Diastolic dysfunction and diastolic heart failure p2 delves into the intricacies of this often-overlooked form of heart failure. We’ll explore the subtle yet significant symptoms, differentiate them from systolic heart failure, and examine the underlying pathophysiology of impaired relaxation and filling in the left ventricle.
This in-depth exploration covers diagnostic methods, from echocardiography to cardiac catheterization, and the crucial role of biomarkers like natriuretic peptides. We’ll also examine the risk factors, including hypertension and diabetes, and discuss current management strategies, including pharmacological interventions and lifestyle modifications. Finally, we’ll consider prognosis, potential complications, and future research directions.
Introduction to Diastolic Dysfunction and Diastolic Heart Failure (p2)
Diastolic dysfunction is a critical aspect of heart failure, often overlooked compared to the more readily recognized systolic dysfunction. It represents a condition where the heart’s left ventricle, the chamber responsible for pumping oxygenated blood to the body, struggles to relax and fill properly during diastole (the heart’s resting phase). This impaired relaxation and filling can lead to a buildup of pressure in the heart, ultimately causing the symptoms of diastolic heart failure.The underlying pathophysiology of diastolic dysfunction encompasses a complex interplay of factors.
Key mechanisms involve stiffening of the left ventricular walls, a condition known as myocardial hypertrophy, and impaired relaxation of the heart muscle itself. These changes disrupt the normal filling process, leading to reduced stroke volume and eventually, reduced cardiac output. This, in turn, impacts the body’s ability to meet its oxygen demands.
Clinical Presentation of Diastolic Heart Failure
Diastolic heart failure often presents with subtle symptoms that can be easily misdiagnosed, especially in the early stages. Patients may experience fatigue, shortness of breath, particularly when lying down (orthopnea), and persistent cough. Important to note, these symptoms can overlap with other conditions, making early detection challenging. Furthermore, the clinical presentation of diastolic heart failure can differ significantly from systolic heart failure, where the heart struggles to contract effectively.
This distinction is crucial for appropriate diagnosis and treatment.
Key Differences Between Diastolic and Systolic Heart Failure
Understanding the nuances between diastolic and systolic heart failure is critical for accurate diagnosis and tailored treatment. The table below highlights the key distinctions.
| Feature | Diastolic Heart Failure | Systolic Heart Failure |
|---|---|---|
| Ventricular Contraction | Normal or near-normal | Impaired |
| Ventricular Relaxation | Impaired | Normal |
| Left Ventricular Filling | Reduced | Normal |
| Left Ventricular Pressure | Increased | Increased |
| Stroke Volume | Reduced | Reduced |
| Symptoms | Often subtle, fatigue, shortness of breath, orthopnea, cough | More pronounced, shortness of breath, edema, fatigue |
| Ejection Fraction (EF) | Usually preserved (above 40%) | Reduced (below 40%) |
Diastolic dysfunction can manifest in various individuals, impacting their daily lives significantly. This disparity in symptom presentation highlights the importance of thorough patient evaluation and careful consideration of individual patient histories.
Diagnostic Evaluation
Understanding diastolic dysfunction and its progression to diastolic heart failure requires a comprehensive diagnostic approach. This involves a careful evaluation of symptoms, risk factors, and a battery of tests to identify the underlying impairment of the heart’s ability to relax and fill properly. Accurate diagnosis is crucial for effective management and prognosis.
Echocardiography
Echocardiography is a cornerstone of diagnosing diastolic dysfunction. This non-invasive technique uses ultrasound waves to create images of the heart’s structure and function. Specific parameters evaluated include left ventricular filling pressures, mitral inflow patterns, and tissue Doppler imaging. These measurements provide insights into the heart’s relaxation and filling capabilities, helping to distinguish diastolic dysfunction from other cardiac conditions.
Digging deeper into diastolic dysfunction and diastolic heart failure p2, understanding the impact of lifestyle factors is key. A crucial aspect of this is maintaining a healthy weight. Knowing your Body Mass Index (BMI) can be helpful in assessing your risk factors, and a handy BMI chart for women can be found here. Ultimately, a comprehensive approach, considering both lifestyle choices and medical interventions, is vital for managing diastolic dysfunction and diastolic heart failure p2 effectively.
