Diabetes and shortness of breath are often linked, but the precise mechanisms aren’t always clear. This exploration delves into the physiological connections, symptoms, diagnosis, management, and prevention strategies related to this often-overlooked complication. Understanding the interplay between diabetes and respiratory function is crucial for effective management and improved patient outcomes.
We’ll examine various types of diabetes and how they might impact breathing. We’ll also investigate potential triggers, common symptoms, and the importance of timely diagnosis and personalized treatment plans. The discussion will cover preventive measures, illustrative case studies, underlying conditions that can exacerbate the problem, and visual representations of the respiratory system to provide a comprehensive understanding of the issue.
Defining the Connection
Diabetes and shortness of breath, while seemingly unrelated, can be linked through a complex web of physiological mechanisms and complications. Understanding these connections is crucial for proper diagnosis and management. Often, shortness of breath in individuals with diabetes isn’t immediately attributed to the underlying condition, leading to delayed diagnosis and treatment. Recognizing the potential interplay is essential for prompt intervention.The interplay between diabetes and respiratory issues stems from a combination of direct and indirect effects.
Elevated blood sugar levels, a hallmark of diabetes, can impact various bodily systems, including the lungs and respiratory muscles. Moreover, long-term complications of diabetes can create significant challenges to breathing.
Physiological Mechanisms
Diabetes can affect the lungs and respiratory muscles in several ways. High blood sugar can lead to the accumulation of fluid in the lungs, a condition known as pulmonary edema. This fluid buildup hinders the lungs’ ability to properly expand and contract, leading to shortness of breath. Furthermore, diabetic neuropathy, a common complication, can damage the nerves controlling respiratory muscles, impacting their strength and efficiency.
This damage can result in reduced respiratory function and increased susceptibility to respiratory infections.
Types of Diabetes and Respiratory Function
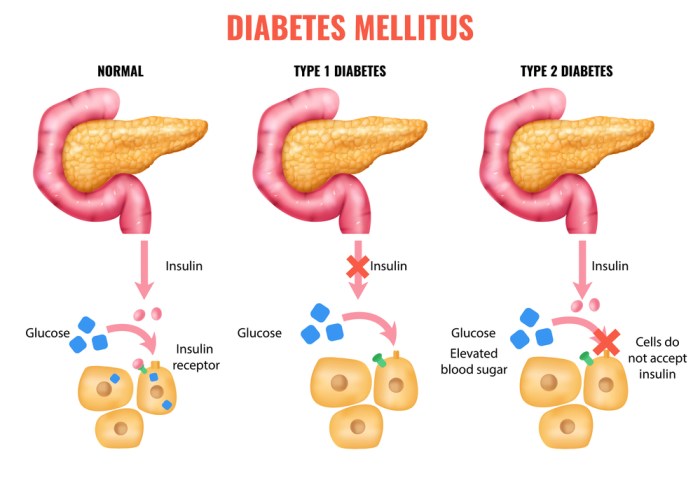
Type 1 diabetes, characterized by the body’s inability to produce insulin, can impact respiratory function through the same mechanisms as Type 2 diabetes. In Type 2 diabetes, the body either doesn’t produce enough insulin or the cells don’t respond effectively to it. Both types can result in elevated blood sugar levels, leading to the complications mentioned earlier.
Role of Complications
Several diabetes-related complications can directly contribute to shortness of breath. Diabetic nephropathy, kidney damage, can cause fluid retention, which can manifest as pulmonary edema and contribute to respiratory distress. Cardiovascular complications, such as heart failure, are frequently associated with diabetes and can lead to shortness of breath due to the heart’s reduced ability to pump blood efficiently. Additionally, diabetic ketoacidosis (DKA), a serious complication characterized by high blood acidity, can also result in shortness of breath, alongside other severe symptoms.
