Drugs for cholesterol and triglycerides are a crucial part of managing cardiovascular health. This guide delves into the science behind these medications, exploring their mechanisms of action, potential side effects, and the importance of lifestyle modifications. We’ll examine the different types of drugs available, their effectiveness, and how healthcare professionals determine the best treatment plan for individual patients.
Understanding cholesterol and triglycerides, and how drugs impact them, empowers individuals to make informed decisions about their health. The information presented here aims to equip readers with a solid foundation of knowledge on this critical topic.
Overview of Cholesterol and Triglycerides
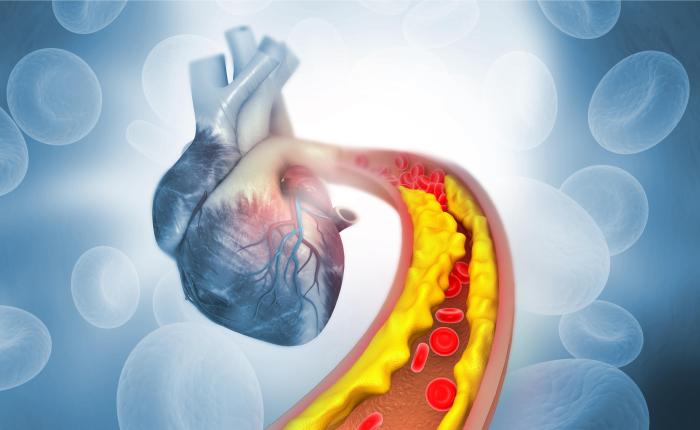
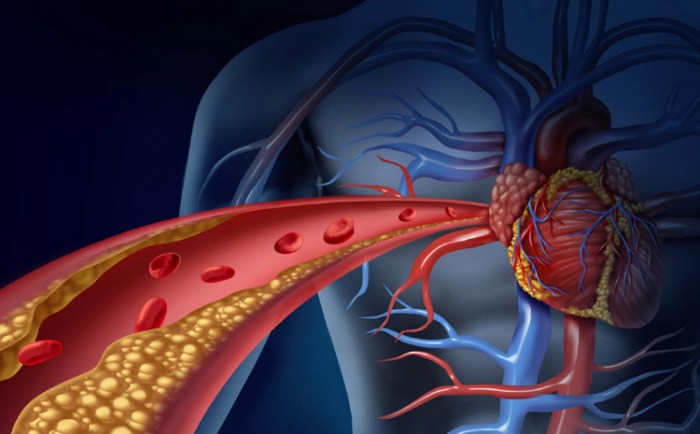
Understanding cholesterol and triglycerides is crucial for maintaining cardiovascular health. These fats, while essential for bodily functions, can become problematic when their levels in the blood become elevated. High levels can contribute to the buildup of plaque in arteries, increasing the risk of heart disease and stroke. This overview will clarify the roles of cholesterol and triglycerides, distinguishing between healthy and unhealthy levels, and explaining the importance of maintaining a balance.
Cholesterol and Triglycerides: Essential Fats
Cholesterol is a waxy, fat-like substance produced by the liver and also found in some foods. It’s vital for building cell membranes, producing hormones, and aiding in digestion. Triglycerides are another type of fat found in the blood, primarily derived from the diet. They serve as a body’s energy storage. Maintaining healthy levels of both cholesterol and triglycerides is paramount for overall health and minimizing cardiovascular risk.
HDL and LDL Cholesterol: A Critical Distinction
High-density lipoprotein (HDL) cholesterol is often referred to as “good” cholesterol. HDL helps remove excess cholesterol from the arteries, transporting it back to the liver for processing and elimination. Low-density lipoprotein (LDL) cholesterol, often called “bad” cholesterol, can accumulate in the arteries, contributing to plaque buildup. The balance between HDL and LDL is critical for cardiovascular health.
High LDL levels and low HDL levels are major risk factors for heart disease.
Triglycerides and Heart Disease Risk
Triglycerides, while not directly forming plaque, are significantly linked to heart disease risk. High triglyceride levels often occur alongside low HDL levels and high LDL levels, creating a dangerous combination that accelerates the buildup of plaque in the arteries. This can lead to narrowing of the arteries and reduced blood flow, potentially causing heart attacks or strokes. The interplay between these factors highlights the importance of maintaining a healthy lifestyle to regulate triglyceride levels.