Echocardiography can also identify structural abnormalities that may contribute to diastolic dysfunction, such as thickened ventricular walls or valve abnormalities. It’s an essential tool for both initial diagnosis and ongoing monitoring of the disease.
Other Imaging Techniques
While echocardiography is paramount, other imaging techniques may complement the evaluation. Cardiac MRI (magnetic resonance imaging) can provide detailed anatomical images of the heart, enabling a comprehensive assessment of ventricular structure and function. Contrast-enhanced cardiac MRI can further refine the evaluation of diastolic function by highlighting areas of impaired relaxation. Radionuclide imaging techniques, like myocardial perfusion scans, may be used in specific cases to assess myocardial viability and the extent of any associated coronary artery disease.
Cardiac Catheterization
Cardiac catheterization, while often reserved for more complex cases or when echocardiography findings are inconclusive, plays a role in evaluating diastolic dysfunction. It involves inserting a catheter into a blood vessel, typically in the groin, and threading it to the heart. Measurements of pressure gradients across the heart valves and chambers, particularly during the filling phase, can provide precise information on diastolic function.
This procedure is typically performed in specialized cardiac catheterization labs, with careful consideration of patient risks.
Biomarkers
Natriuretic peptides, such as BNP (brain natriuretic peptide) and NT-proBNP (N-terminal pro-B-type natriuretic peptide), are valuable biomarkers for diagnosing and monitoring heart failure, including diastolic heart failure. Elevated levels of these peptides can reflect the stress on the heart and the presence of diastolic dysfunction. However, it’s important to note that elevated natriuretic peptide levels can also be seen in other conditions, so their interpretation should be combined with other clinical findings and diagnostic tests.
These biomarkers are often helpful in assessing disease severity and guiding treatment decisions.
Comparison of Diagnostic Tests
| Diagnostic Test | Sensitivity | Specificity | Advantages | Disadvantages |
|---|---|---|---|---|
| Echocardiography | High | High | Non-invasive, readily available, provides structural and functional information | Operator dependence, limited assessment of global diastolic function in some cases |
| Cardiac MRI | High | High | Detailed anatomical and functional information, excellent for assessing myocardial structure and function | More expensive, not readily available everywhere, potential for claustrophobia |
| Cardiac Catheterization | High | High | Direct measurement of pressure gradients, highly specific | Invasive procedure, carries risks, expensive |
| Natriuretic Peptides | Moderate | Moderate | Non-invasive, easily measurable, helpful in assessing disease severity and monitoring | Can be elevated in other conditions, not diagnostic alone |
Note: Sensitivity and specificity values can vary depending on the specific patient population and the criteria used for diagnosis.
Risk Factors and Associated Conditions
Diastolic dysfunction, the inability of the heart’s ventricles to relax and fill properly, often precedes the development of heart failure. Understanding the factors that contribute to this condition is crucial for early detection and preventative measures. Identifying risk factors and associated conditions allows for proactive management and potentially delays or prevents the progression to diastolic heart failure.
Risk Factors for Diastolic Dysfunction
Several factors increase the likelihood of developing diastolic dysfunction. Age-related changes in the heart’s structure and function are a major contributor. The heart muscle stiffens, and the elasticity of the heart valves and chambers diminishes, hindering their ability to relax and fill with blood. Furthermore, a sedentary lifestyle, characterized by a lack of physical activity, negatively impacts cardiovascular health, contributing to the development of diastolic dysfunction.
