Difference between alzheimers and lewy body dementia – Understanding the difference between Alzheimer’s and Lewy body dementia is crucial for early diagnosis and effective care. These conditions, while both debilitating, present unique challenges in terms of symptoms, progression, and ultimately, how they impact daily life. This exploration delves into the nuanced distinctions between these two forms of dementia, highlighting the key characteristics that help clinicians and families navigate this complex landscape.
This comprehensive guide will walk you through the core differences in the neuropathology of each disease, including the presence of amyloid plaques and neurofibrillary tangles in Alzheimer’s, and the presence of Lewy bodies in Lewy Body Dementia. We’ll discuss the typical cognitive and motor symptoms, the progression timeline, and the diagnostic criteria. Tables will visually compare and contrast the symptoms and diagnostic challenges.
We’ll also touch on the impact these dementias have on daily life and offer insights into management strategies and caregiver support.
Introduction to Dementias
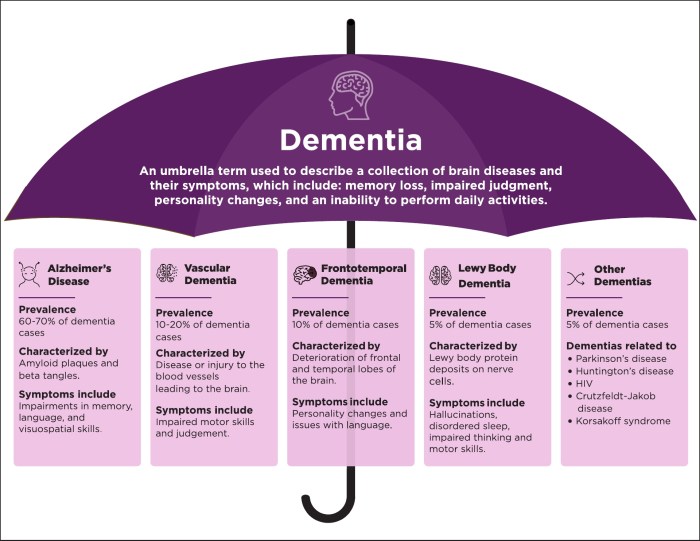
Dementia is not a single disease, but rather a broad term encompassing a range of progressive conditions that gradually impair cognitive functions. These conditions affect memory, thinking, problem-solving, and behavior, significantly impacting the daily lives of those affected and their families. The hallmark of dementia is a decline in cognitive abilities beyond what is considered normal age-related changes.
This decline is progressive and irreversible, leading to increasing dependence on others for care.The common symptoms of various dementias often overlap, making diagnosis challenging. While memory loss is a frequent early symptom, other problems like difficulty with language, visual-spatial processing, and changes in personality and behavior are also commonly observed. Understanding the specific pattern of cognitive decline, the speed of progression, and the accompanying non-cognitive symptoms is crucial for accurate diagnosis and appropriate management.
Early detection and intervention are essential to maximize quality of life and support for individuals and families.
General Characteristics of Dementia
Dementia is characterized by a decline in cognitive functions, impacting daily life. This decline is not a typical part of aging. Common symptoms include memory loss, difficulty with language, impaired judgment, and changes in personality. These symptoms vary depending on the specific type of dementia. The severity of these symptoms progressively worsens over time.
Common Symptoms Across Dementia Types
A variety of symptoms can manifest across different types of dementia, sometimes making differentiation difficult. These symptoms often include memory problems, difficulties with communication, changes in personality and behavior, and impaired judgment. Specific symptoms, like visual-spatial issues or motor problems, might be more prominent in certain types.
Importance of Early Diagnosis and Intervention
Early diagnosis of dementia is crucial for several reasons. It allows for timely intervention, which can slow the progression of symptoms and improve quality of life. Early diagnosis also allows individuals and families to plan for the future, including adjusting daily routines, seeking appropriate support services, and making decisions about future care. This proactive approach empowers individuals and families to navigate the challenges of dementia effectively.
