Direct vs indirect hernia is a crucial distinction in understanding inguinal hernias. These seemingly similar conditions have distinct anatomical pathways, causes, and treatment approaches. This guide delves into the differences between direct and indirect inguinal hernias, exploring their characteristics, diagnostic methods, surgical management, potential complications, and patient education. We’ll cover everything from the underlying anatomy to the recovery process.
Understanding the nuances of each type is vital for accurate diagnosis and effective treatment. This article provides a clear and concise overview, comparing and contrasting the two types of hernias, ensuring that you have a solid grasp of this complex medical topic.
Introduction to Hernias
A hernia occurs when an organ or tissue protrudes through a weakened or damaged area of the surrounding muscle or connective tissue. This protrusion creates a bulge that can be noticeable or, in some cases, only palpable. The condition can range from mild discomfort to severe pain and complications, depending on the type and location of the hernia.
Understanding the different types, causes, and potential complications is crucial for effective diagnosis and treatment.The anatomical location of a hernia is typically where the weakened area allows the protrusion. This often involves areas where the abdominal wall muscles are naturally thinner, such as the inguinal canal (the passageway for the spermatic cord in males and the round ligament in females) or the femoral canal, and the abdominal wall.
The structure of a hernia involves the organ or tissue, the weakened area, and the surrounding tissue that contains the bulge. Understanding these structural components aids in identifying the location and extent of the issue.
Common Causes of Hernias
Several factors contribute to the development of hernias. Weakened abdominal muscles, often resulting from chronic strain or trauma, are a primary cause. Conditions like chronic coughing or lifting heavy objects can put significant stress on the abdominal muscles, increasing the risk of a hernia. Additionally, genetics play a role in predisposing some individuals to hernias. A family history of hernias can increase an individual’s susceptibility to developing one.
Pregnancy, due to the strain on the abdominal muscles, can also increase the risk of hernias. Obesity is also a contributing factor due to the added weight and stress on the abdominal wall.
Types of Hernias (General Overview)
Hernias are broadly categorized based on their location and the type of tissue that protrudes. A general overview of these types includes:
- Inguinal hernias: These are the most common type, occurring in the inguinal canal. They are more frequent in men than women. The protruding tissue, often part of the intestines, bulges through the weakened area of the inguinal canal.
- Femoral hernias: These hernias are located in the femoral canal, which is located lower than the inguinal canal. They are less common than inguinal hernias and occur more often in women.
- Hiatal hernias: These hernias involve the protrusion of a portion of the stomach through the diaphragm, the muscular wall separating the chest and abdomen. This can lead to symptoms like heartburn or acid reflux.
- Umbilical hernias: These hernias occur at the belly button (umbilicus). They are common in infants and often resolve on their own. However, they can persist into adulthood.
- Incisional hernias: These hernias develop at the site of a previous surgical incision. This can happen if the surgical repair did not adequately address the weakened area or if the incision site was not properly healed.
Direct vs. Indirect Inguinal Hernias
Understanding the differences between direct and indirect inguinal hernias is crucial for accurate diagnosis and treatment. These two types, while both involving a protrusion of abdominal contents through a weakness in the abdominal wall, differ significantly in their anatomical pathways, risk factors, and typical presentation. This detailed comparison will help illuminate the unique characteristics of each.Inguinal hernias are a common condition, often requiring surgical intervention.
Distinguishing between direct and indirect hernias is essential for surgeons to plan the most appropriate repair. Precise diagnosis is crucial for patient care, and knowing the anatomical differences is fundamental to the process.
