Decorticate vs decerebrate posturing sets the stage for this enthralling narrative, offering readers a glimpse into the complexities of neurological conditions. This comprehensive exploration delves into the defining characteristics, causes, clinical manifestations, treatment strategies, and potential outcomes of these distinct posturing types. Understanding the nuances between decorticate and decerebrate posturing is crucial for healthcare professionals and anyone interested in the intricacies of the human nervous system.
We’ll dissect the anatomical locations of brain damage, examining the potential relationship between causes and affected areas. Clinical manifestations and assessment methods will be detailed, providing a clearer picture of how these conditions present themselves. The discussion will cover treatment approaches and the critical role of supportive care in managing these conditions, ultimately concluding with an analysis of prognosis and potential outcomes.
Defining Posturing Types
Understanding decorticate and decerebrate posturing is crucial for neurological assessments. These abnormal postures, often observed in patients with brain damage, provide valuable insights into the location and severity of the injury. They reflect the interruption of normal brain pathways controlling muscle tone and movement. The specific pattern of posturing can help clinicians distinguish between different levels of brain stem dysfunction.
Decorticate Posturing Definition
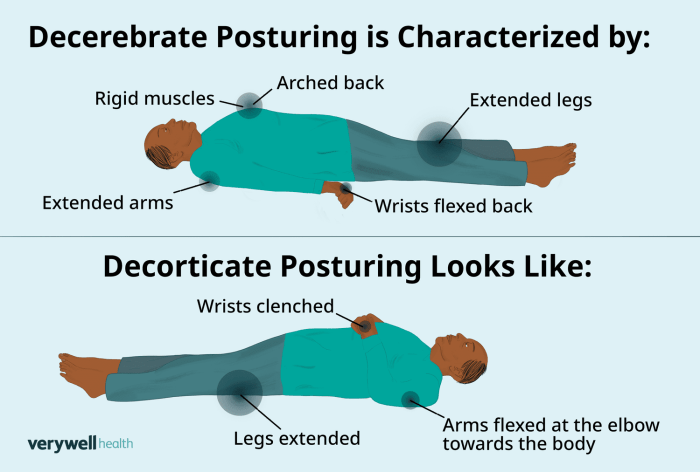
Decorticate posturing is characterized by the flexion of the upper extremities, with the arms drawn inward towards the chest, and the wrists and fingers flexed. The lower extremities are typically extended and externally rotated. This posture suggests damage to the cerebral cortex or its associated pathways, disrupting the normal inhibitory influence on muscle tone. The patient’s posture reflects a loss of cortical control.
Decerebrate Posturing Definition
Decerebrate posturing involves the extension of the upper extremities, with the arms straight out and the hands pronated (palms down). The lower extremities are also extended. The posture is often associated with more severe brain stem damage. The posture results from the loss of the inhibitory influence on muscle tone from the brain stem.
Comparison of Decorticate and Decerebrate Posturing
Decorticate and decerebrate posturing, though both indicative of neurological dysfunction, differ significantly in their anatomical origins and the implications for the affected areas. Decorticate posturing usually suggests a lesion in the cerebral cortex, whereas decerebrate posturing points to a more severe lesion in the brainstem. The differing extents of muscle tone disruption reflect the level of brain damage.
Anatomical Locations of Brain Damage
The anatomical locations of brain damage responsible for these posturing types are significant. Decorticate posturing arises from damage to the cerebral cortex, particularly the corticospinal tracts, disrupting the normal inhibition of muscle tone. Decerebrate posturing, on the other hand, is associated with damage in the brainstem, affecting the descending pathways controlling muscle tone. The location of the lesion significantly impacts the resulting posturing patterns.
