Diabetes and yeast infections are closely linked. Understanding this connection is crucial for effective management. This guide delves into the mechanisms behind this link, exploring the impact of blood sugar control, common symptoms, treatment options, and prevention strategies.
Diabetes often creates a favorable environment for yeast overgrowth, leading to recurrent infections. This article will examine the specifics of these infections in diabetic patients, differentiating them from yeast infections in non-diabetics, and emphasizing the importance of prompt and accurate diagnosis.
Overview of Diabetes and Yeast Infections
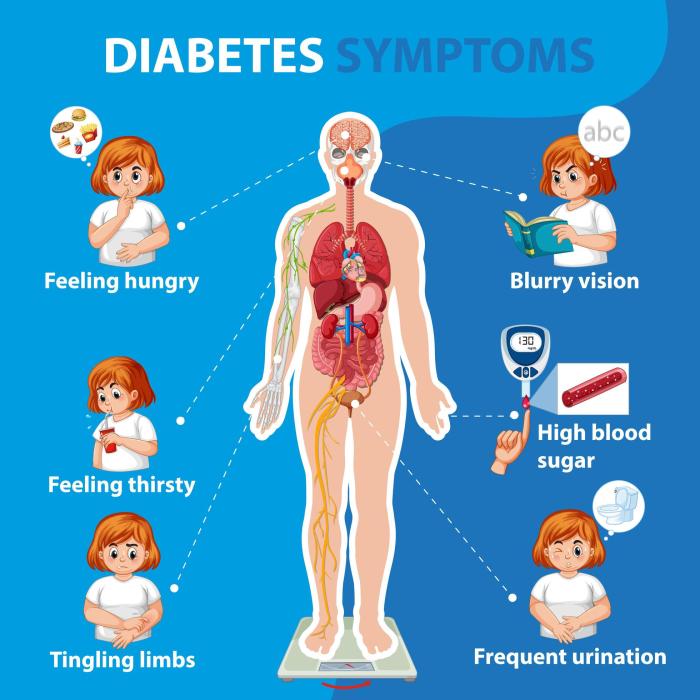
Diabetes significantly increases the risk of yeast infections, primarily due to the impact of high blood sugar levels on the body’s immune system and the environment conducive to yeast growth. Understanding this connection is crucial for effective management of both conditions. Proper blood sugar control plays a pivotal role in preventing these infections.
The Link Between Diabetes and Yeast Infections
High blood sugar levels, a hallmark of diabetes, create an ideal environment for yeast, particularlyCandida albicans*, to thrive. The excess glucose in the body, particularly in areas like the vagina and mouth, fuels the yeast’s rapid multiplication. This is compounded by a weakened immune response in individuals with diabetes, making them less capable of fighting off the infection.
This process ultimately leads to the development of yeast infections.
Dealing with diabetes can sometimes lead to pesky yeast infections, a common complication. Keeping your immune system strong is key, and that includes being mindful of how you care for your eyes. Using allergy eye drops, especially when wearing contact lenses, can sometimes disrupt the delicate balance of your eye’s environment, which can actually make you more susceptible to yeast infections.
For more insights on how to use allergy eye drops safely with contact lenses, check out this helpful guide on allergy eye drops and contact lenses. Ultimately, understanding how various factors can influence yeast infections in people with diabetes is important for managing your overall health.
Mechanisms of Increased Risk
Several mechanisms contribute to the elevated risk of yeast infections in individuals with diabetes. Elevated blood sugar levels provide a readily available nutrient source for yeast growth. High glucose levels also disrupt the normal pH balance in the vagina and other susceptible areas, creating a favorable environment for yeast overgrowth. Furthermore, compromised immune function, a consequence of diabetes, reduces the body’s ability to effectively combat yeast infections.
Consequently, these factors collectively increase the risk of recurrent or severe yeast infections.