Anatomical Pathways
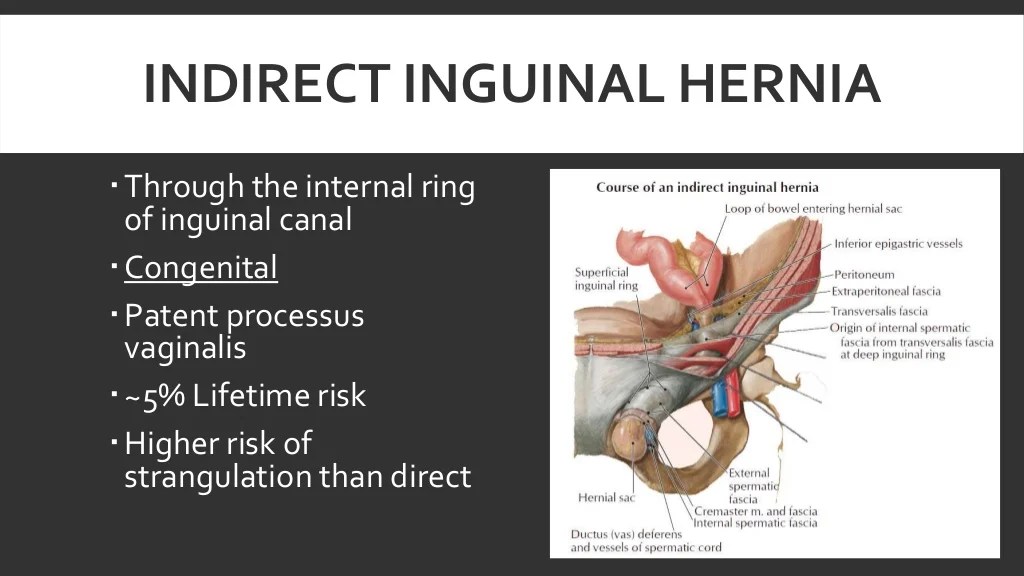
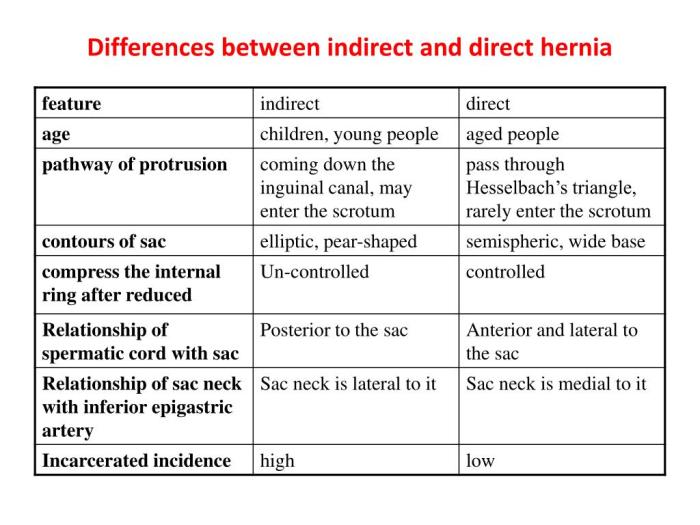
Direct hernias arise from a weakness in the transversalis fascia, a layer of connective tissue in the abdominal wall. This weakness allows a direct passage for abdominal contents to push through the abdominal wall. In contrast, indirect hernias follow a pre-existing pathway, the processus vaginalis, a remnant of the fetal structure. This passage allows abdominal contents to travel laterally through the inguinal canal.
Understanding the difference between direct and indirect hernias is key to proper diagnosis. Direct hernias bulge through weakened abdominal wall areas, while indirect hernias, often more complex, travel through natural pathways. Learning about surgical mesh options like Vectra DA, which is used in hernia repair, can provide additional insight into modern treatment methods. What is vectra da is a critical piece of the puzzle when considering the various types of hernias and the best approaches for repair.
Ultimately, understanding the distinctions between direct and indirect hernias remains essential for informed decision-making in healthcare.
Locations of Direct and Indirect Hernias, Direct vs indirect hernia
Direct hernias are typically located medial to the inferior epigastric vessels, the blood vessels supplying the lower abdomen. Indirect hernias, on the other hand, are typically found lateral to the inferior epigastric vessels, closer to the inguinal ligament.
Risk Factors Associated with Each Type
Several factors increase the risk of developing either type of hernia. Age, chronic coughing, and heavy lifting are common risk factors for both. However, some risk factors are more closely associated with one type than the other.
Risk Factors for Direct Hernias
Increased intra-abdominal pressure, obesity, and chronic conditions that lead to persistent coughing are common risk factors for direct inguinal hernias. For instance, individuals with chronic obstructive pulmonary disease (COPD) or those who frequently lift heavy objects are at a higher risk.
Risk Factors for Indirect Hernias
Indirect hernias are often associated with a history of a particular type of abdominal surgery, or they may be present at birth. Weakened connective tissue, or a history of previous hernias can also increase risk.
Key Characteristics of Direct and Indirect Inguinal Hernias
| Characteristic | Direct Hernia | Indirect Hernia |
|---|---|---|
| Location | Medial to the inferior epigastric vessels | Lateral to the inferior epigastric vessels |
| Cause | Weakness in the transversalis fascia, often associated with increased intra-abdominal pressure. | Defect in the processus vaginalis, a remnant of the fetal structure. |
| Risk Factors | Increased intra-abdominal pressure, obesity, chronic cough, and heavy lifting. | Family history of hernias, previous abdominal surgery, or congenital weakness of the abdominal wall. |
| Presentation | A bulge may be palpable, especially during straining or coughing. Pain may be mild or absent. | A bulge may be palpable, often noticeable when the patient stands or strains. Pain may be mild or moderate. |
Diagnostic Methods
Differentiating between direct and indirect inguinal hernias is crucial for effective treatment planning. Accurate diagnosis relies on a combination of clinical assessment and imaging techniques. A thorough understanding of the diagnostic methods allows healthcare professionals to determine the appropriate surgical approach and minimize potential complications.