Contrasting Decorticate and Decerebrate Posturing, Decorticate vs decerebrate posturing
| Feature | Decorticate Posturing | Decerebrate Posturing |
|---|---|---|
| Symptoms | Flexion of upper extremities (arms drawn inward), flexion of wrists and fingers, extension and external rotation of lower extremities. | Extension of upper extremities (arms straight out, hands pronated), extension of lower extremities. |
| Brain Areas Affected | Cerebral cortex, corticospinal tracts. | Brainstem, descending pathways. |
| Severity | Generally less severe than decerebrate posturing. | Generally more severe than decorticate posturing. |
| Examples | Stroke affecting the cerebral cortex, tumors in the cerebral hemisphere. | Severe head injuries, brainstem stroke, or infections. |
Causes and Etiologies
Understanding the causes of decorticate and decerebrate posturing is crucial for timely diagnosis and appropriate intervention. These abnormal postures, indicative of brain stem or cerebral dysfunction, signal a critical neurological event. Pinpointing the root cause allows healthcare professionals to tailor treatment strategies to the underlying condition.
Common Causes of Decorticate Posturing
Decorticate posturing, characterized by the inward flexion of the arms and legs, typically points towards damage or dysfunction in the cerebral cortex or upper brain centers. Several factors can contribute to this.
- Stroke: Ischemic or hemorrhagic strokes affecting the cerebral cortex or its associated pathways are frequent causes of decorticate posturing. The damage disrupts normal motor control signals, leading to the characteristic flexion posture. Patients experiencing stroke often present with other neurological deficits, including language impairment, sensory loss, and hemiparesis (weakness on one side of the body).
- Traumatic Brain Injury (TBI): Severe head trauma, such as from falls or motor vehicle accidents, can disrupt the neural pathways controlling movement, resulting in decorticate posturing. The severity of the injury and the specific area affected influence the presentation of the posture. Associated symptoms may include loss of consciousness, amnesia, and cognitive impairment.
- Brain Tumors: Growing tumors within the brain can exert pressure on surrounding structures and disrupt neural pathways. The pressure can cause decorticate posturing, alongside other neurological symptoms depending on the tumor’s location and growth rate. Symptoms can vary from mild to severe, and may include headaches, seizures, and cognitive changes.
- Infections: Infections like encephalitis or meningitis can cause inflammation and swelling in the brain. This swelling can compress neural pathways, leading to the development of decorticate posturing. The infection’s severity and location within the brain influence the severity and presentation of the posture.
Common Causes of Decerebrate Posturing
Decerebrate posturing, marked by the extension of the arms and legs, typically indicates damage or dysfunction at a more profound level, often involving the brainstem.
- Severe Head Trauma: Severe head trauma, a common cause of decorticate posturing, can also result in decerebrate posturing, particularly if the damage extends to the brainstem. The severity and location of the injury significantly affect the presentation of the posture. Associated symptoms may include severe loss of consciousness, dilated pupils, and abnormal breathing patterns.
- Brainstem Lesions: Direct damage to the brainstem due to strokes, tumors, or infections can lead to decerebrate posturing. The brainstem controls vital functions like breathing and heart rate, and damage to this region can be life-threatening. Associated symptoms include loss of reflexes, difficulty breathing, and changes in heart rate.
- Cerebral Hemorrhage: Bleeding within the brain, often stemming from aneurysms or arteriovenous malformations (AVMs), can disrupt the brainstem’s function and lead to decerebrate posturing. The location and volume of the hemorrhage affect the severity and nature of the posture and other neurological symptoms.
- Metabolic Disorders: Conditions like severe hypoglycemia (low blood sugar) or hepatic encephalopathy (liver dysfunction) can disrupt brain function and potentially result in decerebrate posturing. These metabolic issues often present with other neurological symptoms, including confusion, altered level of consciousness, and seizures.