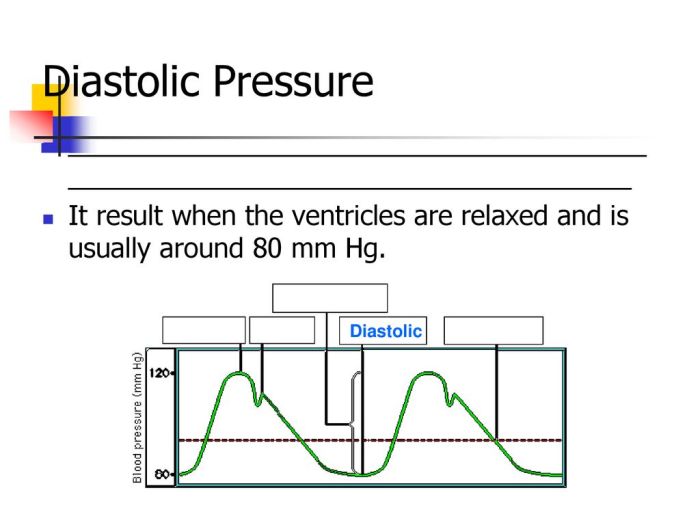
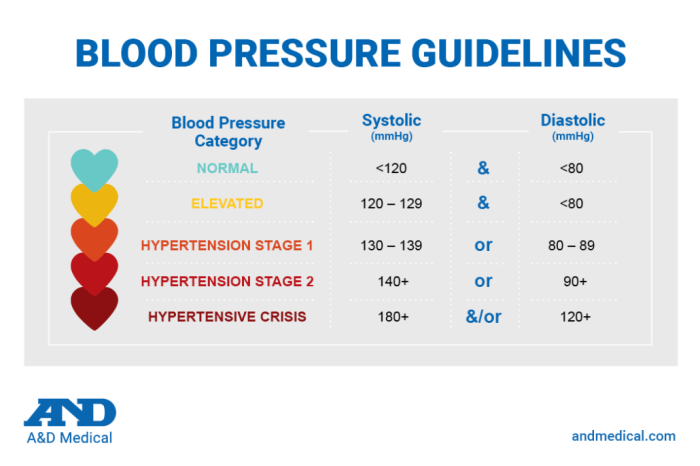
Connection Between Hypertension and Diastolic Dysfunction
Hypertension, or high blood pressure, is a significant risk factor for diastolic dysfunction. Persistent high blood pressure forces the heart to work harder to pump blood, leading to increased pressure within the heart chambers. This increased pressure can cause the heart muscle to become stiff and less compliant, thereby hindering the heart’s ability to relax and fill adequately.
Patients with uncontrolled hypertension are at a substantially higher risk of developing diastolic dysfunction.
Connection Between Diabetes and Diastolic Dysfunction
Diabetes mellitus, particularly type 2, is strongly associated with diastolic dysfunction. Chronic hyperglycemia, a hallmark of diabetes, can lead to vascular damage and increased stiffness of the heart muscle. This, in turn, impacts the heart’s ability to relax and fill with blood effectively, contributing to the development of diastolic dysfunction. The complex interplay of metabolic dysregulation and vascular changes in diabetes increases the risk of this condition.
Other Comorbidities and Diastolic Dysfunction, Diastolic dysfunction and diastolic heart failure p2
Various other medical conditions can elevate the risk of diastolic dysfunction. Obesity, characterized by excessive body fat, places additional strain on the cardiovascular system, potentially leading to heart muscle stiffening and impaired relaxation. Chronic kidney disease can affect the body’s ability to regulate blood pressure and fluid balance, further increasing the risk of diastolic dysfunction. Similarly, conditions such as sleep apnea and thyroid disorders can indirectly contribute to heart muscle stiffness and impaired relaxation.
Age, Lifestyle Factors, and Progression
The interplay of age, lifestyle factors, and the progression of diastolic dysfunction is a complex one. As individuals age, their heart muscle naturally undergoes changes that reduce its ability to relax. Combined with a sedentary lifestyle, poor dietary habits, and lack of regular exercise, these factors accelerate the development and progression of diastolic dysfunction. The progression may be gradual, often without noticeable symptoms in the early stages.
However, as the condition advances, symptoms such as shortness of breath, fatigue, and edema become more pronounced. For example, a 65-year-old individual with a history of hypertension and diabetes, who is also sedentary and obese, has a significantly higher risk of developing diastolic dysfunction than someone with a healthy lifestyle and no comorbidities.
