Diverticulitis vs ulcerative colitis: understanding these two conditions is crucial for effective management. This in-depth look examines the key differences, symptoms, diagnostic procedures, and treatment approaches for each. We’ll explore the anatomical locations affected, the symptoms, and the diagnostic tools used to differentiate between them. This comparison will equip you with the knowledge to better understand these inflammatory bowel diseases.
The discussion will cover the typical symptoms, locations of inflammation, and common diagnostic procedures like colonoscopies and CT scans. We’ll also explore the various treatment options, including medications and potential surgical interventions. Ultimately, this comparison will offer a comprehensive understanding of the differences between diverticulitis and ulcerative colitis, empowering individuals and their healthcare providers to make informed decisions.
Introduction to Diverticulitis and Ulcerative Colitis
Diverticulitis and ulcerative colitis are both inflammatory conditions affecting the digestive system, specifically the large intestine (colon). While both can cause significant discomfort and require medical attention, they differ in their underlying causes, anatomical locations of inflammation, and typical symptoms. Understanding these differences is crucial for proper diagnosis and treatment.These conditions involve inflammation within the gastrointestinal tract, leading to a range of symptoms.
While both can affect quality of life, the location and nature of the inflammation determine the specific symptoms experienced. Recognizing the key differences in these conditions can lead to earlier and more effective medical intervention.
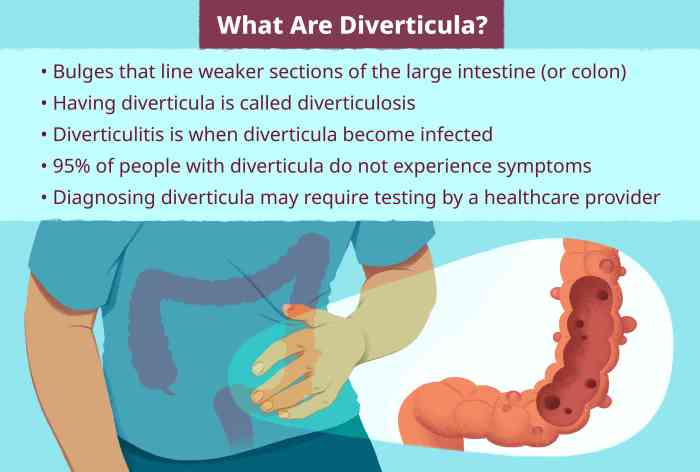
Key Characteristics of Diverticulitis
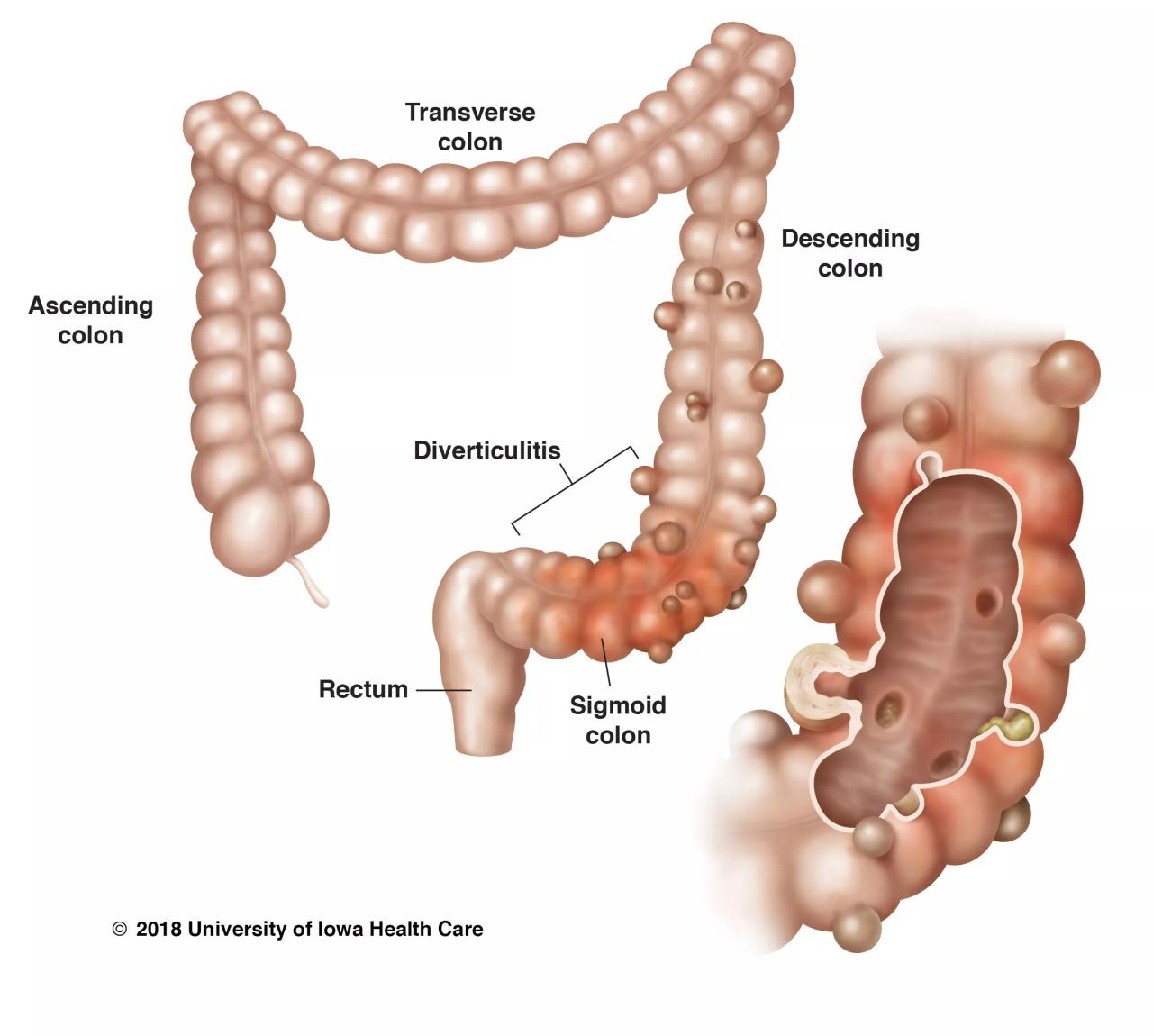
Diverticulitis is characterized by inflammation of small, bulging pouches (diverticula) that develop in the lining of the colon wall. These pouches are most commonly found in the sigmoid colon, the lower part of the colon. The exact cause of diverticula formation isn’t fully understood, but factors like low-fiber diets and increased pressure within the colon are thought to play a role.
Symptoms and Signs of Diverticulitis
Symptoms of diverticulitis can vary, but common signs include abdominal pain, often localized in the lower left quadrant, fever, nausea, vomiting, and changes in bowel habits, such as constipation or diarrhea. The severity of symptoms can range from mild to severe, with some individuals experiencing significant complications. The intensity and duration of symptoms can vary greatly, and the specific symptoms a person experiences can differ.
