When does fertility return after stopping birth control? This crucial question affects many women, and the answer isn’t always straightforward. Factors like age, individual hormonal variations, and even pre-existing conditions can all play a role in how quickly your body returns to its natural fertility cycle after discontinuing birth control. Understanding the nuances of different birth control methods, and how they affect your body, is key to navigating this process.
This guide delves into the complexities of fertility return, providing a comprehensive overview of the factors involved, potential complications, and strategies to optimize your chances of getting pregnant.
This comprehensive guide will explore the diverse factors that influence fertility return, ranging from the different types of birth control methods and their respective impacts to practical methods for tracking fertility and potential complications. We’ll also delve into strategies for optimizing the process, and provide insights into ovulation and the menstrual cycle. By understanding these elements, you can make informed decisions and navigate this important life stage.
Factors Affecting Fertility Return
Returning to fertility after stopping birth control is a journey influenced by various factors. While the desire to conceive is often immediate, the body needs time to adjust and resume its natural reproductive cycle. Understanding these influencing factors can help individuals anticipate the timeframe and approach this transition with realistic expectations.The process of fertility return is highly individualized, influenced by a complex interplay of physiological factors.
This complexity underscores the importance of open communication with healthcare providers to understand personal circumstances and potential challenges.
Individual Hormonal Variations
Hormonal fluctuations are a significant factor in the fertility return process. Birth control methods often alter the body’s natural hormonal balance, and the time it takes for hormones to re-establish their equilibrium varies. This variability is influenced by factors such as the type of birth control used, the duration of use, and individual metabolic rates. Some individuals may experience a more rapid return to normal hormonal levels, while others may take longer.
For instance, women who used hormonal birth control for several years might experience a slightly slower return to regular ovulation compared to those who used it for a shorter period.
Impact of Age
Age is a crucial factor influencing fertility return. Ovarian reserve, the pool of eggs available for fertilization, naturally declines with age. While the cessation of birth control can potentially restore some of the reproductive function, the ability of the ovaries to produce viable eggs is not completely unaffected by age. For example, a woman in her late 30s or early 40s might experience a slightly slower recovery time compared to a younger woman.
This is due to the natural aging process impacting the quantity and quality of eggs. The effects of age are more pronounced as women approach menopause, when the likelihood of successful conception significantly decreases.
Potential Pre-Existing Conditions
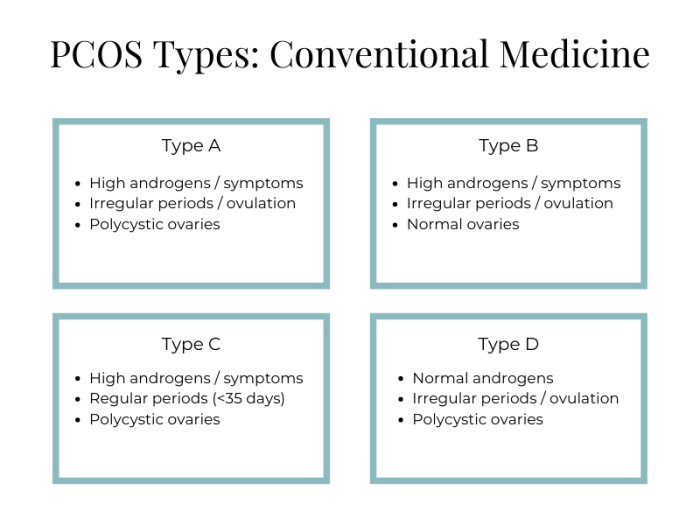
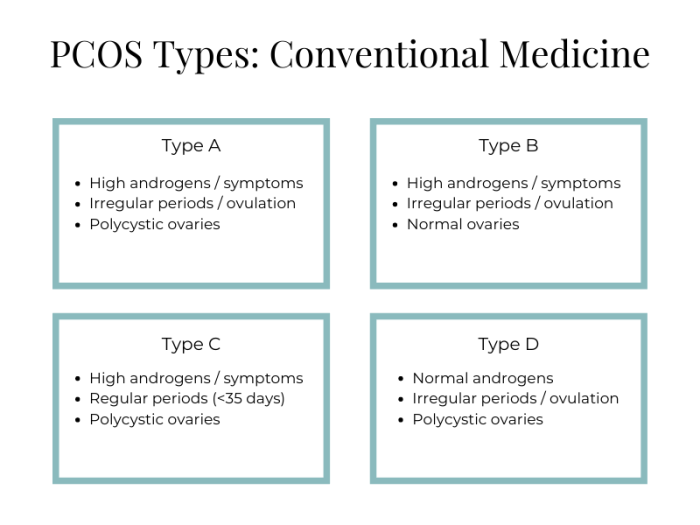
Underlying health conditions can impact the return to fertility after discontinuing birth control. Conditions like Polycystic Ovary Syndrome (PCOS), endometriosis, or thyroid disorders can affect ovulation and hormone production, potentially extending the time it takes for fertility to return. For example, women with PCOS may experience irregular menstrual cycles, which can complicate the prediction of ovulation and successful conception.