Summary Table: Risk Factors for Diastolic Dysfunction
| Risk Factor | Potential Impact | Modifiable Strategies |
|---|---|---|
| Hypertension | Increased pressure on the heart, leading to stiffening and impaired relaxation. | Medication adherence, lifestyle modifications (diet, exercise, stress management). |
| Diabetes | Chronic hyperglycemia damages blood vessels and heart muscle, impacting relaxation. | Maintaining blood sugar control, healthy diet, exercise. |
| Obesity | Increased strain on the cardiovascular system, potentially leading to heart muscle stiffening. | Weight management, healthy diet, exercise. |
| Age | Natural changes in heart structure and function reduce elasticity and relaxation. | Adopting a healthy lifestyle to mitigate age-related effects. |
| Sedentary Lifestyle | Lack of physical activity contributes to increased risk of cardiovascular issues, impacting relaxation. | Regular exercise, increased physical activity. |
| Smoking | Damages blood vessels, increasing risk of stiffening and impacting relaxation. | Smoking cessation. |
Management Strategies
Managing diastolic dysfunction and diastolic heart failure involves a multifaceted approach that focuses on both pharmacological interventions and lifestyle modifications. The goal is to improve diastolic function, reduce symptoms, and prevent progression to more severe heart failure. A crucial component of this management is close monitoring and follow-up to adjust treatment strategies as needed.
Diving deeper into diastolic dysfunction and diastolic heart failure p2, it’s crucial to understand the broader health disparities. For example, factors like socioeconomic status and access to healthcare can significantly impact health outcomes, particularly for the Latinx community, and their risk for HIV. Understanding the latinx and hiv risk gap effects know your status is vital for comprehensive healthcare strategies.
This knowledge helps us better tailor preventative measures and treatment plans to address the unique challenges faced by this community, ultimately improving the outcomes for those dealing with diastolic dysfunction and diastolic heart failure p2.
Pharmacological Interventions
Current pharmacological therapies for diastolic dysfunction and diastolic heart failure primarily aim to address underlying conditions contributing to the impaired relaxation of the heart muscle. These medications can help manage blood pressure, heart rate, and other risk factors. Specific drugs target the underlying mechanisms of diastolic dysfunction, such as reducing afterload, improving myocardial relaxation, and reducing inflammation.
Lifestyle Modifications
Implementing lifestyle changes plays a vital role in improving diastolic function and overall cardiovascular health. Adopting a heart-healthy lifestyle can significantly reduce the strain on the heart, potentially slowing or halting the progression of diastolic dysfunction. Crucially, these modifications address the root causes of the condition, fostering long-term improvements in cardiac health.
- Dietary Modifications: A balanced diet low in sodium, saturated fats, and cholesterol is essential. Reducing processed foods, sugary drinks, and excessive alcohol consumption is crucial. Increasing intake of fruits, vegetables, and whole grains supports overall health and contributes to better heart function.
- Regular Exercise: Engaging in regular moderate-intensity aerobic exercise, such as brisk walking, swimming, or cycling, strengthens the heart muscle and improves blood circulation. Consult a healthcare professional for a personalized exercise plan.
- Stress Management: Chronic stress can negatively impact heart health. Adopting stress-reduction techniques, such as meditation, yoga, or deep breathing exercises, is beneficial for both mental and physical well-being.
- Smoking Cessation: Smoking significantly increases the risk of cardiovascular diseases. Quitting smoking is a crucial step in improving overall heart health and potentially mitigating the progression of diastolic dysfunction.
Close Monitoring and Follow-up
Regular monitoring and follow-up appointments are essential for managing diastolic heart failure. This allows healthcare providers to assess the effectiveness of treatment, detect any changes in the condition, and adjust the management plan accordingly. Monitoring includes blood pressure, heart rate, and symptoms assessment, along with regular blood tests to assess organ function.