Key Characteristics of Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease (IBD) that involves inflammation of the lining of the colon and rectum. Unlike diverticulitis, which affects the colon wall, ulcerative colitis primarily targets the innermost layer of the colon and rectum. This inflammation can cause ulcers and sores, leading to bleeding and discomfort. The cause of ulcerative colitis remains unknown, but genetics and environmental factors are thought to play a significant role.
Symptoms and Signs of Ulcerative Colitis
Symptoms of ulcerative colitis are often similar to those of diverticulitis, including abdominal pain, but the location of the pain might be different. Frequent diarrhea, often with blood and mucus, is a hallmark symptom. The frequency and severity of bowel movements can vary considerably, and individuals may also experience fatigue, weight loss, and fever. Symptoms can range from mild to severe, and the severity and duration of symptoms can fluctuate.
Anatomical Differences and Affected Locations
The table below summarizes the key anatomical differences in the locations of inflammation for diverticulitis and ulcerative colitis.
| Condition | Location | Description |
|---|---|---|
| Diverticulitis | Colon (typically sigmoid colon) | Inflammation of small pouches (diverticula) in the colon wall. |
| Ulcerative Colitis | Colon and rectum | Inflammation of the lining of the colon and rectum. |
Understanding these distinctions is critical for accurate diagnosis and effective treatment strategies. The location of the inflammation is key to distinguishing between these two conditions.
Diagnostic Procedures
Differentiating diverticulitis from ulcerative colitis often relies on a combination of diagnostic tools. A thorough medical history, physical examination, and appropriate testing are crucial to pinpoint the correct diagnosis and initiate the most effective treatment plan. These procedures help identify the location, extent, and severity of the disease, enabling physicians to tailor interventions to individual patient needs.Understanding the nuances of these diseases and the various diagnostic techniques employed can empower individuals to advocate for their health and make informed decisions with their healthcare providers.
Colonoscopy and Biopsies
Colonoscopy is a vital procedure for evaluating the large intestine. A flexible tube with a camera is inserted through the rectum and into the colon, allowing visualization of the entire colon’s lining. This allows physicians to identify abnormalities like inflamed tissue, ulcers, or diverticula. Biopsies, small tissue samples taken during the colonoscopy, are crucial for confirming the diagnosis.