Relationship Between Causes and Affected Anatomical Areas
The specific anatomical areas affected by the underlying cause directly influence the type of posturing. For example, lesions affecting the upper brain centers (cerebral cortex) tend to cause decorticate posturing, while those affecting the brainstem often result in decerebrate posturing. This difference reflects the varying levels of neural control impacted by the etiological factors.
| Posturing Type | Potential Causes | Age Ranges | Associated Symptoms |
|---|---|---|---|
| Decorticate | Stroke, TBI, Brain Tumors, Infections | All ages | Hemiparesis, sensory loss, cognitive impairment, headaches, seizures |
| Decerebrate | Severe TBI, Brainstem Lesions, Cerebral Hemorrhage, Metabolic Disorders | All ages | Loss of consciousness, dilated pupils, abnormal breathing, changes in heart rate, confusion |
Clinical Manifestations and Assessment
Understanding the specific clinical manifestations of decorticate and decerebrate posturing is crucial for accurate neurological assessment and timely intervention. These abnormal postures, often indicative of severe brain injury, provide valuable clues about the location and severity of the underlying pathology. Recognizing the subtle yet significant differences in these postures is paramount for guiding treatment strategies.
Decorticate Posturing Clinical Manifestations
Decorticate posturing, characterized by flexion of the upper extremities and extension of the lower extremities, reflects damage to the cerebral cortex. This posture often presents with the arms flexed inward, wrists and fingers bent, and the legs extended straight. The hands may be clenched into fists. This pattern suggests a lesion above the brainstem, typically in the cerebral hemispheres.
Key clinical manifestations include:
- Flexion of the upper extremities (arms bent inward, wrists and fingers flexed).
- Extension of the lower extremities (legs extended straight).
- Adduction of the upper extremities (arms drawn towards the midline of the body).
- Pronation of the forearms (palms facing downward).
- Possible clenched fists.
Decerebrate Posturing Clinical Manifestations
Decerebrate posturing signifies more severe brain stem damage, often associated with a worse prognosis. This posture is characterized by the extension of the upper and lower extremities, a rigid posture with the arms and legs extended straight out, and the head often extended backward. It’s important to note that this posture is often a more alarming sign than decorticate posturing due to its implications for brainstem function.
Key clinical manifestations include:
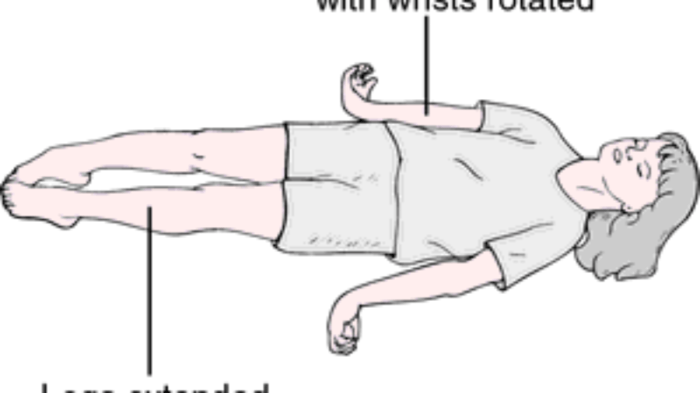
- Extension of the upper extremities (arms straight out, often rotated outward).
- Extension of the lower extremities (legs extended straight).
- Pronation of the forearms (palms facing downward).
- Extension of the head (head arched or tilted backward).
Neurological Assessment Methods
Differentiating between decorticate and decerebrate posturing requires a comprehensive neurological assessment. Careful observation of the patient’s posture and muscle tone is essential. The examiner should note the degree of flexion or extension, the symmetry or asymmetry of the posture, and any associated muscle rigidity. In addition to visual observation, the examiner should also assess for other neurological deficits, such as impaired reflexes, cranial nerve dysfunction, and changes in level of consciousness.
