammation.
Check out everything you need to know about st johns wort for a deeper dive into its potential benefits and how it might be incorporated into a pain management plan. Ultimately, though, consulting a doctor for a proper diagnosis and treatment plan is still crucial for heel pain.
Footwear Selection
Appropriate footwear plays a vital role in preventing heel pain. Choosing shoes with adequate support, cushioning, and arch support is essential. High heels, excessively flat shoes, or shoes with poor cushioning can contribute to heel pain by placing undue stress on the heel and surrounding tissues. Consider the activity for which you will be wearing the shoes, and select shoes appropriate for that activity.
For example, shoes with robust cushioning and support are crucial for running or prolonged walking. The choice of footwear depends on the individual’s foot type, activity level, and specific needs. Look for shoes that provide a secure fit, avoiding shoes that are too tight or too loose.
Exercise and Stretching
Regular exercise, specifically targeted at strengthening the muscles supporting the foot and ankle, is vital for preventing heel pain. Exercises focusing on calf stretches, arch support strengthening, and balance training can help to maintain the health and stability of the foot. Stretching the Achilles tendon and surrounding muscles is crucial. Examples of beneficial exercises include heel raises, toe curls, and calf stretches.
These exercises help to maintain flexibility and strength in the muscles responsible for supporting the heel. Incorporate these exercises into your daily routine, aiming for consistency to reap the benefits.
Preventive Measures
A proactive approach to heel pain prevention involves a combination of strategies. This encompasses careful selection of footwear, regular stretching, maintaining proper posture, and mindful movement. By implementing these measures, individuals can significantly reduce the risk of heel pain. These preventive measures are essential to protect the feet from injury.
- Regular stretching, particularly of the calf muscles and Achilles tendon, can help maintain flexibility and reduce stress on the heel.
- Maintaining good posture and proper foot alignment during daily activities can prevent excessive strain on the heel.
- Choosing supportive footwear with adequate arch support and cushioning is crucial for preventing heel pain.
- Avoiding prolonged periods of standing or walking without rest can help minimize stress on the heel.
- Utilizing appropriate supportive insoles can further enhance foot support and cushioning.
Supportive Insoles, Heel pain when walking
Supportive insoles are designed to enhance foot support and cushioning. Various types of insoles are available, each with unique characteristics and intended benefits. Understanding the differences between these insoles can help individuals choose the most appropriate option for their needs. For example, some insoles provide targeted support for the arch, while others focus on cushioning the entire foot.
| Type of Insole | Description | Benefits |
|---|---|---|
| Arch Support Insoles | Designed to provide additional support for the arch of the foot. | Reduces pressure on the arch, potentially alleviating pain. |
| Cushioning Insoles | Designed to provide added cushioning and comfort for the entire foot. | Reduces impact during activities, offering comfort. |
| Custom Orthotics | Individually designed to fit the unique shape of the foot. | Provides highly personalized support and cushioning. |
Managing Heel Pain During Activities
Heel pain can significantly impact your ability to participate in activities you enjoy, from a brisk walk to a challenging run. Understanding how to manage this pain during various activities is crucial for maintaining an active lifestyle and preventing long-term issues. This section details strategies for effectively navigating heel pain while staying active.
Strategies for Managing Heel Pain During Running
Managing heel pain during running requires a multifaceted approach that combines activity modification, rest, and supportive measures. Gradual progression in training is key to preventing flare-ups. Increasing mileage too quickly or running on hard surfaces without proper support can exacerbate heel pain.
- Gradual Progression: Incrementally increase your running distance and intensity. Start with shorter runs and gradually add time or distance over a period of weeks. Listen to your body and don’t push through pain.
- Proper Running Form: Maintaining good running form is essential for distributing stress evenly across your feet. A gait analysis by a physical therapist can identify any imbalances or flaws in your running technique and provide tailored corrective measures.
- Supportive Running Shoes: Choosing the right running shoes is paramount. Look for shoes with good arch support, cushioning, and stability. Consider consulting a running shoe specialist to find the perfect fit for your needs.
- Rest and Recovery: Incorporate rest days into your running schedule. Rest allows your body to repair and rebuild tissues, reducing the risk of further injury.
Strategies for Managing Heel Pain During Prolonged Walking
Sustained walking, whether for leisure or exercise, can also put strain on your heels. Implementing these strategies can help mitigate the pain and discomfort.
