Gonorrhea symptoms after treatment can be tricky. While treatment often clears the infection, some people experience lingering or new symptoms. This post delves into the potential symptoms that might appear after treatment, explores the reasons behind them, and guides you on when to seek medical help. Understanding these possibilities is key to managing your well-being after treatment.
This comprehensive guide will walk you through potential post-treatment symptoms, their possible causes, and how to interpret them. We’ll cover everything from common misconceptions to strategies for managing discomfort and when to seek immediate medical attention.
Overview of Gonorrhea Symptoms

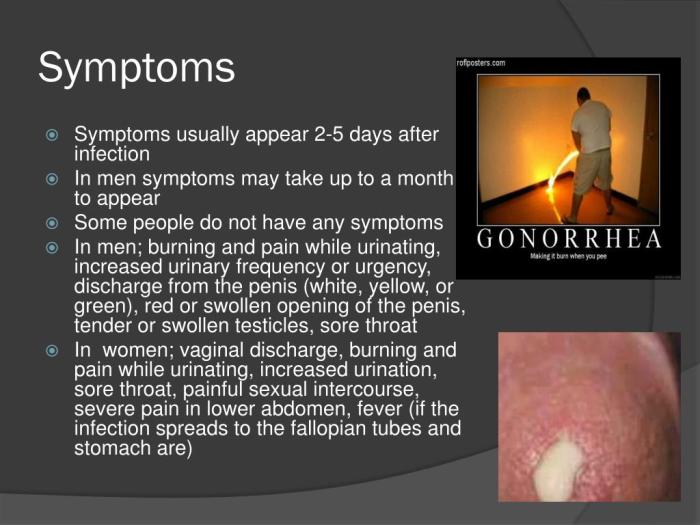
Gonorrhea, a sexually transmitted infection (STI), is caused by the bacteriumNeisseria gonorrhoeae*. It can affect various parts of the body, including the genitals, rectum, and throat. Understanding the symptoms, especially before treatment, is crucial for prompt diagnosis and effective management. Early intervention significantly improves treatment outcomes and reduces the risk of complications.Typical symptoms of gonorrhea, before treatment, can vary significantly in their presentation and severity.
Some individuals may experience noticeable symptoms, while others may be asymptomatic carriers, potentially unknowingly spreading the infection. This makes regular STI testing essential for individuals who are sexually active.
Symptoms Before Treatment
Gonorrhea symptoms, when present, often manifest within a few days or weeks after exposure. However, many individuals, particularly women, may experience no noticeable symptoms at all, making diagnosis challenging. This asymptomatic nature underscores the importance of regular STI screening.
- Genital Symptoms (Men): Men may experience a burning sensation during urination, pus-like discharge from the penis, and pain or swelling in the testicles. These symptoms often appear within a few days of infection. The discharge may vary in color, from clear to yellow or green.
- Genital Symptoms (Women): Women may experience a vaginal discharge, burning sensation during urination, and pain during sexual intercourse. Often, these symptoms are mild or similar to other vaginal conditions, making diagnosis more difficult. Pelvic inflammatory disease (PID), a serious complication of untreated gonorrhea, can result in severe abdominal pain and infertility in women.
- Rectal Symptoms: Rectal infection can lead to pain, discharge, and bleeding from the rectum. Similar to genital infections, symptoms may not be immediately apparent.
- Throat Symptoms: Oral sex can transmit gonorrhea to the throat. Sore throat is a common symptom, but many individuals may not experience any discomfort.
Common Misconceptions
Several misconceptions surround gonorrhea symptoms, often hindering early diagnosis and treatment. It’s crucial to dispel these myths and promote accurate understanding.
- Gonorrhea only affects the genitals: While genital infection is common, gonorrhea can also infect the rectum and throat. This highlights the importance of comprehensive sexual health awareness.
- Symptoms are always severe: The severity of symptoms varies greatly between individuals. Some individuals experience no symptoms at all, while others have noticeable discomfort.