Potential Contributing Factors
Various underlying conditions can further exacerbate the connection between diabetes and shortness of breath. For instance, obesity, a frequent comorbidity of type 2 diabetes, can increase the strain on the respiratory system, making breathing more difficult. Chronic obstructive pulmonary disease (COPD) can interact with diabetes, increasing the risk of respiratory complications and exacerbating shortness of breath. Respiratory infections, such as pneumonia, can also be more prevalent and severe in individuals with diabetes, potentially leading to acute respiratory distress.
It’s important to note that the presence of these factors doesn’t automatically mean someone will experience shortness of breath, but it does increase the risk.
Symptoms and Presentation
Shortness of breath, or dyspnea, can be a significant concern for individuals with diabetes. Understanding the specific symptoms and how they might differ from those without diabetes is crucial for prompt diagnosis and effective management. Recognizing potential triggers can also help in preventing episodes. This section delves into the varied presentations of shortness of breath in diabetic patients, highlighting potential distinctions from those without the condition.
Experiencing shortness of breath alongside diabetes can be concerning. It could be a sign of something more serious, like a complication from diabetes. One potential culprit is an electrolyte imbalance, and understanding what happens when your body is low on electrolytes can help you piece together the puzzle. Low electrolytes can disrupt various bodily functions, potentially contributing to the shortness of breath you’re feeling.
It’s crucial to discuss these symptoms with your doctor to get a proper diagnosis and treatment plan for diabetes and shortness of breath.
Diverse Manifestations of Dyspnea in Diabetes
Shortness of breath in individuals with diabetes can stem from a multitude of underlying factors, ranging from cardiovascular complications to respiratory issues. Symptoms may vary in intensity and frequency, depending on the individual’s overall health, the specific type of diabetes, and the presence of co-morbidities. Important considerations include the presence of autonomic neuropathy, which can affect the body’s ability to regulate heart rate and breathing.
Comparison with Non-Diabetic Dyspnea
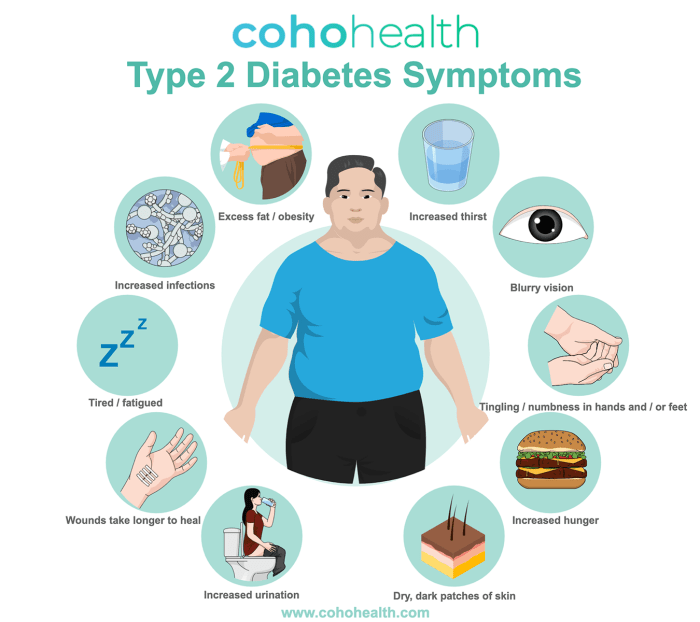
While shortness of breath can occur in anyone, the underlying causes and associated symptoms might differ between individuals with and without diabetes. For instance, a diabetic person experiencing shortness of breath might have concomitant symptoms like increased thirst, frequent urination, or blurred vision. These additional symptoms could be an indication of elevated blood glucose levels, highlighting the interconnectedness of diabetes and respiratory issues.
Conversely, a non-diabetic person might experience shortness of breath due to asthma or allergies, without the accompanying symptoms typically associated with high blood sugar.
Potential Triggers in Diabetic Patients
Several factors can trigger shortness of breath in diabetic individuals. These include:
- High blood glucose levels: Elevated blood sugar can lead to increased fluid retention and strain on the cardiovascular system, potentially causing shortness of breath.