Role of Blood Sugar Control
Maintaining stable blood sugar levels is essential in preventing yeast infections. By controlling blood glucose levels, individuals with diabetes can create a less hospitable environment for yeast to flourish. Consistent monitoring and management of blood sugar through diet, exercise, and medication are crucial in minimizing the risk of yeast infections. For example, a person with diabetes who consistently maintains healthy blood sugar levels through a well-balanced diet and regular exercise is less likely to experience yeast infections.
Types of Yeast Infections Commonly Associated with Diabetes
The most common type of yeast infection associated with diabetes is vaginal yeast infection. However, other areas such as the mouth (oral thrush) and the skin (intertrigo) can also be affected. In individuals with diabetes, yeast infections can exhibit more severe symptoms and may recur more frequently.
Symptoms Comparison
| Symptom | Diabetic | Non-Diabetic |
|---|---|---|
| Burning sensation | Often more intense and persistent | Mild to moderate |
| Itching | Often more intense and persistent | Mild to moderate |
| Discharge | May be thicker, whiter, and more profuse | Usually thin, white, or clear |
| Redness and swelling | May be more pronounced | Usually mild |
| Pain during urination | May be present | Less common or absent |
| Soreness | May be more pronounced | Mild to moderate |
Symptoms and Diagnosis: Diabetes And Yeast Infections
Yeast infections, a common complication for individuals with diabetes, can manifest differently than in those without the condition. Understanding these differences is crucial for prompt and accurate diagnosis, enabling timely and effective treatment. Early detection and management are vital to prevent complications and maintain overall health.Recognizing the symptoms and knowing how they might differ in diabetic patients is essential for seeking timely medical attention.
A thorough understanding of the diagnostic methods employed can help individuals with diabetes and their healthcare providers collaborate effectively in managing these infections.
Diabetes can sometimes lead to pesky yeast infections, a common issue. Finding the right birth control method is crucial, especially for nulliparous women considering options like the IUD, which has its own set of considerations. Learning about IUD use in nulliparous women can help navigate these choices and potentially reduce the risk of complications. This, in turn, can help manage diabetes-related yeast infections more effectively.
Common Symptoms of Yeast Infections in Diabetic Patients
Yeast infections in diabetic individuals often present with symptoms similar to those in non-diabetic patients, but the intensity and duration can vary. This is due to the impact of diabetes on the immune system, making individuals more susceptible to infections. Symptoms might include vaginal itching, burning, and redness. A thick, white, clumpy discharge is also frequently observed.
In some cases, the infection might extend beyond the vagina, causing pain during urination or intercourse. It is crucial to remember that these symptoms can also be indicative of other conditions, making accurate diagnosis critical.
Differences in Symptom Presentation
While the symptoms of yeast infections in diabetic and non-diabetic patients often overlap, there are subtle yet important differences. Diabetic individuals may experience more intense symptoms, or symptoms that last longer. This is because high blood sugar levels can create a more conducive environment for yeast overgrowth. Additionally, the presence of other underlying health conditions associated with diabetes can influence the presentation of symptoms.
Therefore, it’s vital to consider these differences when assessing symptoms and seeking medical attention.
Diagnostic Methods for Yeast Infections in Diabetic Patients
Diagnosis of yeast infections typically involves a physical examination by a healthcare provider. Visual inspection of the affected area can reveal characteristic signs of inflammation, redness, and discharge. A sample of the discharge may be collected for laboratory analysis to confirm the presence of yeast. The laboratory analysis helps identify the specific type of yeast causing the infection and determine the most effective treatment.
This process ensures accurate identification of the infection and avoids misdiagnosis, which can lead to ineffective treatment and potential complications.
Importance of Accurate Diagnosis, Diabetes and yeast infections
Accurate diagnosis is crucial for effective management of yeast infections in individuals with diabetes. Misdiagnosis can lead to delayed treatment, potentially worsening the infection and increasing the risk of complications. This is especially important in diabetes because uncontrolled yeast infections can impact blood sugar control and overall well-being. Prompt and accurate diagnosis allows healthcare providers to prescribe the appropriate antifungal medication, minimizing discomfort and preventing further complications.