- Gonorrhea symptoms disappear on their own: Untreated gonorrhea can lead to serious health complications. Symptoms should not be ignored, and prompt medical attention is crucial.
Comparison of Gonorrhea Symptoms Before and After Treatment
| Symptom | Before Treatment | After Treatment | Possible Explanation |
|---|---|---|---|
| Genital Discharge | Pus-like, yellowish-green | Reduced or absent | Antibiotics effectively kill the bacteria causing the discharge. |
| Painful Urination | Burning or stinging | Subsided | Reduction in bacterial irritation and inflammation. |
| Rectal Pain | Pain, discomfort, bleeding | Reduced or resolved | Antibiotic treatment eliminates the bacteria causing the inflammation. |
| Sore Throat | Pain, scratchiness | Resolved | Elimination of bacteria from the throat. |
| Vaginal Discharge | Unusual discharge | Normal | Antibiotics kill the bacteria causing the abnormal discharge. |
Potential Symptoms After Treatment
Gonorrhea treatment, while often effective, doesn’t always eliminate all symptoms. Some individuals may experience lingering or new symptoms following treatment. Understanding these potential issues is crucial for both self-management and seeking timely medical attention. This section will delve into possible post-treatment symptoms, their potential causes, and associated complications.Persistent or emerging symptoms after treatment can stem from various factors, including incomplete treatment, antibiotic resistance, or the presence of co-infections.
A thorough understanding of these possibilities is essential for appropriate follow-up care and preventing potential complications.
Possible Reasons for Persistent Symptoms
Incomplete treatment, a common reason for persistent symptoms, occurs when the infection isn’t fully eradicated by the prescribed medication. This may happen due to missed doses, incorrect dosage, or the presence of antibiotic resistance. Antibiotic resistance, where the bacteria causing gonorrhea have adapted to resist the treatment, poses a significant challenge to effective therapy. In such cases, a different antibiotic regimen may be necessary.
Co-infections, such as chlamydia, can also contribute to persistent symptoms. The presence of other sexually transmitted infections can mask the true nature of the gonorrhea infection, leading to a delayed or inaccurate diagnosis. It’s important to note that gonorrhea can sometimes manifest in different ways depending on the individual, so symptoms might be less noticeable than expected.
So, you’ve finished your gonorrhea treatment, but still feeling off? It’s totally normal to experience lingering symptoms, but sometimes those persistent aches and pains could be connected to something else, like sleep apnea and oxygen desaturation. Sleep apnea and oxygen desaturation can cause a whole host of issues that mimic gonorrhea symptoms, making diagnosis tricky. Ultimately, if you’re still experiencing unusual symptoms after treatment, it’s always best to chat with your doctor to get to the bottom of things and rule out any other potential causes.
Potential Complications
Untreated or inadequately treated gonorrhea can lead to severe complications, including pelvic inflammatory disease (PID) in women, which can result in infertility or ectopic pregnancy. In men, it can lead to epididymitis, a painful inflammation of the epididymis, a tube that carries sperm. These complications can often occur even after treatment, though the risk is reduced with appropriate and timely treatment.
Therefore, consistent follow-up with a healthcare provider is crucial.
Differentiating Post-Treatment Symptoms
Post-treatment symptoms may differ from pre-treatment symptoms in several ways. For instance, the intensity of symptoms might diminish or disappear during treatment but reappear afterward. This can be confusing, but the important thing is to report any new or persistent symptoms to a healthcare provider. The location and nature of symptoms can also change. A burning sensation during urination might transition to pain in the testicles or lower abdomen, or a discharge might cease, then return.
Recognizing these shifts is key to timely intervention.
So, you’ve finished your gonorrhea treatment, and you’re feeling relieved. But, it’s crucial to remember that symptoms can sometimes linger even after treatment. If you’re experiencing persistent symptoms, it’s always a good idea to check in with your doctor. Considering potential health insurance changes, like special enrollment periods for employer sponsored health insurance , might be important if you want to ensure you have the right coverage for follow-up care.
Don’t hesitate to seek professional medical advice if you have any questions or concerns about your health.