Healthy Cholesterol and Triglyceride Levels
Maintaining healthy levels of cholesterol and triglycerides is crucial for preventing cardiovascular diseases. Elevated levels increase the risk of developing atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
| Category | Total Cholesterol (mg/dL) | LDL Cholesterol (mg/dL) | HDL Cholesterol (mg/dL) | Triglycerides (mg/dL) |
|---|---|---|---|---|
| Healthy | < 200 | < 100 | ≥ 40 (men), ≥ 50 (women) | < 150 |
| Borderline High | 200-239 | 100-129 | ≥ 40 (men), ≥ 50 (women) | 150-199 |
| High | ≥ 240 | ≥ 130 | < 40 (men), < 50 (women) | ≥ 200 |
Types of Drugs for Cholesterol and Triglycerides
High cholesterol and triglycerides can significantly impact cardiovascular health. Fortunately, various medications are available to manage these conditions effectively. These drugs work through different mechanisms, targeting specific aspects of cholesterol and triglyceride metabolism. Understanding these different classes of medications is crucial for patients and healthcare professionals to make informed decisions about treatment plans.
Statins
Statins are the most common class of cholesterol-lowering drugs. They inhibit the enzyme HMG-CoA reductase, a key enzyme in cholesterol synthesis within the liver. By reducing cholesterol production, statins lower LDL (“bad”) cholesterol levels, which is a major risk factor for heart disease.
- Statins effectively reduce LDL cholesterol levels, a crucial factor in cardiovascular health. Lowering LDL cholesterol is associated with a decrease in the risk of heart attacks and strokes. Examples include atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor).
Bile Acid Sequestrants
Bile acid sequestrants work by binding to bile acids in the digestive tract. This binding prevents the reabsorption of bile acids, leading to their excretion from the body. The liver, needing more bile acids, then uses cholesterol to produce more. This process results in a decrease in LDL cholesterol levels.
- Bile acid sequestrants are effective in reducing LDL cholesterol, contributing to a lower risk of heart disease. They can be used as an alternative or in conjunction with statins, especially in patients who cannot tolerate statins. Examples include cholestyramine (Questran), colestipol (Colestid), and colesevelam (Welchol).
Cholesterol Absorption Inhibitors
Cholesterol absorption inhibitors work by preventing the small intestine from absorbing cholesterol from the diet. By reducing cholesterol absorption, these drugs lower LDL cholesterol levels.
Managing cholesterol and triglycerides often involves medication. These conditions can be tricky, and sometimes require a combination of lifestyle changes and, yes, even prescription drugs. Understanding the difference between prescription and OTC drugs is key when choosing the right approach. For instance, some cholesterol-lowering drugs fall under prescription and OTC drugs categories. Ultimately, the best course of action for managing these blood fats is to consult a healthcare professional to determine the most suitable treatment plan for your specific needs.
- These drugs can be effective in lowering LDL cholesterol, particularly in patients with a high intake of dietary cholesterol. They can be used in combination with other medications like statins. A notable example is ezetimibe (Zetia).
Fibrates
Fibrates are primarily used to lower triglyceride levels. They activate an enzyme that increases the breakdown of triglycerides in the liver. They also help to raise HDL (“good”) cholesterol levels and reduce LDL cholesterol levels.
Managing cholesterol and triglycerides can be tricky, and sometimes medication is necessary. Understanding the potential side effects of these drugs is crucial. For example, some individuals experiencing elevated cholesterol might also find themselves facing joint issues like finger osteoarthritis, which requires careful management, as outlined in this informative article about finger osteoarthritis what you need to know.
Ultimately, a holistic approach that includes diet and lifestyle changes, alongside medication, is key to effectively managing both cholesterol and triglyceride levels.
- Fibrates are specifically effective in reducing triglyceride levels and raising HDL cholesterol, both crucial for cardiovascular health. Examples include fenofibrate (Tricor) and gemfibrozil (Lopid).
Nicotinic Acid (Niacin)
Nicotinic acid (niacin) is a B vitamin that can lower triglyceride and LDL cholesterol levels while increasing HDL cholesterol. Its mechanism of action is complex, involving several different pathways in the body.