Comparison of Dementia Types
| Dementia Type | Symptoms | Progression Rate | Typical Age of Onset |
|---|---|---|---|
| Alzheimer’s Disease | Progressive memory loss, confusion, difficulty with language, personality changes. | Moderate to slow, often over several years. | Typically 60-80, but can occur earlier. |
| Vascular Dementia | Step-wise decline in cognitive function, often linked to stroke events, problems with attention and concentration. | Variable, potentially faster depending on stroke frequency and severity. | Typically 65 and older, but can occur earlier. |
| Lewy Body Dementia | Fluctuating cognitive abilities, visual hallucinations, Parkinsonian motor symptoms (e.g., rigidity, tremors). | Moderate to fast, often over 5-10 years. | Typically 60-80, but can occur earlier. |
| Frontotemporal Dementia | Changes in personality, behavior, and language, often impacting social skills and judgment, early onset of inappropriate social behavior. | Variable, can progress quickly or slowly. | Typically between 40-65, sometimes earlier. |
Defining Alzheimer’s Disease
Alzheimer’s disease, a progressive neurodegenerative disorder, is a devastating affliction impacting millions worldwide. It gradually erodes cognitive abilities and disrupts daily life, impacting not only the individual but also their families and caregivers. Understanding the underlying mechanisms, symptoms, and progression of Alzheimer’s is crucial for effective diagnosis, treatment, and support.Alzheimer’s is characterized by the accumulation of abnormal protein deposits in the brain.
These deposits, along with the loss of connections between nerve cells, lead to the progressive decline in cognitive functions.
Neuropathological Hallmarks
The defining pathological features of Alzheimer’s disease are the presence of amyloid plaques and neurofibrillary tangles. Amyloid plaques are abnormal clumps of protein fragments, primarily beta-amyloid, that accumulate between nerve cells. Neurofibrillary tangles are twisted fibers of another protein, tau, that form inside nerve cells. These abnormal protein aggregates disrupt communication between neurons, leading to neuronal dysfunction and eventual cell death.
Cognitive Symptoms
Individuals with Alzheimer’s disease experience a range of cognitive symptoms that vary in severity and progression. Early symptoms often include subtle memory problems, difficulty with language, and impaired judgment. As the disease progresses, these symptoms become more pronounced, affecting daily functioning, and leading to significant challenges in communication, decision-making, and performing everyday tasks.
Progression Timeline
Alzheimer’s disease typically progresses through several stages, characterized by a gradual worsening of symptoms. Early-stage Alzheimer’s is often characterized by mild memory problems and subtle changes in behavior. Middle-stage Alzheimer’s involves more pronounced cognitive decline, including difficulties with language, spatial orientation, and problem-solving. Late-stage Alzheimer’s is marked by severe cognitive impairment, significant functional limitations, and the need for extensive care.
It’s important to note that the progression timeline can vary greatly between individuals.