Post-Treatment Symptom Table
| Symptom | Possible Cause | Duration | Treatment Options |
|---|---|---|---|
| Persistent pain in the testicles | Incomplete treatment, epididymitis, or other infections | Variable, depending on the underlying cause | Antibiotics, pain management, and potentially surgery |
| Recurring discharge | Incomplete treatment, antibiotic resistance, or co-infections | Variable, depending on the underlying cause | Different antibiotic regimens, tests for other STIs |
| Pelvic pain (in women) | Incomplete treatment, PID, or other underlying conditions | Variable, depending on the underlying cause | Antibiotics, pain management, and potential surgery |
| Fever | Possible infection or immune response | Usually short-lived (days) | Symptom management, antibiotics if infection confirmed |
Interpreting Symptoms Post-Treatment
Navigating the aftermath of gonorrhea treatment can be confusing. While most individuals experience a complete resolution of symptoms after successful treatment, some may still experience lingering or new symptoms. Understanding the factors influencing these post-treatment symptoms is crucial for accurate self-assessment and appropriate medical intervention.Interpreting post-treatment symptoms requires careful consideration of various factors, going beyond a simple “yes” or “no” answer.
It’s important to differentiate between lingering effects of the infection, potential side effects of treatment, and entirely unrelated health issues. This involves a thorough understanding of the infection’s typical progression, the specific treatment administered, and a comparison to the individual’s overall health status.
Factors to Consider When Assessing Post-Treatment Symptoms
Identifying the root cause of post-treatment symptoms hinges on a comprehensive evaluation. Several factors need careful consideration.
- Timing of symptoms: Did the symptoms appear immediately after treatment, or several days or weeks later? The timing can provide valuable clues. For example, symptoms appearing shortly after treatment might indicate a side effect of the medication, whereas symptoms appearing weeks later could be a lingering effect of the infection or an unrelated condition.
- Severity of symptoms: The intensity of the symptoms is important. Mild discomfort might be a side effect or a sign of a minor issue, while severe pain could signal a more serious problem. Severe pain requiring immediate medical attention should be reported without delay.
- Location of symptoms: The location of the symptoms can be a significant indicator. For example, persistent pain in the testicles or pelvic area could be a sign of complications related to gonorrhea or a different health issue.
- Prior medical history: Any pre-existing health conditions or other infections can impact the manifestation of post-treatment symptoms. For instance, individuals with a history of STIs or immune deficiencies might be more susceptible to lingering symptoms.
- Treatment details: Understanding the specific treatment regimen is essential. The type of antibiotics used and the dosage regimen will play a role in potential side effects. Differences in treatment methods might result in various reactions.
Seeking Medical Advice
Seeking medical advice is crucial in the face of persistent or new symptoms after gonorrhea treatment. A healthcare provider can perform a thorough evaluation, conduct necessary tests, and provide personalized guidance.
“Delaying medical attention for post-treatment symptoms can potentially worsen the condition or lead to complications.”
Distinguishing Post-Treatment Gonorrhea Symptoms from Other Conditions
Accurate diagnosis requires differentiating between post-treatment gonorrhea symptoms and other possible conditions.
- Other STIs: A thorough sexual health history and physical examination are critical to rule out the presence of other sexually transmitted infections. The symptoms of different STIs can overlap.
- Urinary tract infections (UTIs): Symptoms of a UTI, such as painful urination, can mimic some symptoms of gonorrhea. A urine test can differentiate between the two conditions.
- Pelvic inflammatory disease (PID): In women, persistent pelvic pain or unusual vaginal discharge could be indicative of PID, a potential complication of gonorrhea. A physical examination and appropriate tests are needed for a proper diagnosis.
When to Seek Immediate Medical Attention
Certain symptoms necessitate immediate medical attention.
- Severe pain or swelling in the genital area: This could indicate a serious complication requiring prompt medical intervention.
- High fever or chills: These symptoms could suggest a systemic infection or a more serious complication.
- Difficulty urinating: This can be a sign of a blockage or other serious condition requiring immediate medical care.