Physical Examination
Physical examination plays a pivotal role in the initial evaluation of suspected inguinal hernias. It’s a non-invasive method that provides valuable information about the location, size, and characteristics of the hernia. The examiner typically examines the inguinal region, palpating for a bulge or mass, especially during maneuvers that increase intra-abdominal pressure (like coughing or straining). The consistency and reducibility of the hernia are assessed to determine if the protrusion can be manually pushed back into the abdominal cavity.
Imaging Techniques
Imaging techniques, like ultrasound and CT scans, provide more detailed information about the hernia, including its size, location, and relationship to surrounding structures. These methods are particularly helpful in complex cases or when the clinical picture is unclear.
Ever wondered about the difference between direct and indirect hernias? It’s a fascinating topic in medical understanding. While discussing these types of hernias, it’s important to remember that sometimes, other health issues like arthritis on one side of the body arthritis on one side of the body can be completely unrelated, but it’s crucial to remember that pain on one side of the body can have various causes.
Ultimately, understanding the nuances of direct versus indirect hernias is key to proper diagnosis and treatment.
Diagnostic Tools and Their Applications
| Diagnostic Tool | Procedure | Indications | Limitations |
|---|---|---|---|
| Physical Examination | The examiner palpates the inguinal region, paying attention to the presence of a bulge or mass, particularly during maneuvers like coughing or straining. The consistency and reducibility of the hernia are assessed. | Initial evaluation of suspected inguinal hernias, identifying the location, size, and general characteristics. Useful for differentiating between direct and indirect hernias in uncomplicated cases. | Inability to visualize the deeper structures, difficulty in evaluating the extent of the hernia in obese individuals, or when the hernia is small or difficult to palpate. The reliability of the examination depends on the examiner’s experience and skill. |
| Ultrasound | High-frequency sound waves are used to create images of the inguinal region. The technique allows for visualization of the hernia sac, its contents, and its relationship to surrounding structures. | Evaluating the hernia’s size, shape, and content; differentiating between direct and indirect hernias, and assessing the presence of complications like incarceration or strangulation, especially when physical examination findings are inconclusive. It is also helpful in patients with a high BMI where palpation may be less effective. | Limited ability to visualize deep structures, and the image quality can be affected by patient positioning and the presence of bowel gas. It might not be as definitive as a CT scan in assessing the extent of the hernia or identifying specific anatomical details. |
| CT Scan | A CT scan uses X-rays to generate detailed cross-sectional images of the inguinal region. This technique provides detailed anatomical information about the hernia and surrounding structures, including the inguinal canal and the spermatic cord. | Assessing the extent of the hernia, identifying the presence of complications like incarceration or strangulation, evaluating the presence of associated abnormalities, or when more detailed anatomical information is required, particularly in complex cases. A CT scan may be preferred over ultrasound when there’s a suspicion of a possible underlying pathology. | Exposure to ionizing radiation, potential for contrast agent allergy, and the higher cost compared to ultrasound. The presence of bowel gas can sometimes obscure visualization of the hernia sac. |
Surgical Management
Surgical repair is the definitive treatment for hernias, aiming to restore the weakened abdominal wall and prevent recurrence. Different surgical techniques are employed, depending on the type of hernia and the patient’s specific needs. The choice of approach considers factors like the hernia’s size, location, and the surgeon’s expertise. Post-operative recovery is crucial, and patient compliance with rehabilitation exercises is vital for successful outcomes.
Common Surgical Approaches for Hernia Repair
Various surgical approaches are available, each with its own advantages and disadvantages. These methods vary in their invasiveness, recovery time, and potential for complications. Minimally invasive techniques are increasingly popular due to their reduced pain and scarring.
Techniques for Direct Hernia Repair
Direct hernias often involve a technique known as the “Bassini repair.” This approach involves strengthening the weakened transversalis fascia and the posterior wall of the inguinal canal. In this technique, the surgeon creates a new support structure to prevent future herniation. A synthetic mesh, sometimes, is used to reinforce the repair site and increase the structural integrity of the abdominal wall.
- The surgeon identifies the defect in the transversalis fascia.