Cognitive Domains Affected
The cognitive domains affected in Alzheimer’s disease are diverse and interconnected. The following table Artikels some of the key cognitive domains, along with examples of specific symptoms observed in each:
| Cognitive Domain | Specific Symptoms |
|---|---|
| Memory | Difficulty remembering recent events, misplacing belongings, repeating questions, forgetting appointments. |
| Language | Problems with finding the right words, difficulty understanding spoken or written language, decreased vocabulary, reduced ability to express thoughts. |
| Executive Function | Difficulty with planning, organizing, initiating tasks, multitasking, judgment, problem-solving, abstract thinking. |
| Visuospatial Skills | Problems with recognizing faces, reading maps, navigating familiar surroundings, difficulty judging distances, misplacing objects. |
| Behavioral and Psychological Symptoms | Agitation, anxiety, depression, aggression, wandering, sleep disturbances, delusions, hallucinations. |
Defining Lewy Body Dementia
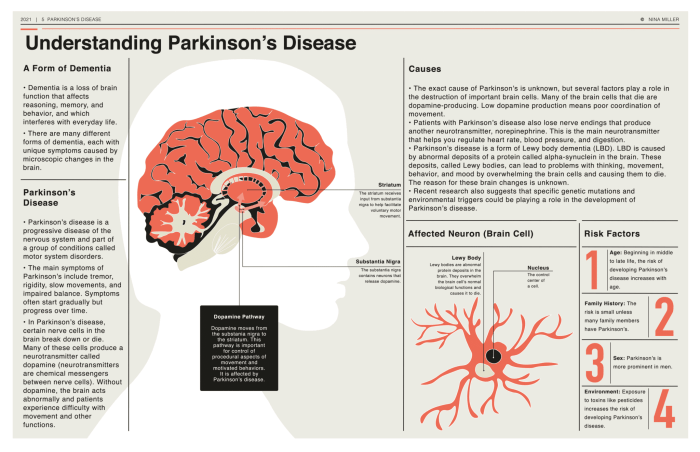
Lewy body dementia (LBD) is a progressive neurodegenerative disorder that affects cognitive function, movement, and behavior. It’s a challenging diagnosis, often misdiagnosed as Alzheimer’s disease or other dementias, due to the overlapping symptoms. Understanding the specific pathological characteristics, cognitive symptoms, and motor features of LBD is crucial for accurate diagnosis and appropriate management.Lewy body dementia is characterized by the abnormal accumulation of protein deposits, called Lewy bodies, within the brain’s nerve cells.
These protein clumps interfere with the normal functioning of these cells, leading to a decline in various brain functions. The presence of Lewy bodies is a defining feature, but it’s important to note that other conditions can also exhibit similar pathology. This makes diagnosis reliant on a thorough evaluation of a patient’s clinical presentation and, often, the results of specialized testing.
Pathological Characteristics
Lewy bodies are abnormal aggregates of a protein called alpha-synuclein. These aggregates accumulate within the brain’s neurons, disrupting their normal function and ultimately leading to cell death. This accumulation is particularly prevalent in areas of the brain associated with movement, memory, and alertness. The exact mechanism by which Lewy bodies cause neuronal dysfunction is still under investigation, but it’s believed to involve disruptions in protein transport, cellular communication, and ultimately, cell death.
The presence of Lewy bodies is a key hallmark of LBD.
Cognitive Symptoms
Cognitive impairment in LBD is often characterized by fluctuating levels of awareness and attention. Patients may experience periods of confusion, drowsiness, or even hallucinations. Difficulties with memory, judgment, and problem-solving are also common. The fluctuating nature of cognitive impairment is a distinguishing feature from other dementias, where symptoms tend to be more consistent. Patients may experience periods of clarity and sharp cognitive function interspersed with periods of significant impairment.
Motor Symptoms
Motor symptoms in LBD often manifest early in the disease progression. Parkinsonism, a group of symptoms that mimic Parkinson’s disease, is a common feature, including rigidity, slowness of movement (bradykinesia), and tremors. These motor symptoms can fluctuate just as cognitive function does. Postural instability, characterized by difficulty maintaining balance and frequent falls, is another frequently observed motor symptom.
The presence of these motor features, particularly in conjunction with cognitive fluctuations, is a significant indicator for LBD.
Fluctuations in Cognitive Function
Fluctuations in cognitive function are a core feature of LBD. This means that a patient’s mental abilities can vary significantly throughout the day or even within a single day. One moment they might be alert and engaged, and the next they might be confused or disoriented. These fluctuations are a key differentiator from other dementias, where cognitive decline tends to be more consistent.
The variability in mental acuity makes daily activities challenging and often requires support from caregivers.
Characteristic Motor Symptoms, Difference between alzheimers and lewy body dementia
The motor symptoms in LBD often mirror those of Parkinson’s disease, including tremors, rigidity, and slowness of movement. These symptoms can be prominent and may even precede the cognitive decline. The fluctuations in motor symptoms, like the cognitive ones, are also characteristic of LBD. Falls are also common due to postural instability. The presence of both cognitive and motor fluctuations is a key feature in differentiating LBD from other dementias.