- Signs of sepsis: Symptoms such as rapid heart rate, shortness of breath, and confusion are signs of sepsis and require immediate emergency care.
Flowchart for Evaluating Post-Treatment Symptoms
The following flowchart provides a simplified guide for evaluating post-treatment symptoms. A healthcare professional should always be consulted for accurate diagnosis and treatment.
| Symptom | Action |
|---|---|
| Mild, localized discomfort | Schedule an appointment with a healthcare provider for evaluation. |
| Severe pain, fever, or difficulty urinating | Seek immediate medical attention at a hospital or urgent care facility. |
| Symptoms persisting after 2 weeks of treatment | Schedule an appointment with a healthcare provider for follow-up. |
Factors Influencing Symptom Persistence After Gonorrhea Treatment: Gonorrhea Symptoms After Treatment
Understanding why some individuals experience lingering symptoms after gonorrhea treatment is crucial for effective management and patient care. This persistence can stem from a variety of interconnected factors, including individual health conditions, treatment efficacy, and adherence to prescribed protocols. It’s important to remember that while persistent symptoms are possible, they don’t always indicate a failure of treatment. Many factors can influence the duration and severity of symptoms following treatment.
Individual Factors Affecting Symptom Duration
Individual variations in immune responses, overall health, and co-existing conditions can significantly impact symptom resolution. For example, individuals with weakened immune systems due to underlying conditions or those taking medications that suppress the immune system may experience prolonged or more severe symptoms. Similarly, concurrent infections or other medical issues can complicate the healing process and potentially prolong symptom duration.
Treatment Effectiveness and Symptom Resolution
The effectiveness of the gonorrhea treatment directly correlates with the likelihood of symptom resolution. Factors such as the specific antibiotic used, the dosage, and the duration of treatment all contribute to the treatment’s success. Antibiotics chosen must be effective against the specific strain of gonorrhea present in the patient. Treatment regimens may vary based on factors such as the patient’s age, overall health, and the presence of other medical conditions.
Adherence to Treatment Protocols
Adherence to the prescribed treatment protocol is paramount for successful symptom resolution. Incomplete treatment courses or missed doses can allow the bacteria to persist, potentially leading to recurrent infections and prolonged symptoms. This is particularly critical for the full duration of the prescribed medication. Understanding and communicating the importance of adhering to the treatment regimen with the patient is vital.
Importance of Completing the Full Course of Antibiotics
The complete course of antibiotics is essential to eliminate the gonorrhea bacteria and prevent potential complications. Skipping doses or stopping treatment prematurely can lead to the bacteria developing resistance to the antibiotic, making future infections more difficult to treat. This is why patient education about the necessity of completing the prescribed course is crucial.
Comparison of Different Treatment Regimens
Various treatment regimens are available for gonorrhea, each with its own potential impact on symptom resolution. Some regimens may be more effective than others, depending on the specific strain of gonorrhea and the individual patient’s response. Factors such as the patient’s tolerance of different antibiotics should also be considered when selecting a treatment plan.
Factors Affecting Symptom Resolution
| Factor | Explanation | Impact | Example |
|---|---|---|---|
| Individual Immune Response | Variation in the body’s ability to fight off infection. | Stronger immune systems tend to clear symptoms faster. | A person with a healthy immune system may see symptoms resolve within a week, while someone with a weakened immune system might experience symptoms for longer. |
| Treatment Efficacy | The ability of the chosen antibiotic to effectively kill the gonorrhea bacteria. | Effective treatment results in faster symptom resolution. | An antibiotic that’s effective against the specific gonorrhea strain will likely resolve symptoms quicker than an ineffective one. |
| Adherence to Treatment | Following the prescribed treatment plan completely. | Complete adherence leads to a higher chance of successful eradication of the bacteria and symptom resolution. | Missing doses or stopping treatment early can prolong symptoms and potentially lead to antibiotic resistance. |
| Co-existing Infections | Presence of other infections that may complicate healing and symptom resolution. | Co-existing infections can prolong symptom resolution. | Someone with both gonorrhea and chlamydia may experience lingering symptoms longer than someone with only gonorrhea. |
When to Seek Medical Help
Gonorrhea treatment is crucial, but understanding when to seek immediate medical attention is equally important. Knowing the signs of potential complications and the importance of follow-up appointments can prevent serious health issues. Prompt intervention, especially when symptoms worsen or persist after treatment, can significantly improve outcomes.Post-treatment, while many individuals experience a resolution of symptoms, some may continue to experience discomfort or new symptoms.