Medication Overview
The following table summarizes common medications used in the management of diastolic dysfunction and diastolic heart failure, outlining their mechanisms of action, potential side effects, and patient education considerations.
| Medication | Mechanism of Action | Potential Side Effects | Patient Education Considerations |
|---|---|---|---|
| Beta-blockers | Reduce heart rate and blood pressure, improving myocardial relaxation | Fatigue, dizziness, hypotension, bradycardia | Importance of gradual dose titration, monitoring for signs of hypotension, and avoiding sudden discontinuation. |
| ACE Inhibitors/ARBs | Reduce blood pressure and afterload, improving myocardial relaxation | Dry cough (ACE inhibitors), dizziness, hypotension, kidney dysfunction | Importance of monitoring for signs of kidney dysfunction, avoiding potassium-sparing diuretics, and monitoring blood pressure closely. |
| Diuretics | Reduce fluid volume, decreasing strain on the heart | Dehydration, electrolyte imbalances (hypokalemia), dizziness | Importance of monitoring for electrolyte imbalances, encouraging adequate fluid intake between doses, and regular weight monitoring. |
| Calcium Channel Blockers | Reduce heart rate and blood pressure, improving myocardial relaxation | Dizziness, headache, edema, constipation | Importance of monitoring for hypotension, edema, and avoiding grapefruit juice. |
Prognosis and Complications: Diastolic Dysfunction And Diastolic Heart Failure P2
Diastolic heart failure, while often less dramatic than systolic heart failure, can still significantly impact a person’s quality of life and longevity. Understanding the prognosis, potential complications, and strategies to mitigate these risks is crucial for both patients and healthcare providers. Factors like the severity of diastolic dysfunction, presence of comorbidities, and adherence to treatment play a significant role in shaping the long-term outlook.The prognosis for individuals with diastolic heart failure is often influenced by the severity of the condition and the presence of other health problems.
While a complete cure isn’t typically possible, effective management can significantly improve the patient’s ability to maintain an active and fulfilling life. This involves addressing both the underlying causes and the symptoms that arise from the compromised heart function.
Impact of Comorbidities
Comorbidities, or co-existing medical conditions, are a key determinant in the prognosis of diastolic heart failure. Conditions like hypertension, diabetes, obesity, and coronary artery disease often coexist and exacerbate the heart’s inability to relax and fill properly. These conditions contribute to the progression of diastolic dysfunction and can negatively affect the overall health and well-being of the patient.
For example, uncontrolled hypertension significantly strains the heart, making it harder for the left ventricle to relax and fill with blood. Similarly, diabetes can lead to microvascular damage, impacting the heart’s ability to function optimally.
Diving deeper into diastolic dysfunction and diastolic heart failure p2, it’s crucial to understand the potential connections to other health issues. Sometimes, symptoms like pain behind the eye can be a red flag , though less directly related to the mechanics of diastolic dysfunction. However, a thorough understanding of the broader physiological picture is vital for effective management and treatment of diastolic dysfunction and diastolic heart failure p2.
Treatment Adherence and Patient Outcomes
Patient adherence to prescribed medications and lifestyle modifications is paramount in managing diastolic heart failure. Consistent medication intake and a healthy lifestyle, including a balanced diet, regular exercise, and stress management, directly impact the progression of the condition. A patient who diligently follows their prescribed treatment plan is more likely to experience a positive outcome, reducing the risk of complications and maintaining a higher quality of life.
Potential Complications
Diastolic heart failure can lead to a range of complications, impacting various organ systems. These complications are often linked to the progressive nature of the condition and the strain it places on the heart.
- Cardiovascular complications: The inability of the heart to relax and fill properly can lead to reduced blood flow to vital organs, causing angina, shortness of breath, and fatigue. A prolonged and uncontrolled condition can further lead to congestive heart failure. Chronic heart failure can lead to severe and potentially life-threatening consequences.
- Renal complications: Reduced blood flow to the kidneys can impair their function, leading to kidney disease and fluid retention. This can further exacerbate the heart’s workload, creating a vicious cycle.
- Neurological complications: Reduced blood flow to the brain can cause cognitive impairment, memory problems, and even stroke. Symptoms can include confusion, dizziness, and headaches.
- Pulmonary complications: Fluid buildup in the lungs (pulmonary edema) can lead to difficulty breathing, shortness of breath, and coughing. This is a significant concern as it directly impacts the patient’s quality of life and can be life-threatening if not managed properly.
Strategies for Improving Patient Outcomes
Effective management of diastolic heart failure requires a multi-faceted approach that focuses on both medical treatment and lifestyle modifications. Early detection, adherence to treatment plans, and proactive management of comorbid conditions are crucial for improving patient outcomes and enhancing quality of life.