- Nicotinic acid can be an effective treatment for high triglycerides and low HDL cholesterol, contributing to overall cardiovascular health. It may also have benefits in reducing the risk of cardiovascular disease. However, niacin can cause significant flushing, which can be a limiting factor in its use.
Table of Drug Classes for Cholesterol and Triglycerides
| Drug Class | Mechanism of Action | Common Side Effects |
|---|---|---|
| Statins | Inhibit HMG-CoA reductase, reducing cholesterol synthesis. | Muscle pain (myalgia), liver damage, elevated blood sugar |
| Bile Acid Sequestrants | Bind to bile acids, preventing their reabsorption, increasing cholesterol use by the liver. | Constipation, bloating, gas, decreased absorption of fat-soluble vitamins |
| Cholesterol Absorption Inhibitors | Prevent cholesterol absorption from the intestines. | Headache, diarrhea, muscle pain |
| Fibrates | Increase triglyceride breakdown and raise HDL cholesterol. | Muscle pain (myopathy), gallstones, elevated liver enzymes |
| Nicotinic Acid | Lower triglycerides and LDL cholesterol, increase HDL cholesterol. | Flushing, liver damage, elevated blood sugar |
How Drugs Work to Lower Cholesterol and Triglycerides
Understanding how cholesterol-lowering and triglyceride-reducing drugs work is crucial for managing these important blood lipids. These medications target specific pathways in the body, leading to reductions in harmful cholesterol and triglyceride levels, which in turn decrease the risk of cardiovascular disease.These drugs work through various mechanisms, primarily by affecting the liver’s role in producing and processing cholesterol and triglycerides.
By influencing the synthesis, absorption, and excretion of these lipids, they help achieve healthier lipid profiles, reducing the risk of atherosclerosis and associated health problems.
Different Mechanisms of Action
Various classes of drugs employ different strategies to lower cholesterol and triglycerides. These differences stem from the unique targets and pathways affected by each class.
- Statins: Statins are the most commonly prescribed cholesterol-lowering medications. They inhibit the enzyme HMG-CoA reductase, a key enzyme in cholesterol synthesis. By blocking this enzyme, statins reduce the production of cholesterol in the liver. This leads to a decrease in circulating cholesterol levels, and a concomitant increase in the number of LDL receptors on the liver surface, thus enhancing the uptake and removal of LDL cholesterol from the blood.
Examples include atorvastatin, simvastatin, and rosuvastatin.
- Bile Acid Sequestrants: These drugs bind to bile acids in the digestive tract, preventing their reabsorption. The liver, needing bile acids to produce bile, must use cholesterol to make more. This increased use of cholesterol for bile acid production leads to a reduction in circulating cholesterol levels. Examples include cholestyramine and colesevelam.
- Cholesterol Absorption Inhibitors: These medications, such as ezetimibe, block the absorption of cholesterol from the intestines. This reduces the amount of cholesterol entering the bloodstream, leading to a decrease in circulating cholesterol levels.
- Fibrates: Fibrates, like fenofibrate and gemfibrozil, primarily target triglyceride levels. They activate peroxisome proliferator-activated receptor alpha (PPARα) receptors, increasing the breakdown and removal of triglycerides from the blood. They also reduce the production of very-low-density lipoproteins (VLDL), the primary carriers of triglycerides in the blood. Importantly, fibrates can also affect HDL cholesterol, usually increasing it. This effect is beneficial, as HDL cholesterol is considered “good” cholesterol, and high levels are associated with reduced cardiovascular risk.
Comparative Effects of Drug Classes
The following table summarizes the specific targets and effects of different drug classes on cholesterol and triglycerides:
| Drug Class | Primary Target | Effect on Cholesterol (LDL, HDL, and Total) | Effect on Triglycerides |
|---|---|---|---|
| Statins | HMG-CoA reductase (cholesterol synthesis) | Significant LDL reduction, modest HDL increase, total cholesterol reduction | Moderate reduction |
| Bile Acid Sequestrants | Bile acid reabsorption | Significant LDL reduction, minimal effect on HDL, total cholesterol reduction | Moderate reduction |
| Cholesterol Absorption Inhibitors | Cholesterol absorption in intestines | Moderate LDL reduction, minimal effect on HDL, total cholesterol reduction | Minimal effect |
| Fibrates | PPARα (triglyceride breakdown), VLDL production | Minimal to modest LDL reduction, usually HDL increase | Significant reduction |
This table illustrates the diverse mechanisms by which drugs target cholesterol and triglyceride levels. The specific effects on different lipid types vary between drug classes. It’s crucial to remember that individual responses to these medications can differ, and a physician’s guidance is essential for personalized treatment plans.