This section will Artikel situations requiring immediate medical attention, the actions to take, and the potential complications that can arise. Understanding these guidelines empowers individuals to take control of their health and seek appropriate care when needed.
Crucial Situations Requiring Immediate Medical Attention
Knowing when to seek immediate medical attention is critical for managing gonorrhea effectively. Prompt intervention can prevent complications and ensure proper treatment. Delaying care can lead to more severe health issues.
| Situation | Symptoms | Actions | Potential Complications |
|---|---|---|---|
| Severe Pain or Discomfort | Intense pelvic or testicular pain, severe burning during urination, or unusual vaginal discharge | Immediately contact a healthcare provider or go to the nearest emergency room. | Untreated gonorrhea can lead to pelvic inflammatory disease (PID) in women, potentially causing infertility or ectopic pregnancy. In men, it can lead to epididymitis, which can also affect fertility. |
| Symptoms Worsening After Treatment | If symptoms that were initially present return or worsen after starting treatment, or if new symptoms emerge. | Schedule a follow-up appointment with your healthcare provider immediately to discuss the change in symptoms. | This could indicate an infection that is resistant to the prescribed medication, requiring a different treatment approach. Or, it might indicate a secondary infection that needs to be addressed. |
| Presence of Fever and Chills | High fever, chills, or flu-like symptoms accompanying gonorrhea symptoms. | Seek immediate medical attention, as this may signal a systemic infection or a serious complication. | Sepsis, a life-threatening condition, is a potential complication of severe infections. |
| Signs of Infection Spreading | Pain radiating to other areas, swelling, redness, or pus discharge outside the typical infection sites. | Contact a healthcare provider or seek emergency medical care. | Disseminated gonococcal infection (DGI) is a rare but serious complication where the infection spreads through the bloodstream, affecting multiple organs. |
| New or Worsening Discharge | Increased volume, unusual color (green, yellow, or gray), or foul odor of discharge. | Contact your healthcare provider for evaluation and appropriate treatment. | Secondary infections or complications related to the initial gonorrhea infection could be present. |
Importance of Follow-up Appointments
Follow-up appointments are essential to ensure the treatment is effective and to monitor for any potential complications. A healthcare provider can assess if the infection has been cleared and that no complications have arisen. This aspect of care is crucial for preventing long-term health problems.Regular follow-up appointments allow healthcare providers to monitor treatment progress and identify any potential complications early.
This proactive approach significantly contributes to successful treatment and prevents future health issues.
Interpreting Symptoms Post-Treatment
Interpreting symptoms post-treatment requires careful consideration of the initial symptoms, the treatment regimen, and any changes observed. It is important to remember that not all symptoms will disappear immediately after treatment. Some individuals may experience lingering symptoms, while others may develop new symptoms. In these cases, seeking prompt medical attention is vital.Understanding the possibility of lingering symptoms or the emergence of new ones after treatment is crucial.
By carefully tracking any changes and promptly reporting them to a healthcare provider, individuals can ensure timely interventions and effective management of potential complications.
Misinterpreting Symptoms Post-Treatment
Sometimes, the road to recovery from gonorrhea feels like a maze, especially when symptoms persist or new ones emerge after treatment. This can lead to feelings of uncertainty and anxiety, making it challenging to distinguish genuine lingering health concerns from the mental overlay of worry. It’s crucial to understand how our minds can influence our perception of symptoms, so we can better navigate this process and seek appropriate help.Misinterpreting post-treatment symptoms is common, and often stems from a combination of factors.