- Diabetic ketoacidosis (DKA): This serious complication, characterized by the buildup of ketones in the blood, can manifest with severe shortness of breath, often accompanied by fruity-smelling breath and rapid pulse.
- Cardiovascular complications: Diabetes often increases the risk of heart disease, including conditions like heart failure, which can cause shortness of breath.
- Respiratory infections: Like anyone, diabetic patients are susceptible to respiratory infections, which can exacerbate shortness of breath.
- Autonomic neuropathy: Damage to the nerves controlling the heart and lungs can disrupt the body’s ability to regulate breathing, leading to dyspnea.
Symptom Severity Table
The following table provides a general overview of common symptoms and their potential severity. Note that severity can vary greatly based on individual factors and underlying conditions.
| Symptom | Description | Severity |
|---|---|---|
| Mild shortness of breath | A feeling of slight difficulty breathing, often noticeable only during exertion. | 1-2 |
| Moderate shortness of breath | Increased difficulty breathing, potentially interfering with daily activities. | 3-4 |
| Severe shortness of breath | Extreme difficulty breathing, requiring immediate medical attention. May include chest pain, rapid heart rate, and bluish discoloration of the skin. | 5-6 |
| Diabetic ketoacidosis (DKA) | Severe shortness of breath with fruity-smelling breath, rapid pulse, and other severe symptoms. | 6+ |
Diagnosis and Assessment
Shortness of breath in a diabetic patient can stem from a multitude of underlying causes, many of which are directly or indirectly related to diabetes complications. A thorough and systematic diagnostic approach is crucial to identify the specific cause and guide appropriate treatment. This involves a combination of patient history, physical examination, and various diagnostic tests.
Diagnostic Approach
A comprehensive evaluation for shortness of breath in a diabetic patient should begin with a detailed patient history, focusing on the onset, duration, and characteristics of the shortness of breath. Key factors to consider include the presence of any associated symptoms, such as chest pain, cough, fever, or leg swelling. The patient’s diabetic history, including the type of diabetes, duration of the disease, blood glucose control, and presence of any complications like neuropathy, nephropathy, or retinopathy, are also vital components.
The physical examination should include assessing vital signs, lung sounds, heart sounds, and peripheral edema.
Key Tests and Procedures
Several tests and procedures are essential to pinpoint the cause of shortness of breath in a diabetic patient. These include but are not limited to pulmonary function tests, electrocardiograms (ECGs), chest X-rays, and blood tests.
Experiencing shortness of breath alongside diabetes can be concerning. Often, this is linked to blood sugar fluctuations, and managing those fluctuations is key. A crucial part of that management can include smart snack choices. For instance, opting for healthy late night snacks that keep blood sugar levels stable can greatly impact your overall well-being, and help to prevent episodes of shortness of breath.
It’s always important to consult your doctor for personalized advice, especially when dealing with diabetes and breathing difficulties.
Pulmonary Function Tests
Pulmonary function tests (PFTs) assess the function of the lungs, measuring lung volumes, capacities, and airflow. These tests are useful in identifying restrictive or obstructive lung diseases, which can be common in diabetic patients. For instance, reduced lung volumes may suggest a restrictive lung disorder, whereas decreased airflow may point to an obstructive condition like asthma or chronic obstructive pulmonary disease (COPD).
Electrocardiograms (ECGs)
Electrocardiograms (ECGs) record the electrical activity of the heart. An ECG is valuable in ruling out cardiac causes of shortness of breath, such as arrhythmias or myocardial ischemia. In diabetic patients, ECGs can help detect underlying heart conditions that may be exacerbated by diabetes-related complications.
Chest X-rays
Chest X-rays provide a visual assessment of the lungs and heart. They can identify abnormalities such as pneumonia, pleural effusion, or pneumothorax. These findings can be important in determining the cause of shortness of breath.