- Close monitoring: Regular check-ups, including cardiac evaluations, blood tests, and monitoring of vital signs, are essential for early detection of any worsening symptoms or complications.
- Medication adherence: Patients need to understand the importance of taking prescribed medications as directed and report any side effects promptly.
- Lifestyle modifications: Adopting a healthy lifestyle, including a balanced diet, regular exercise, weight management, and stress reduction techniques, plays a crucial role in slowing the progression of diastolic heart failure.
- Support groups: Support groups can provide valuable emotional and practical support to patients and their families, helping them navigate the challenges associated with the condition.
Prognosis for diastolic heart failure is often influenced by comorbidities and treatment adherence. Potential complications include cardiovascular, renal, neurological, and pulmonary issues. Improving patient outcomes requires close monitoring, medication adherence, lifestyle modifications, and support systems.
Illustrative Case Studies
Understanding diastolic heart failure requires delving into real-world scenarios. Case studies provide valuable insights into the diagnostic journey, management approaches, and the impact of various factors on patient outcomes. These examples illustrate the complexities of this condition and highlight the importance of personalized care.
Case Study 1: A Patient Presenting with Diastolic Heart Failure
A 65-year-old female patient presented with increasing shortness of breath, especially at night (paroxysmal nocturnal dyspnea), and fatigue. She had a history of hypertension and hyperlipidemia, both poorly controlled. Physical examination revealed an elevated blood pressure of 160/95 mmHg and mild peripheral edema. An echocardiogram revealed a normal left ventricular ejection fraction (LVEF) but evidence of diastolic dysfunction, characterized by impaired relaxation and increased left ventricular stiffness.
Further diagnostic testing included a comprehensive metabolic panel, which showed elevated cholesterol and creatinine levels, and an electrocardiogram (ECG), which indicated left atrial enlargement. The management plan included aggressive blood pressure control with a combination of medications, such as an ACE inhibitor and a beta-blocker, along with lifestyle modifications, including a low-sodium diet, regular exercise, and smoking cessation.
The patient’s response to treatment was monitored closely through serial echocardiograms and blood pressure measurements. Patient education focused on the importance of medication adherence, lifestyle modifications, and the recognition of worsening symptoms. She was instructed to monitor her weight, blood pressure, and pulse, and to contact her physician immediately if symptoms worsened.
Case Study 2: Impact of Hypertension on Diastolic Dysfunction
A 58-year-old male patient with a long-standing history of uncontrolled hypertension presented with progressive dyspnea on exertion and palpitations. Physical examination revealed elevated blood pressure (180/110 mmHg), and auscultation revealed an S4 heart sound, indicative of increased left ventricular stiffness. Diagnostic testing revealed evidence of significant diastolic dysfunction on echocardiography. The patient’s echocardiogram revealed evidence of left ventricular hypertrophy, a common consequence of chronic hypertension.The management plan emphasized aggressive blood pressure control to reduce the strain on the heart.
This included medication adjustments to achieve optimal blood pressure targets, and a focus on lifestyle modifications such as a low-sodium diet and regular exercise. Patient education emphasized the critical link between uncontrolled hypertension and diastolic dysfunction, and the importance of consistent medication adherence and lifestyle changes. Close monitoring of blood pressure and symptom progression was essential.
Case Study 3: Diastolic Dysfunction and Diabetes
A 62-year-old female patient with a history of type 2 diabetes and hypertension presented with persistent fatigue and mild edema. Physical examination revealed a blood pressure of 140/90 mmHg and mild peripheral edema. Diagnostic evaluation included an echocardiogram, revealing diastolic dysfunction. Further investigations revealed microalbuminuria, suggesting early diabetic nephropathy.The management plan integrated strategies to address both conditions.
Blood pressure control remained paramount, but careful selection of medications was crucial to avoid adverse effects on glucose control. Tight glycemic control through lifestyle modifications and possibly medication adjustments was implemented. Patient education emphasized the importance of a comprehensive approach to managing both diabetes and diastolic dysfunction, including regular blood glucose monitoring, blood pressure control, and a healthy diet.