Side Effects and Considerations: Drugs For Cholesterol And Triglycerides
Taking medication to manage cholesterol and triglycerides is a significant step in maintaining cardiovascular health. However, like any medication, these drugs can have potential side effects. Understanding these potential side effects and the importance of monitoring them is crucial for safe and effective treatment. Proper communication with your healthcare provider about any concerns is essential.
Potential Side Effects of Cholesterol-Lowering Drugs
Cholesterol-lowering medications, often called statins, can cause a range of side effects, though not everyone experiences them. The most common side effects are generally mild and temporary. It’s important to remember that individual responses to medication vary.
- Muscle pain (myalgia) and weakness (myopathy): This is a notable side effect, particularly with some statins. Mild muscle aches can occur, but more severe cases, including muscle damage (rhabdomyolysis), are rare. The risk is often higher with higher doses or in combination with other medications. Regular monitoring of muscle pain is important.
- Liver problems: Statins can sometimes affect liver function. Regular blood tests are usually conducted to monitor liver enzyme levels, ensuring the medication’s impact on the liver is within safe parameters. While serious liver damage is rare, it’s crucial to be aware of the potential for liver issues.
- Digestive issues: Some individuals experience digestive problems such as nausea, diarrhea, or constipation. These are usually mild and resolve with continued use or adjustment of the medication. If the issues persist, it’s important to discuss them with a healthcare professional.
- Increased blood sugar: In some cases, cholesterol-lowering drugs can slightly increase blood sugar levels. This is a crucial consideration for people with pre-existing diabetes or those at risk of developing diabetes.
Potential Side Effects of Triglyceride-Reducing Drugs
Specific triglyceride-lowering drugs have their own set of potential side effects. These can vary based on the type of medication.
- Gastrointestinal issues: These drugs can cause digestive upset, including nausea, vomiting, and abdominal pain. These side effects are typically mild and transient.
- Muscle pain (myopathy): Some triglyceride-reducing drugs can also lead to muscle pain, similar to statins. Careful monitoring is crucial, especially if other medications are also being taken.
- Increased risk of pancreatitis: In rare cases, certain triglyceride-lowering medications may increase the risk of pancreatitis, a potentially serious inflammation of the pancreas. This risk is generally low but should be considered.
Importance of Monitoring and Reporting
Regular check-ups and blood tests are essential when taking these medications. Your healthcare provider will monitor your response to the treatment and adjust the dosage if needed. Promptly reporting any unusual symptoms, such as muscle pain, unexplained fatigue, or digestive problems, to your healthcare provider is crucial for early intervention and preventing potential complications.
Drug Interactions, Drugs for cholesterol and triglycerides
Certain medications and supplements can interact with cholesterol and triglyceride-lowering drugs, potentially affecting their effectiveness or increasing the risk of side effects. It’s vital to inform your healthcare provider about all medications, supplements, and herbal remedies you are taking to avoid any negative interactions.
| Drug Class | Common Side Effects | Potential Severity |
|---|---|---|
| Statins | Muscle pain, liver problems, digestive issues | Mild to moderate, but rare serious cases |
| Fibrates | Gastrointestinal issues, muscle pain, increased risk of pancreatitis | Generally mild, but rare serious cases |
| Other drugs | (e.g., niacin, bile acid sequestrants) | Specific to the drug; consult healthcare provider |
“Always consult your doctor before starting any new medication, especially if you are already taking other medications.”
Lifestyle Modifications
Managing cholesterol and triglycerides effectively requires a multifaceted approach that combines medication with healthy lifestyle choices. Simply put, taking medication alone is not enough for long-term, optimal health. A commitment to lifestyle modifications is crucial for preventing future complications and improving overall well-being. These changes are not just about lowering cholesterol; they’re about fostering a healthier, more sustainable way of life.Lifestyle modifications play a vital role in the management of cholesterol and triglycerides.