Assessment Findings Table
| Posturing Type | Muscle Groups Affected | Posture Description | Associated Neurological Levels |
|---|---|---|---|
| Decorticate | Upper extremities, lower extremities | Upper extremities flexed, lower extremities extended | Damage above brainstem, typically in cerebral hemispheres |
| Decerebrate | Upper extremities, lower extremities, head | Upper and lower extremities extended, head extended; rigid posture | Severe damage to brainstem |
Treatment and Management Strategies
Treating patients exhibiting decorticate or decerebrate posturing necessitates a multifaceted approach. The primary focus is on identifying and addressing the underlying cause, as these posturing types are often symptoms of a more serious neurological condition. Effective treatment strategies involve a combination of medical interventions, supportive care, and rehabilitation to maximize functional recovery and improve the patient’s quality of life.Effective management hinges on a thorough understanding of the specific cause.
While there’s no direct treatment for the posturing itself, managing the underlying condition can lead to improvement. This often involves addressing the neurological injury or disease, managing complications, and implementing supportive care measures.
Common Treatment Approaches for Decorticate Posturing
Identifying and treating the underlying cause is paramount. This could involve medications to control seizures, managing infections, or addressing metabolic imbalances. Physical therapy plays a critical role in improving muscle strength and range of motion, preventing contractures, and promoting functional independence. Occupational therapy helps adapt the environment and daily activities to support the patient’s abilities. Speech therapy may be necessary to address communication issues.
Ever wondered about decorticate vs decerebrate posturing? It’s fascinating how the brain’s damage can manifest physically. For a deeper dive into the impact of weight loss on heart health, check out this expert advice on ask an expert will losing weight lower my heart disease risk. Interestingly, these neurological postures, while not directly linked to weight loss, highlight the intricate connection between the brain and body.
Understanding these neurological responses provides a better appreciation of the body’s complex systems.
Common Treatment Approaches for Decerebrate Posturing
Similar to decorticate posturing, treating decerebrate posturing involves addressing the underlying cause, which may be a severe brain injury, stroke, or other neurological conditions. Medical interventions may include medications to control seizures, manage infections, or stabilize vital signs. Maintaining a stable physiological environment is crucial. Physical and occupational therapies are vital in maintaining and improving range of motion, preventing complications, and facilitating functional independence.
Caregivers may require training to assist with activities of daily living and support the patient’s needs.
Importance of Supportive Care
Supportive care is integral in managing both decorticate and decerebrate posturing. It encompasses a wide range of interventions aimed at minimizing discomfort, promoting comfort, and preventing complications. This includes pain management, nutritional support, respiratory assistance, and meticulous skin care to prevent pressure sores. Emotional support for both the patient and their family is essential.
Interventions and Therapies for Managing Posturing Types
| Posturing Type | Intervention/Therapy | Examples | Anticipated Outcomes | Timeline |
|---|---|---|---|---|
| Decorticate | Medical Management | Anticonvulsants, antibiotics, antipyretics | Control of seizures, infections, fever | Variable, dependent on underlying cause |
| Physical Therapy | Range of motion exercises, strengthening exercises, positioning | Improved muscle strength, ROM, decreased contractures | Weeks to months | |
| Occupational Therapy | Adaptive equipment, environmental modifications, ADL training | Improved functional independence, safety | Weeks to months | |
| Speech Therapy | Communication strategies, augmentative communication | Improved communication | Variable, dependent on severity of impairment | |
| Nutritional Support | Feeding tubes, dietary modifications | Maintenance of adequate nutrition | Ongoing | |
| Pain Management | Analgesics, PCA pumps | Reduction of pain and discomfort | Ongoing | |
| Decerebrate | Medical Management | Anticonvulsants, antibiotics, vital sign monitoring | Control of seizures, infections, stabilization of vital functions | Variable, dependent on underlying cause |
| Physical Therapy | Passive ROM, positioning, muscle re-education | Maintenance of ROM, prevention of contractures, and muscle atrophy | Weeks to months | |
| Occupational Therapy | Adaptive equipment, environmental modifications, positioning | Improved functional independence and safety | Weeks to months | |
| Respiratory Support | Mechanical ventilation, suctioning | Maintenance of adequate breathing | Ongoing | |
| Nutritional Support | Feeding tubes, nutritional supplements | Maintenance of adequate nutrition | Ongoing | |
| Pain Management | Analgesics, PCA pumps | Reduction of pain and discomfort | Ongoing |
Prognosis and Outcomes
Understanding the potential outcomes for patients experiencing decorticate or decerebrate posturing is crucial for both the patient and their care team. Accurate prognosis depends heavily on identifying the underlying cause and the patient’s overall health status prior to the onset of the neurological insult. This section delves into the variability of recovery and factors influencing prognosis, offering a framework for realistic expectations.