- The defect is closed using sutures or a mesh.
- The spermatic cord (in males) is carefully identified and protected during the procedure.
- The incision is closed with sutures.
Techniques for Indirect Hernia Repair
Indirect hernias often necessitate a more extensive repair, potentially including the use of mesh. The “Lichtenstein repair” is a common technique for this type of hernia. This procedure aims to reinforce the weakened inguinal floor.
Ever wondered about the difference between direct and indirect hernias? It’s a fascinating medical topic, but honestly, my mind often wanders. Finding natural ways to manage focus and concentration is key, and exploring options like natural remedies for adhd could be beneficial for someone dealing with similar issues. Regardless of the cause, understanding the distinct anatomical paths of direct versus indirect hernias is crucial for proper diagnosis and treatment.
- The surgeon locates the hernia sac and gently reduces the contents of the hernia.
- The hernia sac is ligated and excised.
- A mesh is positioned over the inguinal floor to provide additional support.
- The incision is closed with sutures.
Comparison of Surgical Approaches
| Surgical Approach | Direct Hernia Repair | Indirect Hernia Repair |
|---|---|---|
| Technique | Bassini repair, often involving reinforcement of the transversalis fascia. Potential use of synthetic mesh. | Lichtenstein repair, typically including the use of a mesh to reinforce the inguinal floor. The hernia sac is identified and addressed. |
| Advantages | Relatively simpler procedure, potentially shorter recovery time, and lower risk of complications in some cases. | Stronger support provided by the mesh, reduced risk of recurrence compared to some other techniques, and effective in addressing larger or more complex hernias. |
| Disadvantages | May not be suitable for all cases, especially those with significant tissue weakness or complex hernias. Potentially higher risk of recurrence in some cases compared to indirect hernia repairs with mesh. | Potential for mesh-related complications, such as infection or chronic pain, slightly longer recovery time, and slightly higher risk of complications related to the mesh. |
Complications and Post-operative Care: Direct Vs Indirect Hernia
Post-operative care for hernia repairs is crucial for a smooth recovery and to minimize the risk of complications. Understanding potential issues and the importance of diligent follow-up can significantly impact patient outcomes. This section delves into the common complications associated with hernia repairs and emphasizes the necessary post-operative care strategies.The successful outcome of hernia surgery depends not only on the surgeon’s expertise but also on the patient’s proactive participation in post-operative care.
Adherence to instructions, regular check-ups, and prompt reporting of any unusual symptoms are vital for preventing complications and ensuring a complete recovery.
Potential Complications
A variety of complications can arise following hernia repair. These range from relatively minor issues to more serious conditions that may necessitate further interventions. Awareness of these potential problems is essential for both patients and healthcare providers to ensure swift and effective management.
- Hematoma: A hematoma is a collection of blood outside blood vessels. It can occur due to bleeding from the surgical site. While often self-limiting, a significant hematoma may require aspiration or additional surgical intervention to prevent complications like infection or nerve compression. Examples include post-operative swelling and pain that do not subside within a few days.
- Infection: Infection at the surgical site is a serious concern. Symptoms such as increased pain, redness, swelling, warmth, or pus discharge around the incision require immediate medical attention. Proper wound care and antibiotic therapy are crucial for controlling the infection and preventing its spread.
- Seromas: Seromas are fluid collections at the surgical site. They often form as a result of the body’s response to the surgical trauma. While usually not serious, they may require drainage if they become large or cause discomfort. Symptoms include persistent swelling and tenderness at the surgical site.
- Recurrence: Recurrence, the reappearance of the hernia, is a possibility after surgery. Factors like inadequate repair technique, insufficient tissue support, or patient factors like persistent coughing or straining can contribute to recurrence. Proper patient education about avoiding these factors is crucial in preventing recurrence.
- Nerve Injury: Nerve injury, although less frequent, can occur during the surgical procedure. This can manifest as persistent numbness, tingling, or pain in the area surrounding the repair. Prompt diagnosis and appropriate management, potentially including physical therapy, are necessary for nerve recovery.
Importance of Post-operative Care and Follow-up
Diligent post-operative care and regular follow-up visits are paramount for successful recovery and to minimize the risk of complications. Patients should meticulously follow their surgeon’s instructions, which may include pain management, wound care, activity restrictions, and dietary recommendations. Prompt reporting of any concerning symptoms is essential for early intervention and effective management.This proactive approach empowers patients to take an active role in their recovery, improving the chances of a complete and uncomplicated healing process.
Regular follow-up appointments allow for monitoring of the surgical site, detection of potential complications, and adjustments to the post-operative care plan as needed.