Addressing any pre-existing conditions before attempting to conceive can optimize the chances of a successful pregnancy.
Table of Factors Affecting Fertility Return
| Factor | Description | Impact on Return Time |
|---|---|---|
| Individual Hormonal Variations | Differences in how quickly the body re-establishes normal hormone levels after birth control cessation. | Can vary significantly, ranging from rapid to extended periods. |
| Age | The natural decline in ovarian reserve with increasing age. | Generally, older women may experience slower fertility return. |
| Pre-existing Conditions | Underlying health conditions like PCOS, endometriosis, or thyroid disorders. | Can potentially prolong the time it takes to conceive. |
Types of Birth Control and Their Impact
Understanding how various birth control methods affect fertility return is crucial for individuals planning pregnancies. Different methods employ diverse mechanisms, leading to varying recovery times after discontinuation. This section delves into the specific impacts of hormonal and non-hormonal birth control on the body’s reproductive system.Different birth control methods employ diverse mechanisms, impacting the body’s reproductive system in unique ways.
These methods range from those that primarily suppress ovulation to those that alter the cervical mucus or the uterine environment. Understanding these mechanisms provides insight into the potential timeframes for fertility to return after discontinuing a particular method.
Wondering when your fertility returns after ditching the birth control pill? It’s a common question, and the answer varies. Factors like the type of birth control you used and your individual body play a role. To fuel your body during this transition, consider carefully how to choose a protein bar, like this one , ensuring it aligns with your health goals.
Ultimately, your fertility will likely return relatively quickly for most people, but it’s always best to discuss any concerns with your doctor.
Hormonal Birth Control Methods
Hormonal birth control methods, including combined oral contraceptives, progestin-only pills, and hormonal IUDs, work by suppressing ovulation and altering the uterine lining. This suppression can temporarily impact the natural cycle, potentially affecting the time it takes for ovulation to resume after discontinuation. The duration of this impact varies depending on the specific method and individual factors.
- Combined Oral Contraceptives (COCs): These pills contain both estrogen and progestin. Discontinuing COCs often results in a swift return to fertility, typically within a few months. Individual experiences may vary. For example, a woman who used COCs for a year may experience a faster return to ovulation compared to someone who used them for five years. However, the time frame for restoring fertility varies based on factors like individual metabolic rate and overall health.
- Progestin-only pills: These pills suppress ovulation and alter cervical mucus. Fertility usually returns relatively quickly after stopping these pills, typically within a few months. Similar to COCs, individual experiences can differ.
- Hormonal IUDs: These devices release progestin to prevent pregnancy. The time it takes for fertility to return after removing a hormonal IUD can vary, but it generally takes a few months. The specific duration is affected by factors like the individual’s body’s hormonal response and the length of time the device was used.
Non-Hormonal Birth Control Methods
Non-hormonal methods, such as barrier methods (condoms, diaphragms, cervical caps), the withdrawal method, and fertility awareness-based methods, don’t directly suppress ovarian function or ovulation. Therefore, fertility typically returns promptly after discontinuation.
- Barrier methods: These methods physically prevent sperm from reaching the egg. Once discontinued, fertility typically returns immediately, as these methods do not interfere with the natural hormonal cycle.
- Withdrawal method: This method involves withdrawing the penis from the vagina before ejaculation. Fertility returns quickly after discontinuing this method.
- Fertility awareness-based methods: These methods involve tracking ovulation cycles. These methods do not affect ovarian function or ovulation directly, allowing fertility to return quickly.
Comparison of Fertility Return Timeframes
The following table summarizes the typical timeframe for fertility return after discontinuing various birth control methods. It’s crucial to remember that these are estimates, and individual experiences may vary.
| Birth Control Method | Typical Fertility Return Timeframe |
|---|---|
| Combined Oral Contraceptives | Typically within a few months |
| Progestin-only pills | Typically within a few months |
| Hormonal IUDs | Typically within a few months |
| Barrier methods | Immediately |
| Withdrawal method | Immediately |
| Fertility awareness-based methods | Immediately |
Methods for Tracking Fertility Return
Navigating the return to fertility after discontinuing birth control can feel like a journey into the unknown. Understanding how your body responds and the various ways to monitor this process can significantly aid in planning a pregnancy. This section will explore the most common methods for tracking fertility return, detailing their benefits, limitations, and how to interpret the results.