They work synergistically with medications to achieve and maintain healthy levels. By adopting these changes, individuals can significantly reduce their risk of cardiovascular diseases and improve their overall health and quality of life.
Healthy Dietary Recommendations
A diet rich in fruits, vegetables, and whole grains is essential for managing cholesterol and triglycerides. Reducing saturated and trans fats is crucial for lowering LDL (“bad”) cholesterol levels. Choosing lean protein sources and incorporating healthy fats, like those found in avocados, nuts, and fatty fish, is also beneficial. Focusing on a balanced diet is key to long-term success.
- Prioritize whole, unprocessed foods:
- Limit saturated and trans fats:
- Increase soluble fiber intake:
- Choose lean protein sources:
Fruits, vegetables, whole grains, and lean proteins provide essential nutrients and fiber, which aid in cholesterol management. Examples include whole-wheat bread, brown rice, and various fruits and vegetables.
Saturated fats, found in red meat, full-fat dairy products, and some processed foods, raise LDL cholesterol. Trans fats, often found in processed snacks and baked goods, have a detrimental effect on cholesterol levels. Replacing these with healthier fats, such as those found in avocados and olive oil, is recommended.
Soluble fiber, found in oats, beans, and fruits, helps to bind cholesterol in the digestive tract, preventing its absorption into the bloodstream. Increasing soluble fiber intake is a crucial dietary change.
Taking drugs for cholesterol and triglycerides can be a game-changer for your health, but sometimes you might notice unexpected side effects. For instance, some individuals experience issues with their toenails, such as early stage toenail fungus, which can be a tricky issue to address. It’s crucial to talk to your doctor about any unusual symptoms to ensure the best possible outcome with your cholesterol and triglyceride medication.
Opt for lean meats, poultry without skin, fish, beans, and lentils to limit saturated fat intake. These options are more beneficial for cholesterol management.
Regular Exercise
Regular physical activity is essential for maintaining healthy cholesterol and triglyceride levels. Exercise helps to raise HDL (“good”) cholesterol, which helps remove LDL cholesterol from the bloodstream. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week. Consistency is key.
- Aerobic Exercise:
- Strength Training:
Activities like brisk walking, jogging, swimming, or cycling improve cardiovascular health and help raise HDL cholesterol. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
Incorporating strength training exercises, such as weightlifting or bodyweight exercises, helps build muscle mass and improve metabolism, further supporting cholesterol management. Aim for two or more days a week.
Stress Management
Chronic stress can negatively impact cholesterol and triglyceride levels. Effective stress management techniques, such as mindfulness, yoga, or meditation, can help reduce these impacts. Finding healthy ways to cope with stress is crucial for overall well-being and managing cholesterol.
- Mindfulness and Meditation:
- Yoga and Tai Chi:
- Other Relaxation Techniques:
Practicing mindfulness and meditation can help manage stress levels and improve overall well-being, potentially impacting cholesterol levels.
These practices combine physical postures, breathing techniques, and meditation, offering a holistic approach to stress reduction and improving overall health.
Techniques like deep breathing exercises, spending time in nature, or engaging in hobbies can also help manage stress and improve overall well-being, potentially contributing to better cholesterol management.
Summary Table
| Dietary Changes | Exercise Recommendations | Stress-Reduction Techniques |
|---|---|---|
| Prioritize whole, unprocessed foods. | Aerobic exercise (150 min/week moderate or 75 min/week vigorous). | Mindfulness and meditation |
| Limit saturated and trans fats. | Strength training (2+ days/week). | Yoga and Tai Chi |
| Increase soluble fiber intake. | Maintain a consistent exercise routine. | Other relaxation techniques (deep breathing, nature time). |
| Choose lean protein sources. |
Choosing the Right Treatment
Choosing the right treatment plan for high cholesterol and triglycerides is a crucial step in managing these conditions effectively. It’s not a one-size-fits-all approach; instead, healthcare professionals consider various factors to tailor a personalized strategy. Understanding these factors and the importance of patient input is key to achieving optimal outcomes.A successful treatment plan hinges on careful consideration of individual needs, not just the numbers on a blood test.