Potential Symptoms and Likelihood of Yeast Infection in Diabetic Patients
| Symptom | Likelihood | Possible Alternatives |
|---|---|---|
| Vaginal itching and burning | High | Allergic reactions, other infections (bacterial vaginosis, trichomoniasis) |
| Thick, white, clumpy discharge | High | Other vaginal infections, certain medications |
| Redness and swelling of the vaginal area | Moderate | Other inflammatory conditions, irritation from hygiene products |
| Pain during urination or intercourse | Moderate | Urinary tract infections, other pelvic pain conditions |
| No noticeable symptoms | Low | Yeast infection present but not causing noticeable symptoms, other infections |
Treatment and Management
Managing yeast infections in diabetic individuals requires a multifaceted approach that addresses both the infection itself and the underlying condition. Proper treatment, coupled with lifestyle modifications, plays a crucial role in preventing recurrence and improving overall health. Effective management involves understanding the various treatment options available and their respective advantages and disadvantages.Yeast infections in diabetic patients often require a more proactive and sustained approach compared to those without diabetes.
This is because uncontrolled blood sugar levels can create an environment conducive to yeast overgrowth. Therefore, effective treatment must consider both the infection and the individual’s overall diabetic management.
Common Treatments for Yeast Infections
Various treatments are available for yeast infections, ranging from over-the-counter medications to prescription drugs and lifestyle changes. Choosing the appropriate treatment depends on factors such as the severity of the infection, the individual’s medical history, and their response to previous treatments. Over-the-counter antifungal creams and suppositories, containing clotrimazole or miconazole, are often effective for mild to moderate infections.
Prescription-strength antifungal medications, including oral medications, may be necessary for more severe infections or recurrent issues.
Comparison of Treatment Options
Over-the-counter (OTC) medications are generally safe and effective for mild yeast infections, but they may not be sufficient for more persistent or severe cases. These options are often affordable and readily available, making them a convenient first-line treatment. Prescription medications, on the other hand, often provide a more potent antifungal effect, allowing for quicker resolution of the infection.
They may be necessary when OTC treatments prove ineffective or in cases of recurrent infections. Lifestyle modifications are crucial in preventing recurrent infections.
Importance of Adherence to Treatment Plans
Adherence to the prescribed treatment plan is essential for successful management of yeast infections in diabetic individuals. Consistent use of medications, as directed by a healthcare professional, is critical to ensure the infection is fully eradicated and prevent recurrence. Failure to adhere to the prescribed treatment can lead to persistent infections, potentially causing discomfort and complications.
Lifestyle Modifications for Reducing Recurrence
Lifestyle modifications play a pivotal role in reducing the risk of recurrent yeast infections in diabetic patients. Maintaining good blood sugar control is paramount. This often involves regular blood glucose monitoring, a healthy diet, and consistent physical activity.
Lifestyle Changes to Minimize Yeast Infections
- Maintaining Optimal Blood Sugar Control: Regular blood glucose monitoring, consistent medication adherence, and a healthy diet are crucial for preventing yeast overgrowth. Monitoring blood glucose levels allows for early identification and correction of hyperglycemia, thereby reducing the environment that promotes yeast infections. Consistent adherence to prescribed medications and lifestyle changes plays a significant role in preventing recurrent infections.
- Maintaining Good Hygiene: Maintaining good hygiene practices, such as regularly cleaning the genital area with mild soap and water, can prevent the buildup of moisture and bacteria, which can contribute to yeast overgrowth. Gentle cleansing is essential to avoid irritation and further complications.
- Wearing Breathable Clothing: Wearing breathable clothing, especially in the genital area, helps prevent moisture buildup and reduces the risk of yeast infection. This involves choosing fabrics that allow for proper air circulation and avoiding tight-fitting clothing.
- Avoiding Tight-Fitting Clothing: Avoid tight-fitting clothing, particularly in the genital area, as it can increase moisture and heat, fostering a favorable environment for yeast growth. Loose-fitting clothing is recommended to maintain appropriate air circulation and prevent the buildup of moisture.