Basal Body Temperature (BBT) Monitoring
Tracking basal body temperature (BBT) involves recording your body temperature first thing in the morning before any activity. This method is based on the slight temperature shift that occurs around ovulation. A rise in temperature usually signifies ovulation. Consistent monitoring can help identify patterns and predict ovulation.
- Benefits: BBT is a relatively inexpensive and non-invasive method. It can provide insights into the menstrual cycle and ovulation patterns. It is helpful for identifying irregular cycles or potential underlying issues.
- Limitations: BBT can be affected by factors like illness, stress, and even changes in sleep patterns. Results may not be immediately conclusive and consistent monitoring is required for reliable predictions.
- Interpretation: A consistent temperature rise for several days, usually lasting for 2-3 days, signifies ovulation. A steady temperature throughout the cycle may indicate issues that warrant consultation with a healthcare provider.
Cervical Mucus Changes
Monitoring cervical mucus changes involves observing the texture, consistency, and amount of cervical mucus throughout the cycle. This method is based on the noticeable changes in cervical mucus that occur around ovulation.
- Benefits: Cervical mucus observation is a non-invasive method that can be easily incorporated into daily routines. It offers a natural way to track fertility patterns.
- Limitations: Interpretation can be subjective, and requires practice to identify the key characteristics of fertile mucus. Changes in mucus can be affected by factors like hydration and stress.
- Interpretation: Fertile mucus is typically clear, stretchy, and slippery, resembling egg whites. Dry or thick mucus generally signifies the non-fertile phase of the cycle.
Ovulation Predictor Kits (OPKs)
Ovulation predictor kits (OPKs) are urine-based tests that detect the surge in luteinizing hormone (LH) in the urine, a hormone that precedes ovulation.
- Benefits: OPKs provide a more objective measure of ovulation. They are readily available and easy to use. They offer a relatively quick way to identify the fertile window.
- Limitations: OPKs can be influenced by hydration levels and other factors affecting urine composition. False positives or negatives are possible.
- Interpretation: Positive test results indicate an impending surge in LH, signaling the fertile period. Following the instructions carefully is crucial for accurate interpretation.
Fertility Awareness Methods (FAMs)
Fertility awareness methods (FAMs) combine the aforementioned methods (BBT, cervical mucus, and OPKs) to gain a comprehensive understanding of the menstrual cycle and fertility.
- Benefits: FAMs provide a holistic approach to fertility tracking, incorporating multiple indicators to identify the fertile window. This method empowers individuals to understand their own bodies better.
- Limitations: FAMs require consistent monitoring and careful interpretation of various indicators. Significant time and effort are needed to master the method and become proficient in identifying patterns.
- Interpretation: Using multiple indicators increases the reliability of determining the fertile window. Consistency in the combination of symptoms and patterns is crucial for accurate predictions.
Table: Contrasting Fertility Tracking Methods
| Method | Accuracy | Practicality |
|---|---|---|
| BBT | Moderate | Relatively Easy |
| Cervical Mucus | Moderate | Relatively Easy |
| OPKs | High | Easy |
| FAMs | High | Moderate |
Importance of Professional Consultation
It is essential to consult with a healthcare professional for accurate assessments and personalized guidance. A healthcare provider can help interpret results, address concerns, and identify any underlying issues that may impact fertility.
Wondering when your fertility might return after stopping birth control? It really varies, but generally, ovulation and fertility usually return within a few months for most women. However, some women might experience a delay. To get a comprehensive look at your overall health and potentially uncover any underlying factors impacting fertility, a prenuvo full body MRI scan could be a valuable tool.
Prenuvo full body MRI scan results can provide crucial insights that could potentially help you understand your body better and potentially aid in your journey to conceive. Ultimately, talking to your doctor is key to understanding your individual timeline for fertility return after stopping birth control.
Potential Delays and Complications
While many women experience a swift return to fertility after discontinuing birth control, some may encounter delays. Understanding the potential reasons and complications associated with these delays can empower individuals to make informed decisions about their reproductive health. This section delves into the factors that might prolong the return to fertility and highlights the importance of seeking timely medical advice.The journey back to natural fertility after stopping birth control isn’t always a straightforward one.