Diagnostic Criteria
| Symptoms | Diagnostic Tests | Differentiating Factors from Other Dementias |
|---|---|---|
| Fluctuating cognition, visual hallucinations, parkinsonian features | Neuropsychological testing, neuroimaging (e.g., CT, MRI), detailed medical history, sleep studies | Fluctuations are a key differentiator from other dementias; visual hallucinations are less common in Alzheimer’s disease; parkinsonian features distinguish it from frontotemporal dementia |
| Presence of Lewy bodies | Brain biopsy (rare), but sometimes helpful | Lewy bodies are the defining pathological feature |
| Sensitivity to antipsychotic medications | Careful monitoring of response to antipsychotics | Antipsychotics can cause severe reactions in patients with LBD |
Distinguishing Features
Navigating the complexities of dementia diagnoses often hinges on subtle distinctions between similar conditions. Alzheimer’s disease and Lewy body dementia, while both progressive brain disorders leading to cognitive decline, manifest with unique symptom profiles. Understanding these differences is crucial for accurate diagnosis and tailored care.While both conditions share some overlapping symptoms, key distinctions lie in the timing and prominence of various cognitive, motor, and behavioral manifestations.
Understanding the subtle differences between Alzheimer’s and Lewy body dementia can be tricky. While both affect cognitive function, Lewy body dementia often presents with more pronounced visual hallucinations and movement issues. Learning about the various treatments for these conditions is crucial, and for skincare concerns, exploring treatments like benzoyl peroxide can be beneficial. all about benzoyl peroxide is a great resource for those looking for more information.
Ultimately, a thorough diagnosis by a medical professional is essential for proper management of either condition.
Pinpointing these distinctions can significantly impact the course of treatment and support provided to individuals and their families.
Cognitive Symptoms
Alzheimer’s disease typically begins with gradual declines in memory, particularly short-term memory. Language difficulties, problems with spatial reasoning, and executive functions (planning, organizing) also emerge over time. The progression of these cognitive impairments is usually relatively steady. In contrast, Lewy body dementia often presents with more fluctuating cognitive abilities. Individuals may experience periods of significant cognitive impairment followed by relative clarity, a pattern not always seen in Alzheimer’s.
Visual hallucinations and disturbances in alertness are more common early on in Lewy body dementia than in Alzheimer’s.
While both Alzheimer’s and Lewy body dementia can cause cognitive decline, understanding their subtle differences is crucial. For example, the fluctuating nature of symptoms, like alertness, can sometimes be mistaken for delirium. If you’re concerned about these symptoms, it’s important to learn more about delirium; delirium what you should know can provide valuable insight.
Ultimately, accurate diagnosis relies on careful evaluation by a medical professional to differentiate between these conditions.
Motor Symptoms
Lewy body dementia is characterized by a distinctive set of motor symptoms. Parkinsonian symptoms, such as rigidity, slowness of movement (bradykinesia), and tremors, often appear early in the disease and can be prominent. These motor features are less common or less pronounced in Alzheimer’s disease. The gait abnormalities often seen in Lewy body dementia, such as shuffling steps and instability, further differentiate it from Alzheimer’s, where gait issues tend to develop later and are less pronounced.
Behavioral and Psychological Symptoms
Behavioral and psychological symptoms of dementia (BPSD) can occur in both Alzheimer’s and Lewy body dementia, although they differ in their expression. Depression, anxiety, and apathy are common in both conditions, but Lewy body dementia is often associated with more pronounced fluctuations in mood and greater instances of delusions and hallucinations. For example, a person with Lewy body dementia might experience vivid visual hallucinations, while a person with Alzheimer’s might exhibit more subtle behavioral changes like social withdrawal.
A comprehensive assessment of the specific patterns of these symptoms is critical in distinguishing between the two conditions.