So, you’ve finished your gonorrhea treatment, but are still experiencing some symptoms? It can be frustrating, and sometimes, it’s just a lingering issue. While I’m no medical professional, I’ve heard that sometimes, similar to nausea-related migraine symptoms, it’s just part of the healing process. For those experiencing migraines and seeking effective therapies, exploring options like compazine for migraine therapy might be helpful.
Regardless, it’s always best to follow up with your doctor to ensure everything is okay and to rule out any other underlying issues, especially if the symptoms persist after treatment.
Anxiety, stress, and even the fear of a recurrence can dramatically alter how we experience physical sensations. This isn’t a sign of weakness, but a normal response to uncertainty. Recognizing these psychological influences is key to accurate self-assessment and informed decision-making.
Common Misinterpretations of Post-Treatment Symptoms
Many individuals experience a range of symptoms after gonorrhea treatment, some of which may be entirely unrelated to the infection. This can lead to misinterpreting harmless bodily sensations as serious health problems. It’s important to remember that while some lingering discomfort is possible, not all sensations indicate a relapse or ongoing infection.
Potential Psychological Factors Affecting Symptom Perception
Anxiety and stress are powerful forces in shaping our experience of physical sensations. When we’re anxious about our health, we tend to scrutinize our bodies more intensely. A slight ache, a subtle change in discharge, or a fleeting discomfort can quickly escalate into a perceived medical emergency. This heightened awareness, coupled with stress, can intensify the perceived severity of symptoms.
Furthermore, the fear of reinfection can exacerbate anxiety and contribute to the misinterpretation of benign sensations. For example, a person who experienced a difficult or prolonged infection might be more susceptible to perceiving subtle changes as signs of a return.
How Anxiety and Stress Affect Symptom Experience
Anxiety and stress can alter the body’s physiological responses. These changes can include increased heart rate, muscle tension, and heightened sensitivity to pain. These physiological changes can make symptoms feel more pronounced and distressing than they actually are. An individual experiencing high levels of anxiety might perceive a mild headache as a debilitating migraine, or a slight discomfort in the groin area as a serious relapse.
The brain’s heightened awareness during periods of stress can create a vicious cycle, where perceived symptoms amplify anxiety, and anxiety intensifies the perceived symptoms.
Examples of How Psychological Factors Influence Symptom Perception
A patient who recently experienced a painful gonorrhea infection might be more sensitive to any subsequent discomfort. A slight twinge in the pelvic area could be misinterpreted as a return of the infection, even if it’s unrelated. Similarly, someone experiencing financial stress or relationship problems might perceive any bodily sensations as a reflection of their anxieties, leading to heightened symptom awareness.
These heightened perceptions can lead to unnecessary medical consultations and potentially delay the appropriate treatment for underlying psychological issues.
Table of Common Misinterpretations and Their Potential Causes
| Misinterpretation | Cause | Potential Outcome | Mitigation Strategy |
|---|---|---|---|
| Feeling a persistent burning sensation in the urethra after treatment | Anxiety, heightened sensitivity to normal bodily functions, or undiagnosed urinary tract infection | Unnecessary medical procedures, continued worry, potential delay in addressing other stressors | Keep a symptom diary, communicate concerns with a trusted medical professional, address underlying stressors with therapy or support groups |
| Experiencing recurring discharge after treatment | Stress, anxiety, or an unrelated infection (e.g., yeast infection) | Repeated doctor visits, unnecessary antibiotic use, and continued distress | Discuss with a healthcare provider to rule out other infections, practice relaxation techniques, and manage anxiety |
| Feeling persistent pain in the testicles or ovaries after treatment | Anxiety, stress, or lingering inflammation | Unnecessary tests, surgeries, and feelings of hopelessness | Maintain open communication with a trusted healthcare provider, engage in stress-reduction activities |
Managing Post-Treatment Symptoms
Dealing with gonorrhea and its aftermath can be emotionally and physically challenging. While treatment effectively addresses the infection, some individuals may experience lingering symptoms. This section focuses on practical strategies to manage these symptoms and promote overall well-being during this process.Understanding that symptom persistence after treatment isn’t uncommon, it’s crucial to adopt a proactive approach to self-care. This includes focusing on healthy lifestyle choices, managing discomfort, and seeking support when needed.