Wondering when your fertility returns after ditching the birth control pill? It can vary quite a bit, but generally, it takes a few months for your body to get back to its normal rhythm. Interestingly, factors like your overall health, including your mean cell hemoglobin concentration , might play a role in how quickly your body recovers.
So, while some people get pregnant right away, others might take a little longer. Patience and a healthy lifestyle can make a big difference in the process.
Various factors can influence the time it takes for a woman’s body to resume its natural reproductive cycle. These delays, while often temporary, can sometimes signal underlying health concerns, necessitating prompt medical attention.
Potential Reasons for Delayed Fertility Return
Factors influencing the return to fertility after stopping birth control are diverse and multifaceted. Some common causes include the specific type of birth control used, the duration of use, and individual health conditions. Hormonal imbalances, which are frequently associated with certain types of birth control, can take time to normalize.
Possible Complications of Delayed Fertility Return
Delayed fertility return can lead to various complications, ranging from emotional distress to potential long-term health issues. Anxiety, stress, and uncertainty surrounding the timing of pregnancy can negatively impact mental well-being. Further, prolonged delays might indicate underlying health conditions that require medical intervention. It’s important to acknowledge that a delay in fertility return doesn’t necessarily imply infertility, but it warrants attention.
Importance of Seeking Medical Advice
If fertility doesn’t return within a reasonable timeframe after discontinuing birth control, seeking medical advice is crucial. A healthcare professional can assess individual circumstances, rule out potential underlying health issues, and recommend appropriate diagnostic tests and management strategies. A timely evaluation can alleviate anxieties and provide the necessary support to address any concerns efficiently. A physician can help determine if the delay is a temporary fluctuation or a sign of a more significant health issue.
Potential Underlying Health Issues, When does fertility return after stopping birth control
Several underlying health issues can potentially contribute to delays in fertility return after discontinuing birth control. These conditions include polycystic ovary syndrome (PCOS), thyroid disorders, and certain autoimmune diseases. These conditions can impact hormonal balance and ovulation, thereby affecting fertility. It is essential to note that this list is not exhaustive, and a healthcare professional should be consulted for personalized evaluation.
Table of Potential Complications and Associated Symptoms
| Potential Complications | Associated Symptoms |
|---|---|
| Hormonal Imbalances | Irregular periods, mood swings, fatigue, weight changes |
| Polycystic Ovary Syndrome (PCOS) | Irregular periods, ovarian cysts, acne, excess hair growth |
| Thyroid Disorders | Fatigue, weight changes, mood swings, difficulty concentrating |
| Autoimmune Diseases | Joint pain, fatigue, skin rashes, unexplained fevers |
| Stress and Anxiety | Difficulty sleeping, irritability, loss of appetite, decreased libido |
Strategies for Optimizing Fertility Return: When Does Fertility Return After Stopping Birth Control
After discontinuing birth control, the body naturally begins the process of restoring its fertility. However, the timeline and ease of this return can vary significantly. Taking proactive steps to support your body’s natural processes can often enhance and accelerate the return to fertility. These strategies focus on optimizing overall health and well-being, creating a supportive environment for successful conception.
Lifestyle Factors Supporting Fertility
Maintaining a healthy lifestyle is crucial for optimal reproductive health. Proper nutrition and regular exercise are vital components for overall well-being and can directly influence the body’s ability to conceive. A balanced diet rich in essential vitamins, minerals, and antioxidants supports cellular health, including the reproductive system. Exercise promotes circulation, reduces stress, and helps maintain a healthy weight, all of which contribute positively to fertility.
- Balanced Diet: A diet rich in fruits, vegetables, lean proteins, and whole grains provides the necessary nutrients for optimal reproductive health. Limit processed foods, sugary drinks, and excessive caffeine. Consider consulting a registered dietitian for personalized dietary recommendations based on individual needs.
- Regular Exercise: Moderate-intensity exercise, such as brisk walking, swimming, or cycling, can improve cardiovascular health and regulate hormone levels. Avoid extreme or strenuous exercise that could negatively impact fertility.
- Healthy Weight Management: Maintaining a healthy weight range is crucial for reproductive health. Both underweight and overweight individuals may experience difficulties conceiving. Consult a healthcare professional for guidance on achieving and maintaining a healthy weight.
Stress Management and Fertility
Chronic stress can significantly impact fertility by disrupting hormone balance and ovulation cycles. Implementing stress-reducing techniques is essential for optimizing reproductive health. Stress management strategies can range from simple relaxation techniques to more comprehensive therapeutic approaches.