Blood Tests
Blood tests are vital in evaluating various aspects of the patient’s health. These include complete blood counts (CBCs), blood glucose levels, and cardiac markers, such as troponin. CBCs can identify infections or other blood disorders. Elevated blood glucose levels can suggest uncontrolled diabetes, which may contribute to the shortness of breath. Cardiac markers can help determine if there is ongoing myocardial damage.
Comparison of Diagnostic Tools
| Diagnostic Tool | Description | Relevance to Diabetes |
|---|---|---|
| Pulmonary Function Tests (PFTs) | Measure lung function, including volumes, capacities, and airflow. | Helpful in identifying restrictive or obstructive lung diseases, common in diabetic patients due to complications. |
| Electrocardiograms (ECGs) | Record the electrical activity of the heart. | Useful in ruling out cardiac causes of shortness of breath, such as arrhythmias or myocardial ischemia, which can be exacerbated by diabetes. |
| Chest X-rays | Visual assessment of the lungs and heart. | Identify abnormalities like pneumonia, pleural effusion, or pneumothorax, potential contributors to shortness of breath. |
| Blood Tests (CBC, blood glucose, cardiac markers) | Assess various aspects of the patient’s health, including infections, blood glucose levels, and cardiac damage. | Detect infections, uncontrolled diabetes, or underlying cardiac problems that may be linked to the shortness of breath. |
Management and Treatment
Shortness of breath in diabetic patients requires a multifaceted approach encompassing both medical interventions and lifestyle adjustments. Effective management involves meticulous monitoring of blood glucose levels, addressing underlying cardiovascular complications, and implementing strategies to improve respiratory function. The goal is not just to alleviate symptoms but also to prevent exacerbations and improve overall well-being.Managing shortness of breath in diabetes necessitates a comprehensive strategy that considers the individual’s specific needs and health conditions.
Treatment plans should be tailored to address the root causes of the respiratory distress, whether it’s related to heart failure, infections, or other complications. Furthermore, patient education and active participation are crucial components of successful management.
Blood Glucose Control
Maintaining stable blood glucose levels is paramount in managing shortness of breath in diabetic patients. Fluctuations in blood sugar can impact various bodily functions, including respiratory mechanics. Hyperglycemia can lead to increased inflammation and impaired lung function, potentially worsening shortness of breath. Conversely, hypoglycemia can cause a cascade of symptoms, including dizziness, confusion, and even loss of consciousness, which can be detrimental to respiratory function.
Medication Management
Various medications can play a role in treating shortness of breath in diabetic patients, particularly if it’s linked to underlying conditions. For example, medications to manage heart failure, such as ACE inhibitors or beta-blockers, might be prescribed. Bronchodilators may be used to relax the airways and improve breathing, particularly if asthma or chronic obstructive pulmonary disease (COPD) is suspected.
It is essential to work closely with a healthcare team to determine the most appropriate medication regimen.
Lifestyle Modifications
Lifestyle changes can significantly impact the management of shortness of breath in diabetes. Weight management, regular exercise, and a balanced diet are key components. Weight loss can improve cardiac function, while regular exercise strengthens respiratory muscles and enhances overall cardiovascular health. Furthermore, avoiding smoking and excessive alcohol consumption is critical.
Monitoring and Follow-up
Regular monitoring of blood glucose levels, lung function tests, and cardiovascular assessments is essential. This allows healthcare providers to track the patient’s response to treatment and adjust the plan as needed. Regular follow-up appointments are vital to assess the effectiveness of interventions, detect any complications, and adapt the management strategy accordingly. This continuous monitoring ensures that treatment remains optimized and tailored to the patient’s evolving needs.
Experiencing shortness of breath alongside diabetes can be concerning. Understanding the optimal exercise regimen is key to managing both conditions effectively. For instance, consulting a healthcare professional about how many days a week should you exercise is important to avoid overexertion while also maintaining a healthy activity level. This balanced approach can help improve overall well-being and potentially alleviate shortness of breath symptoms in people with diabetes.