Patient Education
Understanding and managing a hernia involves more than just surgery. A crucial component of successful treatment is comprehensive patient education. This empowers individuals to actively participate in their recovery, making informed decisions and minimizing potential complications. This section details the essential aspects of patient education, focusing on hernia types, risks, and the recovery process.
Hernia Types and Risks
Patient education should clearly explain the different types of hernias, emphasizing the distinction between direct and indirect inguinal hernias. Understanding the anatomical differences is key to comprehending the risks and appropriate treatment strategies. Direct hernias typically occur through a weakness in the abdominal wall, while indirect hernias involve a protrusion through a weakness in the inguinal canal. These differences influence the surgical approach and potential complications.
- Direct Inguinal Hernia: These hernias are characterized by a protrusion through a weakness in the transversalis fascia. They typically occur in older individuals and are often associated with increased intra-abdominal pressure.
- Indirect Inguinal Hernia: These hernias occur when the processus vaginalis, a structure present during fetal development, fails to close completely. This allows a portion of the intestine to protrude into the inguinal canal. Indirect hernias are more common in younger individuals and can sometimes be present from birth.
Educating patients about the potential complications of hernias is equally important. These can include strangulation, where the protruding tissue becomes trapped and cut off from blood supply, and obstruction, where the intestine becomes compressed, potentially leading to severe pain and even life-threatening conditions. Early detection and prompt surgical intervention are critical in these cases. Risk factors, such as chronic cough, heavy lifting, and obesity, should be discussed, emphasizing the importance of preventative measures.
Recovery Process
Post-operative recovery is a critical phase of hernia treatment. Clear instructions and realistic expectations are essential to ensure a smooth and successful recovery. The education should cover pain management strategies, activity restrictions, and when to seek medical attention.
- Pain Management: Post-operative pain is common, and patients should be provided with clear instructions on pain medication use, including dosages and potential side effects. Non-pharmacological methods, such as ice packs and gentle movement, should also be discussed.
- Activity Restrictions: Post-operative activity restrictions are vital to prevent strain on the surgical site and promote healing. Patients should be advised on the types of activities they can and cannot perform during the initial recovery period. Examples of activities to avoid include heavy lifting, strenuous exercise, and excessive straining. Gradual return to normal activities is key, following the surgeon’s recommendations.
- Follow-up Appointments: Regular follow-up appointments with the surgeon are crucial for monitoring healing, addressing any concerns, and ensuring the hernia does not recur. The importance of these appointments should be stressed, along with the schedule for follow-up visits.
Pre-Operative Patient Education
Pre-operative education is vital to prepare patients for the upcoming surgery and to reduce anxiety. This involves providing information about the procedure, potential risks, and post-operative care. It’s also a time to address any concerns or questions patients may have.
- Understanding the Procedure: A detailed explanation of the surgical procedure, including the specific technique to be used, helps patients feel more informed and comfortable. Illustrative materials, such as diagrams, can further enhance understanding.
- Potential Risks and Complications: Patients should be informed about potential risks and complications associated with the surgery. Addressing these concerns proactively can help manage anxiety and set realistic expectations.
- Pre-operative Instructions: Clear pre-operative instructions, such as dietary restrictions, medication adjustments, and fasting guidelines, are essential for ensuring a smooth surgical process. These instructions should be provided in writing and discussed in detail with the patient.
Patient Questions
Patients often have numerous questions regarding direct and indirect hernias. These questions should be addressed proactively to alleviate concerns and ensure a positive patient experience. This comprehensive approach empowers patients to make informed decisions and actively participate in their recovery.
- What are the long-term effects of a hernia? Long-term effects are usually minimal with successful surgical repair, but patients should be aware that complications such as recurrence may occur. Regular follow-up appointments are essential for ongoing management.
- What are the different types of surgical approaches? The surgical approach depends on the hernia type and individual patient factors. Open or laparoscopic approaches are common, and patients should be informed about the advantages and disadvantages of each.
- How long will the recovery take? Recovery time varies based on individual factors, including the complexity of the procedure, the patient’s overall health, and adherence to post-operative instructions. A personalized recovery plan is crucial for optimal outcomes.
Conclusion
In conclusion, differentiating between direct and indirect inguinal hernias is critical for proper diagnosis and treatment. The key distinctions in their anatomical pathways, risk factors, and clinical presentations have been highlighted. This information empowers patients and healthcare professionals to navigate this important medical condition effectively. Remember, seeking medical advice from a qualified healthcare provider is essential for accurate diagnosis and personalized care.