- Managing Stress: Stress can affect blood sugar levels, which in turn can increase the risk of yeast infections. Practicing stress-reducing techniques, such as yoga, meditation, or deep breathing exercises, can help manage stress and maintain overall health.
Prevention Strategies
Yeast infections, a common complication for individuals with diabetes, can be effectively managed through proactive prevention strategies. Understanding the factors that contribute to these infections and implementing appropriate lifestyle adjustments are crucial for minimizing the risk and improving overall well-being. A holistic approach focusing on blood sugar control, hygiene, diet, and stress management is key.
Maintaining Optimal Blood Sugar Control
Consistent blood sugar management is paramount in preventing yeast infections. Elevated blood sugar levels create a favorable environment for yeast overgrowth. This is because high glucose levels in the body provide a readily available food source for yeast, enabling their rapid multiplication. By maintaining blood sugar levels within a healthy range, you reduce the fuel that yeast needs to proliferate.
Dealing with diabetes can sometimes lead to tricky yeast infections, a common issue for many. While these infections are often manageable, it’s important to consider the broader health picture. Sometimes, severe illnesses like meningitis can have lasting impacts, as explored in this article about long term effects meningitis. Fortunately, with proper care and management, diabetes and yeast infections can be effectively controlled, allowing for a healthier life.
Regular monitoring, medication adherence, and dietary adjustments play a vital role in achieving and sustaining this control.
Personal Hygiene Practices
Maintaining good hygiene is essential in reducing the risk of yeast infections. Proper cleansing and drying of the genital area is critical. Avoid harsh soaps and excessive scrubbing, as these can disrupt the natural pH balance and increase the risk of irritation. Focus on gentle cleansing with water or a mild, unscented soap, followed by thorough drying.
Using cotton underwear is recommended, as it allows for better air circulation and prevents moisture buildup, a breeding ground for yeast.
Dietary Considerations
Dietary changes can significantly impact yeast infection risk in individuals with diabetes. A diet rich in fiber and low in simple sugars is crucial. Fiber aids in regulating blood sugar levels, reducing the chances of yeast overgrowth. Examples of fiber-rich foods include fruits, vegetables, and whole grains. Limiting sugary foods and drinks is equally important.
Sugary foods and drinks provide readily available nutrients for yeast to thrive. Instead, choose complex carbohydrates, which are broken down more slowly, helping to maintain steady blood sugar levels.
Stress Management Techniques
Stress can impact blood sugar control, making individuals more susceptible to yeast infections. Chronic stress can lead to fluctuations in blood sugar levels, increasing the risk of yeast overgrowth. Chronic stress disrupts the body’s natural hormone balance, impacting insulin sensitivity and blood glucose regulation. Implementing stress management techniques, such as regular exercise, yoga, meditation, or spending time in nature, can significantly help in managing stress levels.
These practices help to reduce cortisol levels, promote relaxation, and support better blood sugar control.
Complications and Associated Issues

Untreated yeast infections can pose significant challenges for individuals with diabetes, potentially leading to more serious health problems. The delicate balance of the body’s immune system and the high blood sugar levels associated with diabetes can create an environment conducive to yeast overgrowth. Understanding these complications is crucial for effective management and prevention.
Potential Complications of Untreated Yeast Infections
Yeast infections, if left unaddressed, can escalate into more complex issues, particularly for individuals with diabetes. This is because the high blood sugar levels characteristic of diabetes can compromise the immune system’s ability to fight off infections, including yeast infections. This weakened immune response can allow the infection to spread and potentially affect other areas of the body.
Impact on Overall Health and Well-being
Persistent or recurrent yeast infections can significantly impact a person’s overall health and well-being. The discomfort and itching associated with these infections can disrupt sleep, cause emotional distress, and negatively affect quality of life. Moreover, the constant struggle with managing the infection can lead to feelings of frustration and anxiety. For instance, repeated episodes of vaginal yeast infections can lead to chronic vulvovaginal discomfort, impacting sexual activity and relationships.