This involves a deep dive into a patient’s medical history, current health status, and lifestyle, alongside their specific goals and preferences. The ultimate goal is to not just lower cholesterol and triglycerides but to do so safely and sustainably, minimizing any potential side effects while improving overall well-being.
Factors Considered by Healthcare Professionals
Healthcare professionals meticulously analyze several factors when designing a treatment plan. These factors are interconnected and play a vital role in the effectiveness and safety of the chosen medication.
- Patient’s Medical History: A thorough review of past and present health conditions is essential. This includes any pre-existing medical issues like diabetes, kidney disease, or liver problems, as these can influence drug choices and dosages. Previous adverse reactions to medications are also significant.
- Current Health Status: The patient’s overall health and well-being are assessed, considering any current symptoms or limitations. Factors such as age, weight, and other health markers are also taken into account. This comprehensive evaluation allows for the selection of a treatment plan that aligns with the patient’s current physical capacity.
- Individual Needs and Preferences: Understanding the patient’s lifestyle, dietary habits, and preferences is vital. Are there any allergies or dietary restrictions? Are they willing to make lifestyle changes alongside medication? This personalized approach allows for better patient adherence to the treatment plan.
Patient Case Study Example
Consider a 55-year-old female patient, Sarah, with a history of high cholesterol, mild hypertension, and a family history of heart disease. Her current blood test shows total cholesterol of 250 mg/dL and triglycerides of 200 mg/dL. She reports a sedentary lifestyle and a preference for a high-fat diet.Possible treatment options for Sarah include:
- Lifestyle Modifications: This might involve dietary changes (reducing saturated and trans fats), increasing physical activity, and weight management. This approach is often the first line of defense and can be very effective when combined with medication.
- Statins: Given her family history and the moderate elevation in cholesterol, statins could be a suitable option. Different statins have varying potency and side effect profiles. The choice will depend on Sarah’s specific needs and tolerance.
- Other Lipid-Lowering Medications: If statins are not tolerated or insufficient, other lipid-lowering medications like bile acid sequestrants or fibrates could be considered. These medications work through different mechanisms and may be more appropriate for certain situations, such as when triglycerides are significantly elevated.
Importance of Regular Monitoring and Follow-Up
Regular monitoring and follow-up appointments are crucial for managing cholesterol and triglyceride levels. This allows for adjustments to the treatment plan as needed.
- Regular Blood Tests: Monitoring blood cholesterol and triglyceride levels at scheduled intervals is essential to assess the effectiveness of the treatment. These tests provide critical data to make necessary adjustments to the medication or lifestyle changes.
- Physician Communication: Open communication with the healthcare provider is essential for reporting any side effects or concerns related to the treatment. This feedback loop allows for timely adjustments to the treatment plan, ensuring patient safety and efficacy.
- Lifestyle Adjustments: Ongoing support and guidance from the healthcare team can help patients maintain or adopt healthier lifestyle choices, promoting long-term success in managing cholesterol and triglycerides.
Patient Education
Taking charge of your cholesterol and triglyceride levels is a journey, not a race. This section focuses on empowering you with the knowledge and tools to effectively manage your health and understand your treatment plan. Understanding your medication, potential side effects, and the importance of adherence will be key to achieving your health goals.
Understanding Your Medications
Medication adherence is crucial for successful treatment. Taking your prescribed medications as directed by your doctor is vital for controlling cholesterol and triglyceride levels. Knowing how your medications work, potential side effects, and when to contact your doctor is essential. The information provided here is for educational purposes only and should not be considered medical advice. Always consult with your healthcare provider for personalized guidance.
Recognizing Potential Side Effects
Every medication carries potential side effects, and cholesterol and triglyceride medications are no exception. Common side effects can range from mild discomfort to more serious reactions. Be vigilant about any unusual symptoms and promptly report them to your doctor. Early detection and management of side effects can prevent complications and ensure your treatment remains effective.
Importance of Adherence to the Treatment Plan
Consistency is key to managing cholesterol and triglycerides effectively. Adherence to your prescribed treatment plan, including medication, diet, and lifestyle modifications, is paramount. A consistent approach ensures that your body responds favorably to the treatment and maintains healthy levels over time. Sticking to your plan, with support from your healthcare team, is critical for long-term health.