Microscopic examination of these samples can reveal specific characteristics of inflammation, aiding in the distinction between diverticulitis and ulcerative colitis. The presence of specific inflammatory cells or ulcer patterns can be indicative of either condition. The information gathered from biopsies complements the visual assessment during the colonoscopy, providing a more definitive diagnosis.
Imaging Techniques
Imaging plays a significant role in the diagnostic process, particularly when evaluating potential complications. CT scans, in particular, offer cross-sectional views of the abdomen, allowing visualization of the colon and surrounding structures. A CT scan can reveal the presence of abscesses, thickened bowel walls, or perforations, which are often associated with diverticulitis. X-rays, while less detailed than CT scans, can still identify some abnormalities in the digestive tract.
These tests can help confirm the presence of inflammation, narrowed areas, or other signs of diverticular disease or inflammatory bowel disease. In cases where diverticulitis is suspected, CT scans are frequently employed to identify complications like abscess formation.
Ever wondered about the differences between diverticulitis and ulcerative colitis? It’s a tricky area, but understanding the underlying issues is key. While researching these digestive conditions, I stumbled upon some fascinating information about PFAS in drinking water. PFAS in drinking water could potentially play a role in the development of inflammatory bowel diseases, and it’s a crucial factor to consider when trying to distinguish between diverticulitis and ulcerative colitis.
Ultimately, more research is needed to fully grasp the intricate relationship between environmental factors and these digestive conditions.
Diagnostic Procedures Table
| Procedure | Indications | Potential Findings in Diverticulitis | Potential Findings in Ulcerative Colitis |
|---|---|---|---|
| Colonoscopy | Suspected inflammatory bowel disease, evaluation of lower GI tract | Diverticula (small pouches), localized inflammation, signs of infection (abscesses) | Inflammation of the colonic lining (mucosa), ulcers, varying degrees of inflammation throughout the colon. |
| CT Scan | Suspected abscess, perforation, or other complications | Abscesses, thickened bowel wall, possible perforation, fluid collection around the affected area | Inflamed bowel wall, possible narrowing of the colon, signs of inflammation in surrounding tissue |
| X-rays | Initial screening for bowel obstruction, detecting significant changes in the digestive tract | Possible signs of bowel obstruction, or gas or fluid accumulation if significant complications exist. | Evidence of inflammation or narrowing of the bowel, possible signs of obstruction. |
Treatment Approaches
Treating diverticulitis and ulcerative colitis involves different strategies tailored to the specific condition and its severity. Understanding these approaches is crucial for effective management and minimizing complications. Successful treatment often hinges on a multi-faceted strategy encompassing medication, dietary changes, and potentially surgical intervention.Diverticulitis and ulcerative colitis, while both affecting the colon, have distinct inflammatory characteristics and responses to treatment.
This section will Artikel the differing treatment approaches for each condition, highlighting the importance of personalized care.
Antibiotic Use in Diverticulitis
Acute diverticulitis episodes frequently require antibiotic treatment to combat bacterial infections. Antibiotics target the bacteria that proliferate in the inflamed diverticula, reducing the infection and promoting healing. Broad-spectrum antibiotics, effective against a wider range of bacteria, are often prescribed. Commonly used antibiotics include metronidazole and ciprofloxacin, though the precise choice may vary depending on individual factors. Prompt antibiotic administration is crucial to minimize the risk of complications such as abscess formation or perforation.
Proper antibiotic selection and duration are important to ensure the effectiveness and safety of treatment.
Anti-inflammatory Medications in Ulcerative Colitis
Ulcerative colitis, characterized by chronic inflammation of the colon, often responds to anti-inflammatory medications. These medications aim to reduce the inflammation, which is central to the disease process. Corticosteroids, such as prednisone, are potent anti-inflammatory drugs that can quickly control symptoms. However, long-term use of corticosteroids can have side effects. Thus, the goal is to gradually taper off the dosage as the inflammation subsides.
Other anti-inflammatory drugs, like aminosalicylates (e.g., mesalamine), are often used in milder cases, offering a less potent but potentially safer approach for long-term management. The specific type and dosage of anti-inflammatory medication are tailored to the individual’s needs and the severity of their condition.
Ever wondered about the differences between diverticulitis and ulcerative colitis? It’s a tricky area, and often, people with IBS find themselves struggling to manage their symptoms. Fortunately, understanding how to lose weight with IBS can be a powerful tool in managing overall digestive health, which can impact both diverticulitis and ulcerative colitis. Learning more about strategies for losing weight with ibs could significantly help in managing these conditions.