Potential Outcomes for Decorticate Posturing
Decorticate posturing, characterized by the flexion of the upper extremities and extension of the lower extremities, often reflects a lesion in the cerebral hemispheres or upper brainstem. The prognosis for recovery from decorticate posturing varies widely, dependent on the severity and location of the underlying brain injury. Some patients with mild cases might experience significant improvement and regain function, while others may have limited recovery.
Ever wondered about decorticate vs decerebrate posturing? It’s fascinating how neurological conditions manifest physically. While these postures highlight neurological damage, it’s important to remember that underlying health conditions, such as thyroid issues, can impact the heart, as discussed in depth at thyroid disease and the heart. Ultimately, understanding these neurological responses helps medical professionals diagnose and treat patients effectively.
Learning about different posturing types can be a real eye-opener.
Factors influencing the extent of recovery include the extent of brain damage, the speed of diagnosis and treatment of the underlying cause, and the patient’s pre-existing health conditions.
Potential Outcomes for Decerebrate Posturing
Decerebrate posturing, characterized by the extension of all four extremities, signifies a more severe lesion typically located in the brainstem. The prognosis for recovery from decerebrate posturing is generally poorer than for decorticate posturing, as brainstem damage is often more devastating. Full recovery is uncommon, and even with rehabilitation, patients may experience residual motor impairments. The degree of recovery hinges on the extent of brainstem damage and the swiftness of intervention for the causative issue.
Understanding decorticate and decerebrate posturing is crucial in neurological assessments. These posturing types often show up in severe cases, and a crucial part of rehabilitation after injury is physical therapy. For instance, following a Jones fracture, a specific type of foot injury, rigorous physical therapy, like the kind detailed at physical therapy after a jones fracture , helps restore function and prevent these types of posturing from becoming a long-term issue.
Ultimately, these posturing distinctions help medical professionals pinpoint the location and severity of the neurological damage.
Factors Influencing Prognosis and Recovery
Several factors play a critical role in the prognosis and recovery of patients with these posturing types. The severity and location of the underlying neurological injury are paramount. A more diffuse injury typically results in poorer outcomes. The speed of diagnosis and treatment for the underlying cause directly influences the extent of brain damage and the potential for recovery.
Pre-existing medical conditions and the patient’s age also play a role. A younger patient with no significant prior health issues generally has a better chance of recovery. The patient’s motivation and engagement in rehabilitation also contribute significantly to positive outcomes.
Prognosis Summary Table
| Prognosis Factor | Recovery Timeline (Estimate) | Potential Complications |
|---|---|---|
| Severity of Brain Injury | Mild: weeks to months; Moderate: months to years; Severe: limited or no recovery | Spasticity, contractures, seizures, pressure sores, swallowing difficulties, respiratory issues |
| Location of Brain Injury | Cortical lesions: potentially better outcomes than brainstem lesions. | Depend on the location and extent of the damage |
| Speed of Diagnosis & Treatment | Early intervention can improve the likelihood of recovery. | Delay in diagnosis can worsen outcomes |
| Pre-existing Medical Conditions | Presence of other conditions can impact recovery | Underlying health conditions can influence the extent of recovery |
| Patient Age | Younger patients tend to have a better chance of recovery | Age is associated with varying physiological responses and vulnerability |
| Patient Motivation & Rehabilitation Participation | Active participation is crucial | Lack of motivation can hinder progress |
Illustrative Examples
Decorticate and decerebrate posturing are crucial indicators of neurological damage, offering valuable insights into the location and severity of the brain injury. Understanding these posturing types, alongside the factors influencing their presentation, is vital for effective diagnosis and treatment. Case studies, combined with an analysis of the role of imaging techniques, help solidify this understanding.