Treatment Comparisons
Different treatment approaches for shortness of breath in diabetes may vary in their effectiveness depending on the underlying cause and individual factors. For instance, a patient experiencing shortness of breath due to heart failure may respond better to a combination of medication and lifestyle modifications, whereas a patient with an infection may need antibiotic therapy as part of the treatment plan.
Healthcare professionals must consider these factors and tailor the approach to the specific circumstances.
Preventive Measures: Diabetes And Shortness Of Breath
Shortness of breath in individuals with diabetes can stem from various factors, often interconnected with blood sugar management. Proactive measures can significantly reduce the risk and severity of these breathing difficulties. Understanding the link between blood sugar control, lifestyle choices, and respiratory health is crucial for effective prevention.Effective management of diabetes, including meticulous blood sugar control, plays a pivotal role in mitigating the risk of respiratory complications.
Consistent monitoring and appropriate treatment strategies can significantly reduce the chances of developing shortness of breath. By focusing on lifestyle adjustments and adopting proactive measures, individuals with diabetes can take control of their respiratory health and overall well-being.
Blood Sugar Control Strategies
Maintaining stable blood glucose levels is paramount for preventing complications, including respiratory issues. Consistent monitoring and adherence to prescribed treatment plans are key elements in this strategy. This includes regular blood sugar checks, appropriate medication use, and a balanced diet. Diabetic patients should strive for blood sugar levels within the target range recommended by their healthcare providers.
Lifestyle Adjustments for Respiratory Health
Adopting a healthy lifestyle can significantly reduce the risk of shortness of breath in diabetic patients. This encompasses several crucial areas:
- Regular Exercise: Incorporating regular physical activity into the daily routine can improve lung capacity and overall cardiovascular health. Moderate-intensity exercise, such as brisk walking or swimming, for at least 30 minutes most days of the week is beneficial. Consistency is key. For instance, a 30-minute walk after dinner can significantly improve lung function and reduce the risk of shortness of breath.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains is essential for overall health and can help regulate blood sugar levels. Limiting processed foods, sugary drinks, and excessive saturated fats can further support optimal respiratory health. For example, a diet rich in antioxidants from fruits and vegetables can protect the respiratory system from oxidative stress.
- Quitting Smoking (if applicable): Smoking significantly impairs lung function and increases the risk of respiratory problems. Quitting smoking, if applicable, is crucial for maintaining good respiratory health. Support groups and cessation aids can help individuals successfully quit.
Actionable Steps for Diabetes Management
Implementing these steps can significantly contribute to the prevention of shortness of breath in diabetic patients:
- Regular Blood Sugar Monitoring: Tracking blood sugar levels throughout the day allows for early detection of fluctuations and timely adjustments to treatment plans. This proactive approach can help avoid potential complications, including shortness of breath.
- Adherence to Medication Regimen: Taking prescribed medications as directed is essential for maintaining optimal blood sugar control and minimizing the risk of complications. Missed doses or inconsistent medication schedules can negatively impact blood sugar levels and potentially lead to respiratory issues.
- Healthy Eating Habits: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is crucial for regulating blood sugar and supporting overall health, including respiratory function. Portion control is equally important.
- Stress Management Techniques: Chronic stress can negatively impact blood sugar levels and overall health. Implementing stress management techniques, such as meditation, yoga, or deep breathing exercises, can help regulate blood sugar and reduce the risk of shortness of breath.
Illustrative Cases
Understanding the interplay between diabetes and shortness of breath requires examining real-world examples. These case studies highlight the diverse presentations, diagnostic challenges, and treatment approaches associated with this complex condition. They also illustrate the importance of early detection and proactive management in achieving positive outcomes.Diabetes-related shortness of breath can manifest in various ways, impacting individuals differently. Recognizing the specific symptoms and underlying causes is crucial for effective diagnosis and treatment.
These cases demonstrate the potential for complications to arise and the proactive measures that can prevent future issues.