Diagnostic Challenges
The overlap in symptoms between Alzheimer’s and Lewy body dementia creates significant diagnostic challenges. A precise diagnosis often requires a comprehensive assessment that considers the patient’s medical history, cognitive performance, motor skills, and behavioral patterns. The evaluation should include detailed interviews with the patient and caregivers, neuropsychological testing, and potentially brain imaging techniques. The complexity of these conditions necessitates a multidisciplinary approach.
| Feature | Alzheimer’s Disease | Lewy Body Dementia |
|---|---|---|
| Cognitive Decline | Gradual, steady decline in memory, language, and executive functions. | Fluctuating cognitive abilities, with periods of clarity interspersed with impairment. |
| Motor Symptoms | Less common or less pronounced Parkinsonian symptoms; gait issues typically develop later and are less severe. | Prominent Parkinsonian symptoms (rigidity, slowness, tremors) often appear early in the disease. |
| Behavioral Symptoms | Depression, anxiety, apathy, and more subtle behavioral changes. | Fluctuations in mood, more pronounced delusions and hallucinations (especially visual). |
| Hallucinations | Less frequent and often less vivid. | More frequent and often vivid, particularly visual hallucinations. |
| Diagnosis | Based on cognitive and memory testing, and medical history. | More complex, requiring a comprehensive assessment including motor function, behavioral observations, and possibly brain imaging. |
Diagnosis and Management: Difference Between Alzheimers And Lewy Body Dementia
Navigating the complexities of dementia diagnoses, particularly distinguishing between Alzheimer’s and Lewy body dementia, requires a multifaceted approach. Accurate diagnosis is crucial for tailoring appropriate management strategies and ensuring the best possible quality of life for individuals and their families. The journey often involves a combination of medical assessments, cognitive evaluations, and careful observation of symptom progression.Effective management of these conditions involves a holistic strategy that encompasses both pharmacological and non-pharmacological interventions.
Understanding the nuances of each approach is vital for maximizing benefits and minimizing potential side effects. Furthermore, fostering a supportive environment for both the patient and their caregivers is essential for navigating the challenges of long-term care.
Diagnostic Process
The diagnostic process for both Alzheimer’s and Lewy body dementia relies heavily on a thorough medical history, neurological examinations, and cognitive testing. Medical professionals gather information about the patient’s past medical conditions, family history of dementia, and the progression of cognitive decline. Neurological examinations assess reflexes, muscle tone, balance, and coordination, providing insights into potential neurological abnormalities. Cognitive testing evaluates memory, language skills, problem-solving abilities, and other cognitive functions.
These assessments help distinguish between different types of dementia and identify any underlying medical conditions that might be contributing to the symptoms.
Non-Pharmacological Management
Non-pharmacological approaches play a critical role in managing the symptoms of both Alzheimer’s and Lewy body dementia. Lifestyle modifications, such as maintaining a healthy diet, regular exercise, and cognitive stimulation activities, can significantly improve overall well-being and slow the progression of cognitive decline. Supportive therapies, including occupational therapy, physical therapy, and speech therapy, can help individuals maintain their independence and functional abilities.
Understanding the subtle differences between Alzheimer’s and Lewy body dementia can be tricky. While both affect cognitive function, Lewy body dementia often presents with visual hallucinations and movement problems, unlike Alzheimer’s. Protecting yourself and your loved ones from harmful radiation during dental X-rays is crucial, and using lead aprons dental x ray is a key preventative measure.
Ultimately, recognizing these distinctions helps doctors make the right diagnosis and tailor treatment plans.
These therapies address specific needs and challenges faced by patients with these conditions, allowing them to adapt and thrive in their daily lives. For example, occupational therapy can help individuals with daily tasks such as dressing and eating, while physical therapy can improve mobility and balance.