Key Points for Patient Education
| Topic | Explanation | Potential Questions & Answers |
|---|---|---|
| Understanding Medications | Knowing how your medications work, potential side effects, and dosage instructions is essential. | “How does this medication work?” “What are the common side effects?” “What should I do if I miss a dose?” |
| Side Effects | Be aware of possible side effects and promptly report any unusual symptoms to your doctor. | “What are the serious side effects I should be concerned about?” “How do I know if a side effect is serious?” “When should I contact my doctor?” |
| Adherence | Consistent adherence to your treatment plan, including medication, diet, and lifestyle changes, is vital. | “How can I make sure I take my medication consistently?” “What are some strategies to support adherence?” “How can I stay motivated to follow my treatment plan?” |
| Lifestyle Modifications | Incorporating healthy lifestyle choices, like a balanced diet and regular exercise, is important in managing cholesterol and triglycerides. | “What are some healthy eating habits to adopt?” “How much exercise do I need?” “What are some ways to manage stress?” |
Future Directions in Treatment
The current landscape of cholesterol and triglyceride management is constantly evolving, driven by ongoing research and a deeper understanding of these complex lipid disorders. This evolution promises to lead to more targeted and effective treatments, potentially minimizing side effects and maximizing patient outcomes. Advancements in drug development are paving the way for new therapies with enhanced efficacy and safety profiles.This exploration into future directions will highlight promising areas of research, potential breakthroughs, and the emergence of innovative drug targets.
We will delve into the strategies being employed to create safer and more effective treatments for cholesterol and triglyceride disorders.
Potential Advancements in Drug Therapies
Several exciting avenues are being pursued to improve upon existing cholesterol and triglyceride-lowering medications. Researchers are working on developing drugs with enhanced efficacy, reduced side effects, and tailored treatment options for diverse patient populations. The ultimate goal is to optimize treatment plans, making them more accessible and effective for a broader range of patients.
Novel Drug Targets
Researchers are investigating new drug targets beyond the traditional HMG-CoA reductase inhibitors (statins). These efforts are driven by the desire to address the limitations of current therapies and explore alternative pathways involved in lipid metabolism. The potential for targeting specific proteins and enzymes involved in cholesterol and triglyceride synthesis, absorption, and transport holds significant promise for developing more precise and personalized treatments.
This includes exploring targets in the liver, intestines, and other organs involved in lipid processing.
Personalized Medicine Approaches
The concept of personalized medicine is gaining traction in the field of lipid management. Researchers are increasingly recognizing the importance of considering individual patient factors such as genetics, lifestyle, and comorbidities when selecting treatment strategies. The development of genetic tests and biomarkers that predict treatment response and potential side effects will enable doctors to tailor therapy to each patient’s unique needs, leading to more effective and safe outcomes.
This approach promises to minimize adverse effects and maximize treatment efficacy, leading to improved long-term health for individuals with elevated cholesterol and triglycerides.
Research on Combination Therapies
Combining different lipid-lowering medications could potentially lead to greater efficacy and reduced side effects compared to monotherapy. Researchers are exploring the synergistic effects of combining existing drugs or developing novel combinations that target multiple pathways in lipid metabolism. For example, a combination therapy could simultaneously reduce cholesterol synthesis, enhance excretion, and improve triglyceride clearance. This could result in a more potent and comprehensive approach to managing lipid disorders.
A comprehensive understanding of the interplay between various lipid-lowering drugs is crucial for the development of these combination therapies.
Advances in Delivery Systems
Scientists are exploring innovative drug delivery systems to improve treatment adherence and reduce side effects. For instance, the development of long-acting formulations or targeted delivery systems that release medication directly to the liver could potentially reduce the frequency of dosing, making treatments more convenient and improving patient compliance. These improvements can translate to better patient outcomes and a more positive experience with treatment.
Last Recap
In conclusion, managing cholesterol and triglycerides effectively often requires a combination of medication and lifestyle adjustments. This comprehensive guide has highlighted the various drug classes, their mechanisms, and potential side effects. Crucially, it emphasizes the importance of patient education and ongoing monitoring to ensure optimal outcomes. Remember, always consult with a healthcare professional for personalized advice.