Case Study 1: Acute Respiratory Distress Syndrome (ARDS), Diabetes and shortness of breath
Diabetic ketoacidosis (DKA), a serious complication of diabetes, can lead to ARDS. This case highlights the potential for severe respiratory distress in uncontrolled diabetes.A 45-year-old male with poorly controlled type 2 diabetes presented with severe shortness of breath, rapid breathing, and chest pain. His blood glucose levels were significantly elevated, and he exhibited signs of DKA. A diagnosis of ARDS was made based on his clinical presentation and respiratory function tests.
Treatment focused on stabilizing his blood glucose levels, administering supportive respiratory care, and addressing any underlying infections. Recovery was gradual, requiring intensive care unit (ICU) monitoring and prolonged respiratory support. This case demonstrates the critical need for prompt diagnosis and aggressive treatment of DKA to prevent the development of severe complications like ARDS.
Case Study 2: Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
The presence of underlying COPD significantly influences the presentation and management of shortness of breath in diabetic patients.A 68-year-old female with a history of type 1 diabetes and COPD experienced a sudden worsening of shortness of breath, accompanied by increased sputum production and a persistent cough. Her diabetes was well-controlled, but the COPD exacerbation triggered an increase in respiratory symptoms.
The diagnosis was confirmed through pulmonary function tests and chest X-rays. Treatment involved administering bronchodilators, corticosteroids, and supplemental oxygen, alongside managing her diabetes. This case underscores the importance of recognizing the interplay between pre-existing conditions and diabetes in exacerbating respiratory symptoms. Early intervention and comprehensive management are crucial in preventing severe complications.
Case Study 3: Preventive Measures and Positive Outcomes
A proactive approach to managing diabetes can significantly reduce the risk of respiratory complications.A 30-year-old female with type 1 diabetes consistently maintained optimal blood glucose control through regular monitoring, healthy eating, and consistent exercise. She actively participated in diabetes education programs and diligently followed her prescribed medication regimen. Regular check-ups with her healthcare provider allowed for early detection and management of potential complications.
Over time, she avoided significant respiratory issues. This positive outcome highlights the importance of preventative measures, including stringent blood glucose control, healthy lifestyle choices, and consistent medical monitoring in reducing the risk of diabetes-related respiratory complications.
Underlying Conditions
Diabetes, a chronic metabolic disorder, can significantly impact overall health, making individuals susceptible to various other medical conditions. These coexisting conditions, often referred to as comorbidities, can exacerbate symptoms and complicate management. This section explores how certain underlying medical conditions can interact with diabetes, leading to shortness of breath.
Interplay Between Diabetes and Respiratory Diseases
Diabetes and respiratory diseases often share a complex relationship, with each condition potentially worsening the other. For example, diabetes can impair the body’s immune response, increasing the risk of respiratory infections. Furthermore, diabetic neuropathy, a common complication of diabetes, can affect the nerves controlling breathing, potentially leading to respiratory compromise. The interplay can create a vicious cycle, with diabetes increasing the susceptibility to respiratory issues and these issues, in turn, negatively impacting blood sugar control.
Comorbid Conditions Affecting Shortness of Breath in Diabetics
Several comorbidities can contribute to shortness of breath in individuals with diabetes. These conditions encompass a range of respiratory, cardiovascular, and other systems. The presence of these comorbidities necessitates careful assessment and management to address the multifaceted nature of the patient’s health needs.