Pharmacological Management
Several medications are commonly used to manage symptoms in both Alzheimer’s and Lewy body dementia. While not a cure, these medications can help improve cognitive function, manage behavioral symptoms, and alleviate non-cognitive symptoms.
| Drug Name | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Donepezil (Aricept) | Inhibits the breakdown of acetylcholine, a neurotransmitter crucial for memory and cognitive function. | Nausea, vomiting, diarrhea, insomnia, headache. |
| Rivastigmine (Exelon) | Similar to Donepezil, inhibiting the breakdown of acetylcholine. | Nausea, vomiting, diarrhea, weight loss, insomnia. |
| Memantine (Namenda) | Regulates glutamate activity, a neurotransmitter involved in learning and memory. | Headache, dizziness, constipation, confusion. |
| Quetiapine (Seroquel) | Antipsychotic medication used to manage behavioral and psychiatric symptoms. | Sedation, weight gain, orthostatic hypotension, dizziness. |
Caregiver Support and Education
Caring for individuals with dementia requires significant emotional and practical support. Caregivers often face immense stress and challenges. Caregiver support groups, educational programs, and respite care services can provide essential resources and guidance. Education about the specific needs of individuals with Alzheimer’s and Lewy body dementia, including communication strategies and coping mechanisms, empowers caregivers to provide the best possible care.
Training and resources to assist caregivers with practical tasks, such as meal preparation, medication reminders, and home modifications, can significantly enhance their ability to manage their responsibilities.
Illustrative Case Studies
Understanding the nuanced differences between Alzheimer’s disease and Lewy body dementia often requires careful examination of individual cases. These case studies provide a glimpse into the varied presentations of these conditions, highlighting the complexities in diagnosis and management. By exploring the symptoms, cognitive profiles, and physical examination findings, we can better appreciate the distinctive features that aid in differentiation.
Case Study 1: Alzheimer’s Disease
This hypothetical case involves a 72-year-old woman, Mrs. Smith, who has been experiencing progressive memory loss over the past two years. Initially, her forgetfulness was subtle, affecting recent events and appointments. As the condition progressed, she began exhibiting difficulty with language, struggling to find the right words and following conversations. Her cognitive function deteriorated further, affecting her ability to perform daily tasks like cooking and dressing.
She also displayed signs of disorientation, getting lost in familiar surroundings. Physical examination revealed no significant motor deficits, but subtle impairments in executive functions, such as planning and problem-solving, were noted. Her mood remained relatively stable, with occasional episodes of mild anxiety.
Case Study 2: Lewy Body Dementia
Mr. Jones, a 68-year-old man, presents with a unique constellation of symptoms. His initial complaint was of fluctuating cognitive abilities. One day, he might be sharp and engaged in conversation, while the next, he would exhibit periods of confusion and disorientation. This fluctuation is a hallmark feature of Lewy body dementia.
He also displayed visual hallucinations, reporting seeing people or animals that were not present. His gait was unsteady, with a shuffling pattern and difficulty initiating movement. He experienced pronounced fluctuations in alertness and attention, often falling asleep abruptly during conversations. Physical examination revealed rigidity in his muscles, a hallmark of Parkinsonism.
Comparison of Case Studies
| Characteristic | Alzheimer’s Disease (Mrs. Smith) | Lewy Body Dementia (Mr. Jones) |
|---|---|---|
| Onset | Gradual, insidious | Variable, with fluctuations |
| Cognitive Function | Progressive decline in memory, language, and executive functions; relatively stable mood | Fluctuating cognition, with periods of clarity and confusion; visual hallucinations; often accompanied by Parkinsonian features |
| Motor Function | Generally preserved, with subtle executive function impairments | Parkinsonian features (rigidity, shuffling gait, difficulty initiating movement); often prominent motor symptoms |
| Hallucinations | Rare | Common, especially visual |
| Sleep Disturbances | Mild | Prominent, including REM sleep behavior disorder |
| Mood | Relatively stable | Can be labile, with episodes of depression or anxiety |
Diagnostic Considerations
Differentiating between Alzheimer’s and Lewy body dementia necessitates a comprehensive assessment, including detailed patient history, cognitive testing, and neurological examination. Neuroimaging, such as CT or MRI scans, can help rule out other causes of dementia. Neuropsychological testing is essential to evaluate specific cognitive domains, and the pattern of cognitive deficits helps in distinguishing the two conditions. A detailed evaluation of the patient’s motor function and presence of Parkinsonian features is critical.