Connection to Other Diabetic Complications
There’s a notable connection between yeast infections and other diabetic complications. The same factors that contribute to yeast overgrowth, such as high blood sugar levels and compromised immune function, can also increase the risk of developing other diabetic-related conditions. For example, poorly controlled blood sugar can lead to nerve damage (neuropathy), which can impair sensation in the affected area and potentially increase the risk of unnoticed skin breakdown, creating an ideal environment for yeast infection to take hold.
Importance of Early Intervention
Early detection and prompt treatment of yeast infections are crucial in preventing complications. By addressing the infection promptly, individuals can avoid the escalation of the problem into more severe conditions. Early intervention also minimizes the potential impact on overall health and well-being. The quicker the infection is treated, the less likely it is to spread and cause further complications.
Potential Complications Table
| Complication | Severity | Preventive Measures |
|---|---|---|
| Vulvovaginal Candidiasis (VVC) | Moderate to Severe | Maintaining good blood sugar control, practicing good hygiene, and using antifungal medications as prescribed. |
| Recurrent VVC | Moderate to Severe | Identifying and addressing underlying causes, such as uncontrolled diabetes, and consistently practicing preventive measures. |
| Disseminated Infection | Severe | Prompt diagnosis and treatment by a healthcare professional. Maintaining good blood sugar control is paramount. |
| Skin Infections | Moderate to Severe | Maintaining good skin hygiene, monitoring for signs of infection, and promptly seeking medical attention if necessary. |
| Systemic Infection | Severe | Immediate medical attention and aggressive treatment are essential. This often requires hospitalization and intensive care. |
Specific Considerations for Different Patient Populations
Managing yeast infections in individuals with diabetes requires careful consideration of various patient populations, each with unique needs and challenges. Different factors, such as age, physiological changes, and overall health conditions, influence how yeast infections manifest and how they should be treated. Understanding these variations is crucial for effective management and preventing complications.
Children
Children with diabetes are susceptible to yeast infections, often presenting with symptoms in different ways compared to adults. The developing immune system and potential for undiagnosed conditions can make diagnosis and treatment more complex. Proper communication with pediatricians and caregivers is essential for successful management. Addressing concerns about potential side effects of medications in young patients is crucial.
Pregnant Women
Pregnancy significantly impacts a woman’s body, including her immune system. Gestational diabetes, a temporary form of diabetes, further complicates the picture. Hormonal fluctuations and changes in blood sugar levels can increase the risk of yeast infections during pregnancy. Careful monitoring and adjusted treatment plans are necessary to ensure the safety of both the mother and the developing fetus.
Elderly Adults
Elderly individuals with diabetes may experience weakened immune systems and underlying health conditions that can affect their response to yeast infections. Chronic conditions, such as cognitive decline or mobility issues, can also hinder adherence to treatment regimens. Clear communication, simpler treatment plans, and caregiver support are crucial for effective management. A collaborative approach involving healthcare providers, caregivers, and the patient is vital.
Impact on Immune Response
Diabetes can negatively impact the immune system’s ability to fight off infections, including yeast infections. High blood sugar levels create an environment that favors yeast overgrowth. Weakened immune responses make individuals more susceptible to recurrent infections and more severe complications. Maintaining good blood sugar control is crucial for strengthening the immune response and preventing recurrent yeast infections.
This is often a significant factor in managing infections in these patient populations.
Resources for Patients
Several resources can help patients understand and manage yeast infections related to diabetes. Patient education materials, online support groups, and diabetes self-management education programs can provide valuable information and support. Consulting with healthcare providers and utilizing available resources are vital for effective management. Organizations like the American Diabetes Association (ADA) and the National Institutes of Health (NIH) offer valuable information.
Talking with your healthcare provider is also essential. They can offer personalized advice and support.
Outcome Summary
In conclusion, managing diabetes and yeast infections requires a multifaceted approach, combining blood sugar control, appropriate treatment, and preventive measures. Understanding the specific symptoms, diagnostic procedures, and available treatments is key to effectively controlling these infections. This comprehensive guide offers a roadmap for individuals with diabetes to navigate the challenges of yeast infections and maintain overall well-being.