Ultimately, a balanced approach is key when dealing with diverticulitis versus ulcerative colitis.
Surgical Interventions
In severe cases of both diverticulitis and ulcerative colitis, surgical intervention might be necessary. In diverticulitis, surgical procedures may address complications such as abscesses, fistulas, or perforations. These procedures may involve draining the abscess, repairing a perforation, or removing affected sections of the colon. In ulcerative colitis, colectomy, the surgical removal of the colon, may be a consideration for severe, unresponsive cases.
The decision for surgical intervention is made on a case-by-case basis, taking into account the patient’s overall health, the severity of the condition, and the presence of complications.
Dietary Modifications and Lifestyle Changes
Dietary modifications and lifestyle adjustments play a vital role in managing both diverticulitis and ulcerative colitis. For diverticulitis, a low-fiber diet during acute episodes can help reduce strain on the colon. Once the inflammation subsides, a gradual increase in fiber is usually recommended. For ulcerative colitis, a balanced diet with adequate nutrition is essential. While certain foods might trigger symptoms, it is crucial to work with a registered dietitian to identify specific dietary triggers and develop a tailored plan.
Lifestyle factors such as stress management and regular exercise can significantly influence the course of both conditions. The dietary and lifestyle modifications are highly individualized, taking into account the specific needs and preferences of each patient.
Comparison of Treatment Options
| Treatment | Diverticulitis | Ulcerative Colitis |
|---|---|---|
| Antibiotics | Often used for acute episodes to combat infection. | Not typically a primary treatment; used in specific situations |
| Anti-inflammatory medications | Not typically used; the focus is on resolving infection. | Used to control inflammation, often in conjunction with other treatments. |
| Surgical Interventions | Potentially required for complications like abscesses or perforations. | Colectomy (removal of the colon) may be necessary in severe, unresponsive cases. |
| Dietary Modifications | Low-fiber diet during acute episodes, gradual increase afterward. | Balanced diet, identification of triggers, and working with a registered dietitian. |
Complications and Prognosis
Understanding the potential complications and long-term prognosis of diverticulitis and ulcerative colitis is crucial for effective management and patient well-being. These conditions, while treatable, can lead to serious consequences if not monitored and managed appropriately. This section delves into the possible complications and the importance of ongoing follow-up care.The course of both diverticulitis and ulcerative colitis varies significantly among individuals.
Factors such as the severity of the initial attack, the presence of underlying health conditions, and adherence to treatment plans all play a role in shaping the long-term outlook. While complete remission is achievable for many, some individuals may experience recurrent episodes or develop more severe complications.
Potential Complications of Diverticulitis
Diverticulitis, characterized by inflammation of the diverticula (small pouches in the colon), can lead to a range of complications. Prompt diagnosis and appropriate treatment are essential to minimize these risks.
- Bowel Obstruction: Diverticulitis can cause inflammation and scarring in the colon, potentially leading to a blockage in the bowel. This obstruction can result in severe pain, nausea, vomiting, and abdominal distension. In severe cases, surgical intervention might be necessary to restore bowel function.
- Abscess Formation: A collection of pus can form around the inflamed diverticula, leading to an abscess. This can cause significant pain and tenderness in the abdomen, and may require drainage procedures.
- Fistula Formation: An abnormal connection between the colon and other organs or structures (e.g., bladder, vagina) can form as a complication of diverticulitis. This fistula can lead to leakage of stool or other bodily fluids, requiring surgical repair or other interventions.
- Perforation: A perforation occurs when the colon wall tears, potentially releasing intestinal contents into the abdominal cavity. This is a serious complication that necessitates emergency surgery to repair the damage and prevent peritonitis (inflammation of the lining of the abdomen).
Potential Complications of Ulcerative Colitis
Ulcerative colitis, an inflammatory condition affecting the colon and rectum, carries its own set of potential complications. Early intervention and close monitoring are crucial for managing these risks effectively.
Figuring out diverticulitis versus ulcerative colitis can be tricky, right? While I’m no doctor, I’ve been researching different health topics lately, and one thing that’s become clear is how important it is to explore all your options. For example, if you’re looking for ways to avoid hormonal birth control, exploring non hormonal birth control options could be a game-changer.
Ultimately, understanding the differences between diverticulitis and ulcerative colitis is crucial for making informed decisions about your health.
- Toxic Megacolon: This severe complication involves the dilation and paralysis of the colon, which can lead to significant abdominal distention, pain, and potentially life-threatening complications. Rapid medical intervention is critical in such cases.