Furthermore, the presence or absence of hallucinations, fluctuations in cognition, and sleep disturbances can significantly aid in reaching a definitive diagnosis.
Impact on Daily Life
Dementia, encompassing conditions like Alzheimer’s and Lewy Body Dementia, significantly impacts daily life, affecting not only the individual but also their loved ones. The progressive nature of these conditions necessitates adapting to changing abilities and limitations, requiring significant adjustments to routines, environments, and social interactions. Understanding the challenges and implementing supportive strategies are crucial for maintaining quality of life for both the person with dementia and their caregivers.The impact of dementia varies greatly depending on the specific type, progression rate, and individual coping mechanisms.
While some individuals may experience subtle changes early on, others may face rapid decline. This variability necessitates a flexible and adaptable approach to support and care. This section will explore the effects on daily activities, social interactions, and relationships, outlining challenges and providing practical strategies for adaptation.
Challenges in Daily Activities
The cognitive and functional decline associated with dementia impacts various daily activities. Memory loss, difficulty with language, and impaired judgment affect tasks like meal preparation, medication management, and personal hygiene. Simple actions that were once routine can become overwhelming or unsafe.
- Meal Preparation and Eating: Difficulty remembering steps in a recipe, recognizing food items, or safely using utensils are common challenges. This can lead to malnutrition and a decline in overall health.
- Medication Management: Remembering to take medications at the correct time and dosage can become increasingly difficult. This requires careful monitoring and support systems, including medication reminders and assistance with administration.
- Personal Hygiene: Tasks like bathing, dressing, and toileting may become challenging as cognitive and physical abilities diminish. Caregivers must provide appropriate support and guidance while ensuring safety and dignity.
Social Interactions and Relationships
Dementia can significantly alter social interactions and relationships. Communication difficulties, changes in personality, and behavioral issues can strain relationships with family members, friends, and community members. Maintaining connections becomes challenging for both the individual with dementia and their loved ones.
- Communication Difficulties: The individual may struggle to express themselves clearly or understand others. Misunderstandings and frustration can arise, affecting communication and social engagement. Finding alternative methods of communication, like using visual aids or nonverbal cues, can be beneficial.
- Changes in Personality and Behavior: Dementia can lead to mood swings, agitation, or unusual behaviors. These changes can be distressing for the individual and challenging for caregivers, requiring patience, understanding, and appropriate strategies to manage these behaviors.
- Relationship Strain: As dementia progresses, the individual may exhibit behaviors that strain relationships with family and friends. Open communication, empathy, and understanding are vital for navigating these challenges.
Adapting Daily Routines and Environments
Adapting daily routines and environments is essential for maintaining quality of life for individuals with dementia. Creating a safe and supportive environment can significantly improve their well-being and reduce stress for caregivers.
- Routine and Structure: Establishing a consistent daily routine can provide a sense of predictability and security for individuals with dementia. Structured activities, like scheduled meals, outings, and relaxation periods, can be helpful.
- Environmental Modifications: Modifying the home environment to promote safety and reduce confusion is crucial. This may involve installing grab bars, removing tripping hazards, and using visual cues to enhance orientation.
- Support Systems: Enlisting the support of family, friends, and community resources can ease the burden on caregivers and provide necessary assistance for individuals with dementia. This may include respite care, support groups, and professional services.
Closing Notes
In conclusion, while both Alzheimer’s and Lewy body dementia are devastating forms of dementia, understanding their unique characteristics is vital for accurate diagnosis and personalized care. The subtle yet significant differences in symptom presentation, progression, and diagnostic criteria demand a nuanced approach to treatment and support. By exploring these distinctions, we gain a deeper appreciation for the challenges faced by individuals and families navigating this complex health landscape.