Case Study: Decorticate Posturing
A 65-year-old male patient presented with a sudden onset of severe headache and altered mental status. Neurological examination revealed decorticate posturing, characterized by the flexion of the upper extremities (arms bent at the elbows, wrists flexed, and fingers fisted), with extension of the lower extremities (legs extended). The patient’s pupils were constricted and sluggishly reactive to light. Further assessment revealed a history of hypertension and a recent stroke.
Computed Tomography (CT) scans confirmed a large right-hemispheric stroke, implicating the corticospinal tracts as a primary site of injury. The patient’s condition deteriorated rapidly, and despite aggressive medical interventions, the prognosis was poor due to the extensive brain damage.
Case Study: Decerebrate Posturing
A 28-year-old female patient, involved in a high-speed motor vehicle accident, sustained severe head trauma. Upon arrival at the emergency room, the patient displayed decerebrate posturing. This was manifested by the rigid extension of all extremities, with the arms extended straight out, palms pronated (turned inward), and the legs also extended. The patient’s pupils were dilated and non-reactive to light.
Initial CT scans revealed a significant diffuse axonal injury, impacting the brainstem and disrupting descending motor pathways. While the patient initially responded to some treatments, the profound brainstem damage resulted in a poor outcome.
Factors Affecting Severity and Prognosis
The severity and prognosis of both decorticate and decerebrate posturing are influenced by several key factors. These include:
- Location and Extent of Brain Injury: The precise area of the brain affected dictates the specific pattern of posturing. Larger or more widespread lesions typically correlate with more severe and debilitating outcomes. For example, a stroke involving a significant portion of the frontal lobe can result in more profound decorticate posturing compared to a smaller lesion. Similarly, a diffuse axonal injury in the brainstem region is likely to manifest with more severe and persistent decerebrate posturing.
- Underlying Medical Conditions: Pre-existing conditions like hypertension, diabetes, or heart disease can significantly impact the patient’s overall health and response to treatment, potentially exacerbating the severity of posturing and reducing the chances of a favorable outcome. Patients with pre-existing conditions might require more intensive care and have a more challenging recovery trajectory.
- Time to Treatment: The time elapsed between the onset of the injury and receiving appropriate medical care is crucial. Early intervention is essential for maximizing recovery potential and minimizing long-term complications. Delays in diagnosis or treatment can lead to more severe neurological deficits.
Role of Imaging Techniques
Imaging techniques play a critical role in visualizing the brain damage associated with each posturing type.
- Computed Tomography (CT) Scans: CT scans are valuable for identifying structural abnormalities in the brain, such as hemorrhages, contusions, or edema. They provide a quick and readily available method for initial assessment, helping to determine the location and extent of the brain injury, providing crucial data for initial diagnosis and treatment.
- Magnetic Resonance Imaging (MRI) Scans: MRI scans offer higher resolution and can provide more detailed information about the soft tissues of the brain. They can reveal subtle structural damage not visible on CT scans, and can detect more subtle abnormalities, including diffuse axonal injury. This is particularly crucial for evaluating the extent of the damage in cases of decerebrate posturing.
Final Wrap-Up: Decorticate Vs Decerebrate Posturing
In conclusion, understanding decorticate and decerebrate posturing provides a crucial framework for comprehending neurological damage. The interplay between anatomy, clinical presentation, and treatment strategies is highlighted, showcasing the multifaceted nature of these conditions. While the potential for recovery varies, a thorough understanding of these factors is paramount for effective patient management and care.