- Hemorrhage: Ulcerative colitis can cause bleeding from the colon, which can range from mild to severe. Persistent bleeding can lead to anemia and other health problems.
- Strictures: Narrowing of the colon due to scarring can develop in some individuals with ulcerative colitis, potentially obstructing bowel function. Surgical intervention may be required to address these strictures.
- Cancer: Individuals with long-standing ulcerative colitis have an increased risk of developing colon cancer. Regular colonoscopies and close monitoring are crucial for early detection and prevention.
Long-Term Prognosis and Management
The long-term prognosis for both diverticulitis and ulcerative colitis varies depending on the individual’s response to treatment, the severity of the condition, and adherence to prescribed management strategies.
- Regular Follow-up Care: Maintaining regular follow-up appointments with a gastroenterologist or other specialists is essential for monitoring disease progression, detecting complications early, and adjusting treatment plans as needed. These appointments are critical for disease surveillance, enabling timely intervention for complications and adjustments to therapy.
- Dietary Modifications: Dietary changes, including avoiding trigger foods or adopting a specific diet, can play a significant role in managing symptoms and preventing flare-ups. These adjustments can lead to better control of the disease and improved quality of life.
- Medication Management: Pharmacological interventions, such as medications to reduce inflammation or suppress the immune system, are crucial for controlling symptoms and preventing complications. Medication management is crucial for achieving and maintaining remission.
Patient Education: Diverticulitis Vs Ulcerative Colitis
Taking control of your diverticulitis or ulcerative colitis journey involves understanding the condition, actively participating in treatment, and making necessary lifestyle changes. Education empowers you to manage symptoms, prevent complications, and live a fulfilling life. This section will focus on key aspects of patient education, including treatment adherence, lifestyle modifications, common questions, and early warning signs of complications.
Understanding Your Treatment Plan, Diverticulitis vs ulcerative colitis
Adherence to your prescribed treatment plan is crucial for managing your condition effectively. This includes taking medications as directed, attending scheduled appointments, and following dietary recommendations. Consistency in these areas is directly linked to symptom control and preventing exacerbations. Regular communication with your healthcare team is vital to address any concerns or adjustments needed. Consistency is key to managing the condition effectively.
Lifestyle Modifications
Lifestyle modifications play a significant role in managing both diverticulitis and ulcerative colitis. Dietary adjustments, stress management techniques, and regular exercise can positively impact symptom severity and overall well-being. These modifications are not just about short-term relief; they’re about building long-term health and improving quality of life. Identifying triggers and making informed choices are crucial for symptom management.
Common Patient Questions
Patients often have concerns about their condition. Here are some frequently asked questions and their answers.
- What foods should I avoid? Dietary restrictions can vary depending on the individual and the severity of the condition. Generally, high-fiber foods may be limited during flare-ups, and certain triggers, such as spicy foods or processed foods, may need to be avoided. Consulting with a registered dietitian can provide personalized dietary recommendations.
- How can I manage stress? Stress can exacerbate symptoms in some individuals. Stress-reducing techniques such as meditation, yoga, or spending time in nature can be beneficial.
- What are the long-term implications of diverticulitis/ulcerative colitis? The long-term outlook for diverticulitis and ulcerative colitis is generally good with appropriate medical management. However, potential complications such as chronic inflammation or colorectal cancer are possibilities. Ongoing monitoring and adherence to treatment plans are important for minimizing these risks.
Identifying Early Warning Signs of Complications
Recognizing early warning signs of complications is crucial for timely intervention. These signs can vary but often include increased pain, fever, changes in bowel habits (frequency or consistency), and unexplained weight loss. Prompt medical attention is essential for preventing potential serious complications.
- Increased abdominal pain: If the pain worsens or becomes significantly more intense than usual, seeking immediate medical attention is essential. This could indicate a developing complication.
- Fever: A fever, especially a high fever, can be a sign of infection or inflammation, requiring prompt medical evaluation.
- Significant changes in bowel habits: Sudden and significant changes in bowel habits, such as increased frequency or significant changes in consistency (e.g., diarrhea or blood in stool), are important indicators to report to your doctor immediately.
- Unexplained weight loss: Unexplained weight loss can be a sign of underlying inflammation or other complications. It’s important to consult your doctor if you experience this.
Conclusive Thoughts
In summary, understanding the distinct characteristics of diverticulitis and ulcerative colitis is paramount for effective diagnosis and treatment. Key distinctions lie in the location of inflammation, typical symptoms, and the treatment strategies employed. While both conditions can cause significant discomfort and require medical attention, grasping these nuances allows for personalized care and management. Remember to always consult with a healthcare professional for accurate diagnoses and tailored treatment plans.