The need for regular nephrology follow-up was also highlighted.
Hypothetical Case: Progressive Symptoms
A 70-year-old patient with a history of hypertension and mild coronary artery disease presented with progressively worsening dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea. Over several months, the patient experienced a gradual decline in functional capacity, limiting activities of daily living. Initial diagnostic evaluations showed evidence of diastolic dysfunction and mild left ventricular hypertrophy. As symptoms worsened, echocardiographic findings indicated a progressive decline in diastolic function and potential signs of left ventricular filling pressures increasing.
The management plan included optimizing blood pressure control with medication adjustments, regular cardiac monitoring, and careful consideration of potential heart failure therapies. Patient education emphasized the need for careful symptom monitoring and prompt medical intervention to prevent further deterioration. This case highlights the importance of recognizing and addressing the progressive nature of diastolic heart failure.
Future Directions in Research
Unraveling the complexities of diastolic dysfunction and heart failure remains a significant challenge, prompting ongoing research into the underlying mechanisms and potential therapeutic targets. This quest for understanding necessitates a multi-faceted approach encompassing basic science research, clinical trials, and the exploration of novel diagnostic and treatment modalities. The future of research in this area hinges on identifying effective preventative strategies and improving the lives of those affected.Current research gaps include a deeper understanding of the intricate interplay of genetic, environmental, and lifestyle factors in the development of diastolic dysfunction.
Moreover, the precise mechanisms driving the progressive nature of diastolic dysfunction, particularly in the context of comorbidities, are not fully elucidated. The need for reliable biomarkers to aid in early diagnosis and risk stratification remains a crucial area for investigation.
Research Gaps in Understanding Diastolic Dysfunction
Significant gaps exist in our understanding of the specific molecular and cellular mechanisms underlying diastolic dysfunction. Research needs to focus on elucidating the intricate interplay of various factors, including oxidative stress, inflammation, and the renin-angiotensin-aldosterone system, in the development and progression of diastolic dysfunction. This understanding is crucial for developing targeted therapies and preventative strategies. The variability in responses to current treatments across different patient populations necessitates further research to identify and personalize treatment approaches.
Future Research Directions in Potential Treatments
Future research should prioritize the development of novel therapies targeting the specific cellular and molecular pathways involved in diastolic dysfunction. This includes investigating the potential of pharmacologic agents that specifically address the impaired relaxation and contractility of the heart muscle. The role of epigenetic modifications in modulating cardiac function and the potential for epigenetic therapies to reverse or mitigate diastolic dysfunction deserve further exploration.
Importance of Ongoing Clinical Trials and Observational Studies
Large-scale, well-designed clinical trials are essential to validate and refine existing treatment strategies and evaluate the efficacy of novel therapies in preventing and treating diastolic dysfunction. Observational studies, particularly longitudinal studies following patients over time, are crucial for identifying risk factors, understanding disease progression, and evaluating the long-term outcomes of various interventions. These studies should include diverse patient populations to account for the varying clinical presentations and responses to treatments.
Furthermore, studies must evaluate the impact of lifestyle modifications, such as dietary changes and exercise regimens, on the progression of diastolic dysfunction.
Potential Impact of Novel Technologies on Diagnosis and Management
Novel technologies, such as advanced imaging techniques like cardiac MRI and echocardiography, can provide detailed information about the structure and function of the heart, enabling earlier and more precise diagnoses of diastolic dysfunction. These advanced techniques can also help monitor the progression of the disease and the effectiveness of treatments. Further development and implementation of digital health tools and wearable sensors, capable of continuous monitoring of cardiac function and lifestyle factors, could potentially enhance the management of diastolic dysfunction.
This includes the development of sophisticated algorithms for risk stratification and personalized treatment recommendations.
End of Discussion
In conclusion, diastolic heart failure, while often less dramatic than systolic failure, poses significant health challenges. Understanding its unique characteristics, diagnostic approaches, and management strategies is crucial for improving patient outcomes. This comprehensive overview provides a solid foundation for healthcare professionals and patients alike, highlighting the importance of early detection and proactive management.