- Appropriate Footwear: Wear supportive shoes with good cushioning and arch support. Avoid walking barefoot or in shoes that lack adequate support.
- Surface Considerations: Choose softer surfaces for prolonged walks, such as grass or a well-maintained trail, rather than hard pavements or concrete.
- Walking Technique: Pay attention to your posture and stride. Maintain a steady pace and avoid overstriding. Proper posture and stride mechanics reduce the impact on your heels.
- Rest Breaks: Schedule regular rest breaks during longer walks to reduce strain on your heels and allow your feet to recover.
Modifying Activity Levels and Incorporating Rest Periods
Consistent rest periods are crucial in managing heel pain. Overexertion can lead to increased pain and hinder the healing process.
- Listen to Your Body: Pay attention to your body’s signals. If you experience pain, stop the activity and rest.
- Progressive Reduction: If you experience pain, gradually reduce your activity level rather than stopping abruptly. This approach allows your body to adapt and recover more effectively.
- Rest Days: Ensure you have adequate rest days to allow your heels to recover. A combination of rest and activity modification is a crucial strategy to avoid worsening your heel pain.
Gradual Progression When Returning to Activities
Returning to activities after a period of heel pain requires a careful and gradual approach. A sudden return can lead to a recurrence of the problem.
- Start Slowly: Begin with shorter durations of activity and gradually increase the intensity and duration as tolerated.
- Monitor Pain Levels: Pay close attention to your pain levels during and after activity. Any significant increase in pain should prompt a reduction in activity.
- Consult Healthcare Professionals: Seek guidance from a healthcare professional if you are unsure about the best way to return to your previous activity level. A physical therapist can provide personalized recommendations.
Activities and Suggested Modifications Table
| Activity | Modifications |
|---|---|
| Running | Gradually increase mileage, use proper running form, choose supportive running shoes, incorporate rest days, and monitor pain levels. |
| Prolonged Walking | Choose softer surfaces, wear supportive footwear, maintain proper posture and stride, and incorporate rest breaks. |
| Hiking | Select trails with moderate inclines, wear appropriate footwear, and take frequent breaks. |
| Stair Climbing | Use the handrails for support, maintain a slow and controlled pace, and avoid rapid ascents or descents. |
Home Remedies and Self-Care
Taking a proactive approach to managing heel pain often involves simple home remedies and self-care strategies. These methods, when combined with professional medical advice, can significantly reduce discomfort and promote healing. Addressing the root causes of heel pain through lifestyle adjustments and at-home treatments can be highly effective in the initial stages of pain management.Understanding the nature of heel pain and its underlying causes is crucial for implementing appropriate self-care measures.
Different remedies target various contributing factors, from inflammation to poor posture. This section explores practical strategies for managing heel pain at home, emphasizing the importance of consistency and monitoring for progress.
Ice and Heat Therapy
Applying ice and heat are common home remedies for managing inflammation and pain. Ice therapy is effective in reducing inflammation and swelling, while heat therapy can help relax muscles and improve blood flow. It’s important to use these therapies strategically to maximize their benefits.
Heel pain when walking can be a real drag, especially if you’re planning a long hike. Thinking about how long it takes to walk 10 miles can be a good way to gauge your fitness level and the strain on your feet. How long does it take to walk 10 miles will depend on your pace and fitness, but it’s a useful consideration for anyone dealing with heel pain when walking.
Ultimately, listening to your body and adjusting your walking routine is key to avoiding further issues.
- Ice Therapy: Applying ice packs to the affected area for 15-20 minutes at a time, several times a day, can help reduce inflammation and numb the pain. Wrap the ice pack in a thin towel to prevent skin irritation. Avoid applying ice directly to the skin for extended periods.
- Heat Therapy: Applying heat, such as a warm compress or heating pad, can help relax tight muscles and improve blood flow to the area. Use heat for 15-20 minutes at a time, several times a day. Always use caution to prevent burns. Be sure to check the heat setting regularly, especially with electric heating pads.
Rest and Elevation
Rest and elevation are crucial for allowing the injured heel to heal properly. These strategies can reduce swelling and promote blood circulation to the affected area. It is important to listen to your body and adjust your activity levels as needed.
- Rest: Avoid activities that exacerbate your heel pain. Resting allows the affected tissues to recover and reduce stress on the injured area. If you work a job that involves standing or walking for extended periods, consider modifying your tasks to minimize stress on your heels.