- Stress Reduction Techniques: Incorporate stress-reducing activities into your daily routine, such as meditation, deep breathing exercises, yoga, or spending time in nature. These practices can help regulate stress hormones and promote overall well-being.
- Mindfulness and Relaxation: Mindfulness practices, such as meditation and deep breathing exercises, can help manage stress and improve overall emotional well-being. These techniques can help regulate the body’s stress response and promote hormonal balance.
- Seek Professional Support: If stress levels are consistently high, consider seeking support from a therapist or counselor. They can provide personalized strategies for managing stress and promoting emotional well-being.
Adequate Sleep and Reproductive Health
Adequate sleep is essential for overall health and well-being, including reproductive function. Sufficient sleep helps regulate hormones, supports cellular repair, and enhances the body’s ability to function optimally.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep per night. Establish a consistent sleep schedule and create a relaxing bedtime routine to improve sleep quality.
- Create a Conducive Sleep Environment: Ensure your bedroom is dark, quiet, and cool to promote restful sleep. Minimize exposure to electronic devices before bed.
Information on Ovulation and Cycle
Understanding your ovulation cycle is crucial for optimizing your fertility journey after stopping birth control. Your body’s natural rhythm plays a vital role in conception, and knowing the signs and patterns of your cycle can significantly increase your chances of getting pregnant. This section will explore the ovulation process, typical cycle lengths, signs of ovulation, and the accuracy of ovulation prediction kits.
The Ovulation Process and Fertility
Ovulation is the release of a mature egg from the ovary. This process typically occurs midway through a woman’s menstrual cycle. The egg is then swept into the fallopian tube, where it awaits fertilization by sperm. If fertilization occurs, the egg implants in the uterine lining, initiating pregnancy. If fertilization doesn’t happen, the uterine lining sheds, leading to menstruation.
Ovulation is directly linked to fertility because it’s the point where a woman is most capable of conceiving.
Typical Menstrual Cycle Length and Variations After Stopping Birth Control
The typical menstrual cycle length is 28 days, though it can vary between 21 and 35 days for healthy women. After discontinuing birth control, your cycle might take some time to return to its natural rhythm. Some women experience irregular cycles for a few months. It’s essential to track your cycles to understand your personal pattern. For example, a woman might have a cycle that averages 32 days, and her ovulation typically occurs around day 18.
Signs and Symptoms Associated with Ovulation
Several signs and symptoms can indicate that ovulation is occurring. One common sign is a noticeable increase in cervical mucus, which becomes clear, stretchy, and slippery. This change in mucus helps sperm travel to the egg. Basal body temperature (BBT) is another indicator. A slight increase in BBT, typically 0.5-1°F, after ovulation is a common observation.
Other possible signs include mittelschmerz (ovulation pain), increased libido, and breast tenderness. However, it’s important to note that these signs aren’t always consistent or reliable for every woman.
Ovulation Prediction Kits and Their Accuracy
Ovulation prediction kits (OPKs) measure the surge in luteinizing hormone (LH) in your urine, which typically occurs 24-48 hours before ovulation. These kits can help pinpoint the fertile window of your cycle. OPKs are generally accurate, with results often indicating the day or two before ovulation. However, individual results may vary. For example, a woman might experience a surge on day 12, but ovulation might occur on day 14.
Therefore, relying solely on OPKs for timing intercourse might not be entirely accurate.
Menstrual Cycle and Ovulation Tracking Table
| Day of Cycle | Event | Possible Signs | Impact on Fertility |
|---|---|---|---|
| 1-5 | Menstruation | Heavy bleeding | Low fertility |
| 6-12 | Follicular Phase | Increased cervical mucus, slight changes in BBT | Increasing fertility |
| 13-15 | Ovulation | Surge in LH (detected by OPK), mittelschmerz, increased libido | Peak fertility |
| 16-28 | Luteal Phase | Decreased cervical mucus, sustained BBT increase, possible breast tenderness | Decreasing fertility |
End of Discussion
In conclusion, the return to fertility after stopping birth control is a personalized journey. Factors like age, hormonal variations, and pre-existing conditions significantly impact the timeline. Understanding the types of birth control, methods for tracking fertility, potential delays, and strategies for optimization can empower you to make informed decisions. Remember, consulting a healthcare professional is essential for accurate assessments and personalized guidance throughout this process.
Ultimately, patience and a proactive approach can significantly enhance your chances of a successful return to fertility.