By incorporating these strategies, individuals can navigate this period with greater ease and confidence.
Self-Care Strategies for Symptom Management
Managing post-treatment symptoms requires a multi-faceted approach. Addressing physical discomfort, emotional well-being, and lifestyle choices all play a vital role in recovery. The following strategies provide practical steps to support your journey.
| Strategy | Description | Benefits | Implementation |
|---|---|---|---|
| Rest and Relaxation | Prioritize adequate sleep and incorporate relaxation techniques like deep breathing, meditation, or gentle stretching. | Reduces stress, promotes physical healing, and improves overall well-being. | Aim for 7-9 hours of quality sleep each night. Practice deep breathing exercises for 10-15 minutes daily. Consider a calming bedtime routine. |
| Hydration | Drink plenty of fluids, especially water, to maintain proper bodily functions and aid in flushing out toxins. | Supports overall bodily functions, reduces inflammation, and helps maintain hydration. | Carry a reusable water bottle and sip water throughout the day. Avoid sugary drinks. |
| Nutritious Diet | Consume a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Avoid processed foods, excessive sugar, and unhealthy fats. | Provides essential nutrients for healing, boosts the immune system, and promotes overall health. | Focus on whole foods. Include a variety of colorful fruits and vegetables. Choose lean protein sources like fish, poultry, or beans. |
| Gentle Exercise | Engage in light, regular exercise like walking, swimming, or yoga to promote blood circulation and reduce stress. | Improves mood, reduces muscle tension, and boosts energy levels. Exercise can also help manage stress and anxiety. | Start with 15-20 minutes of low-impact exercise most days of the week. Listen to your body and adjust the intensity as needed. |
| Stress Management Techniques | Practice stress-reducing techniques like mindfulness, progressive muscle relaxation, or journaling. | Reduces stress hormones, improves emotional regulation, and promotes mental well-being. | Allocate dedicated time for stress-reducing activities. Try mindfulness meditation apps or guided relaxation exercises. |
| Seek Support | Connect with friends, family, or support groups to share experiences and receive emotional support. | Provides emotional support, reduces feelings of isolation, and offers a sense of community. | Reach out to trusted friends or family. Consider joining online or in-person support groups. |
Managing Discomfort and Pain
Discomfort, including pain or tenderness, can be a common experience after gonorrhea treatment. Managing this involves using appropriate pain relief measures and understanding potential contributing factors.Applying a warm compress to the affected area, and over-the-counter pain relievers like ibuprofen, can help alleviate discomfort. However, it’s important to consult a healthcare professional if pain persists or worsens significantly.
Importance of a Healthy Lifestyle
A healthy lifestyle, including proper nutrition, regular exercise, and adequate sleep, plays a crucial role in the body’s ability to heal and recover from infections. A well-nourished body is better equipped to combat any lingering symptoms and promote overall well-being.
Stress Reduction Strategies
Stress can exacerbate physical and emotional symptoms. Implementing stress reduction techniques can be a powerful tool in managing the recovery process. Mindfulness exercises, deep breathing techniques, and engaging in enjoyable activities can significantly reduce stress levels.
Resources for Support and Guidance, Gonorrhea symptoms after treatment
Numerous resources are available to provide guidance and support during the recovery process. Healthcare providers, support groups, and online communities can offer valuable information and encouragement. Remember that you are not alone in this process.
Concluding Remarks
In summary, gonorrhea symptoms after treatment can vary greatly. It’s crucial to understand that lingering or new symptoms aren’t always a sign of the infection returning. This article has explored potential reasons for these symptoms, offering insights into factors that influence resolution and when professional medical advice is essential. Remember, open communication with your healthcare provider is vital for a successful recovery.