- Elevation: Elevating the affected foot above the heart can help reduce swelling. This promotes better blood circulation and can help alleviate pain. When sitting or lying down, prop your foot up on a pillow or cushion.
Posture and Foot Hygiene
Maintaining good posture and proper foot hygiene can prevent and alleviate heel pain. Poor posture can strain the muscles and ligaments in the foot and ankle, while poor hygiene can increase the risk of infections.
- Posture: Maintaining good posture while standing and walking can help distribute weight evenly across your feet. This reduces stress on the heels and prevents strain on the muscles and ligaments. Pay attention to your posture, especially when standing for prolonged periods.
- Foot Hygiene: Keeping your feet clean and dry can prevent fungal infections and other foot problems that can contribute to heel pain. Wash your feet regularly and dry them thoroughly, especially between the toes. Use clean socks and shoes to maintain good foot hygiene.
Over-the-Counter Pain Relievers
Over-the-counter pain relievers, such as ibuprofen or naproxen, can help manage pain and inflammation associated with heel pain. However, it is essential to use them responsibly and be aware of potential side effects.
- Common Over-the-Counter Pain Relievers: Ibuprofen (Advil, Motrin) and naproxen (Aleve) are common choices. Always follow the dosage instructions on the label. Aspirin is another option, but it can increase the risk of stomach bleeding.
- Potential Side Effects: Over-the-counter pain relievers can cause side effects such as stomach upset, nausea, and allergic reactions. If you experience any unusual symptoms, stop taking the medication and consult a doctor.
When to Seek Professional Help
Heel pain can range from a minor annoyance to a debilitating condition. Understanding when to seek professional help is crucial for effective treatment and preventing the pain from worsening. Ignoring persistent or severe heel pain can lead to long-term problems and hinder your ability to perform daily activities.Knowing the specific situations where professional medical attention is necessary empowers you to take proactive steps toward healing and restoring your mobility.
This section Artikels the critical factors that signal a need to consult a healthcare provider for your heel pain.
Signs of Serious Underlying Conditions
Heel pain isn’t always just a simple strain or overuse injury. Sometimes, it can be a symptom of a more serious underlying condition. Prompt diagnosis and treatment are essential in these cases to prevent complications.
- Severe pain that significantly limits your ability to walk or bear weight on your heel. This pain should not be relieved with rest or over-the-counter pain medications.
- Swelling or redness around the heel that increases over time, accompanied by pain.
- A noticeable change in the shape or appearance of your heel, such as a lump or deformity.
- Numbness or tingling in the heel or foot, which can be indicative of nerve damage.
- A history of diabetes or other conditions that affect blood circulation. Individuals with these conditions are at higher risk for complications related to heel pain.
Persistent Pain
Persistent heel pain, even with self-care measures, warrants a doctor’s evaluation. While some pain is expected with overuse or minor injuries, persistent pain that doesn’t improve or worsens over time needs attention.
- Pain that lasts longer than a few weeks, despite rest and home remedies.
- Pain that significantly interferes with daily activities, such as walking, standing, or participating in sports.
- Pain that awakens you at night or makes it difficult to sleep.
Limited Mobility
If your heel pain restricts your ability to move or bear weight, it’s essential to seek professional help. Inability to perform everyday tasks or participate in activities that were once routine signals a need for proper diagnosis and treatment.
- Difficulty putting weight on your heel or foot.
- Inability to walk normally or cover distances without experiencing significant pain.
- Significant limitation in your range of motion in the affected area.
Symptoms Requiring Immediate Medical Attention
Certain symptoms associated with heel pain demand immediate medical attention. These include signs that might indicate a more serious problem or a medical emergency.
- Sudden, severe pain in the heel, especially if accompanied by fever, chills, or redness.
- Significant swelling in the foot or ankle that rapidly increases in size.
- Visible deformity or change in the shape of the heel or foot.
- Signs of infection, such as pus or drainage from the affected area.
- Numbness or tingling in the foot or leg that spreads upwards.
Epilogue
In conclusion, heel pain when walking can stem from a variety of factors, and proper diagnosis and treatment are crucial. This guide offers insights into the causes, diagnostic methods, and treatment options available. Remember, prevention plays a vital role in maintaining healthy feet. By understanding the risk factors and implementing preventative measures, you can significantly reduce your chances of experiencing this common ailment.