Table Illustrating Possible Link Between Underlying Conditions and Shortness of Breath in Diabetes
| Underlying Condition | Description | Possible Link to Shortness of Breath |
|---|---|---|
| Chronic Obstructive Pulmonary Disease (COPD) | A group of lung diseases that block airflow to the lungs. | Diabetes can exacerbate COPD symptoms, potentially leading to increased shortness of breath, especially during periods of high blood sugar. Reduced lung function and inflammation can further compromise respiratory capacity. |
| Asthma | A chronic inflammatory disorder of the airways. | Diabetics with asthma may experience more frequent and severe asthma attacks, resulting in shortness of breath. Blood sugar fluctuations can trigger or worsen asthma symptoms. |
| Heart Failure | A condition in which the heart is unable to pump enough blood to meet the body’s needs. | Diabetes is a significant risk factor for heart failure. The combination can lead to fluid buildup in the lungs (pulmonary edema), causing shortness of breath, particularly during exertion. |
| Obesity | Excessive accumulation of body fat. | Obesity often accompanies diabetes and can contribute to shortness of breath. The extra weight puts stress on the respiratory system, reducing lung capacity and increasing the risk of sleep apnea, a sleep disorder that can cause breathing pauses. |
| Pneumonia | An infection of the lungs. | Individuals with diabetes are more susceptible to pneumonia due to weakened immune function. Pneumonia can cause inflammation and fluid buildup in the lungs, resulting in shortness of breath. |
| Sleep Apnea | A sleep disorder characterized by pauses in breathing during sleep. | Diabetes is a risk factor for sleep apnea. The combination can lead to chronic hypoxia (low blood oxygen levels) and further complications. This lack of oxygen can cause shortness of breath during sleep and daytime drowsiness. |
Visual Representation
Understanding the intricate relationship between diabetes and shortness of breath requires a clear visualization of the anatomical structures involved. The respiratory system, a complex network of organs, is crucial for oxygen intake and carbon dioxide expulsion. Diabetes, when uncontrolled, can disrupt this delicate balance, leading to various complications, including respiratory issues.
Anatomical Structures Involved in Shortness of Breath
The respiratory system comprises the nose, pharynx, larynx, trachea, bronchi, and lungs. Air enters through the nose and mouth, passing through the pharynx and larynx before reaching the trachea. The trachea branches into two bronchi, each leading to a lung. Within the lungs, the bronchi further divide into smaller bronchioles, ultimately ending in tiny air sacs called alveoli. These alveoli are the primary sites of gas exchange.
The diaphragm and intercostal muscles are crucial for breathing mechanics. Dysfunction in any of these components can contribute to shortness of breath.
Visual Representation of the Respiratory System
Imagine a tree. The trunk represents the trachea, branching into two major bronchi, which are the thick branches. These further subdivide into smaller and smaller bronchioles, resembling twigs and leaves. The alveoli are like the tiny leaves at the end of the branches. The interplay of these components allows for efficient gas exchange.
In a person with diabetes, potential complications, such as fluid buildup in the lungs, could be represented by a blockage in the bronchioles, making it difficult for the air to reach the alveoli. This visual analogy helps illustrate the potential impact of diabetes on the respiratory system.
Effects of Diabetes on Lung Tissue
High blood sugar levels can damage various tissues throughout the body, including the lungs. This damage can manifest in several ways. For instance, thickening of the alveolar walls can hinder gas exchange, reducing the efficiency of oxygen uptake and carbon dioxide release. Additionally, chronic inflammation in the lungs can lead to a build-up of fluid, making it difficult to expand the lungs and breathe.
Diabetic ketoacidosis (DKA), a serious complication of uncontrolled diabetes, can also affect the lungs, potentially leading to respiratory failure.
High Blood Sugar and Lung Tissue: A Visual Explanation
Imagine a healthy alveolus as a balloon filled with air, allowing for smooth gas exchange. In a diabetic patient with uncontrolled blood sugar, the alveolus might become inflamed and thickened, similar to a balloon with a rough surface. This thickened membrane impedes the diffusion of oxygen and carbon dioxide, leading to a reduced ability to breathe easily. In severe cases, the buildup of fluid in the lungs could be visualized as the balloon being partially filled with water, further hindering proper functioning.
This visual representation highlights the potential impact of high blood sugar on the structure and function of the alveoli.
Summary
In conclusion, the connection between diabetes and shortness of breath is multifaceted and complex. Proper understanding of the underlying mechanisms, varied symptoms, diagnostic approaches, and comprehensive management strategies are essential for optimal patient care. Ultimately, proactive management, including lifestyle adjustments and regular monitoring, can significantly reduce the risk of this complication. Early intervention and personalized care plans are key to effectively addressing this issue.




