Obsessive compulsive disorder ocd – Obsessive Compulsive Disorder (OCD) affects millions worldwide, characterized by intrusive thoughts and repetitive behaviors. This disorder can significantly impact daily life, but with proper understanding and treatment, individuals can find effective strategies for managing their symptoms and leading fulfilling lives. This exploration dives deep into the complexities of OCD, from defining its key characteristics to examining various treatment approaches and the crucial role of support systems.
This post will explore the different types of obsessions and compulsions associated with OCD, providing clear examples and descriptions. We’ll also discuss the potential biological, psychological, and environmental factors that contribute to its development, offering insights into how OCD can manifest differently across individuals. Furthermore, we’ll look at the diagnostic process and evidence-based treatment options available, including Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP).
Defining Obsessive-Compulsive Disorder (OCD): Obsessive Compulsive Disorder Ocd
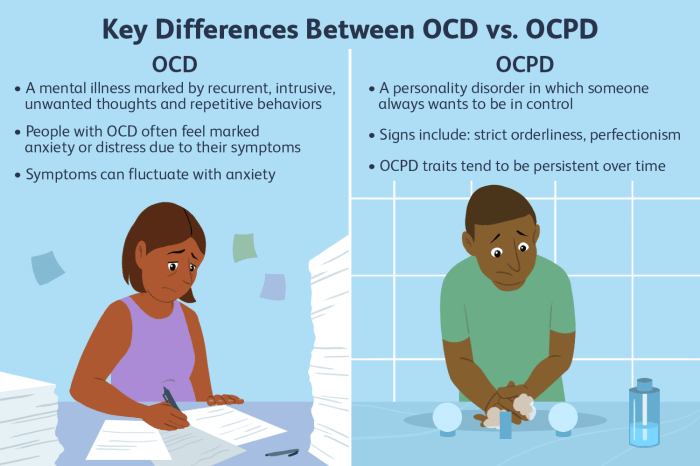
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition characterized by intrusive, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) aimed at reducing anxiety stemming from these thoughts. It’s a complex disorder affecting individuals across diverse backgrounds and impacting various aspects of their lives. Understanding its key characteristics is crucial for recognizing and addressing the condition.OCD is more than just occasional worries or anxieties.
It’s a persistent and debilitating condition that significantly interferes with daily functioning, relationships, and overall well-being. Individuals with OCD experience a relentless cycle of distressing thoughts and behaviors, often leading to significant distress and impairment.
Key Characteristics of OCD
Understanding the distinguishing factors between typical anxieties and OCD is crucial. While everyone experiences anxieties, those with OCD experience them in a markedly different way. OCD’s defining feature is the intrusive and recurring nature of obsessions and the compulsion to engage in repetitive behaviors.
Obsessions
Obsessions are persistent, unwanted thoughts, impulses, or images that intrude upon a person’s mind. These thoughts are often distressing and cause significant anxiety. They’re not simply worries or fears; they are recurrent and difficult to dismiss, often focusing on themes like contamination, doubt, order, symmetry, aggression, or religious or sexual taboo issues.
Compulsions
Compulsions are repetitive behaviors or mental acts that individuals feel driven to perform in response to obsessions. These behaviors are often aimed at reducing anxiety or preventing a feared outcome, but they are not rationally connected to the obsession. Examples include excessive handwashing, checking doors repeatedly, arranging objects meticulously, or counting. The compulsion may seem senseless to others, yet it provides a temporary sense of relief from the anxiety generated by the obsession.
Distinguishing OCD from Normal Anxiety
Normal anxieties are often temporary and situational. They arise in response to specific stressors and typically subside when the stressor is removed. OCD-related anxieties, however, are persistent and intrusive, regardless of the situation. The individual feels compelled to engage in rituals or mental acts to manage these anxieties, even if those rituals don’t logically address the underlying concerns.
Dealing with obsessive-compulsive disorder (OCD) can be tough, sometimes manifesting in unusual ways. For example, certain OCD behaviors might involve rituals surrounding bowel movements, potentially leading to issues like rectal discomfort. Understanding the potential link between OCD and conditions like rectal ulcers is important, and resources like rectal ulcer overview and more can offer valuable insights into potential causes and treatment options.
Ultimately, it’s crucial to remember that managing OCD requires a comprehensive approach, and seeking professional help is key.
The difference lies in the intensity, pervasiveness, and the individual’s inability to control the thoughts and behaviors.
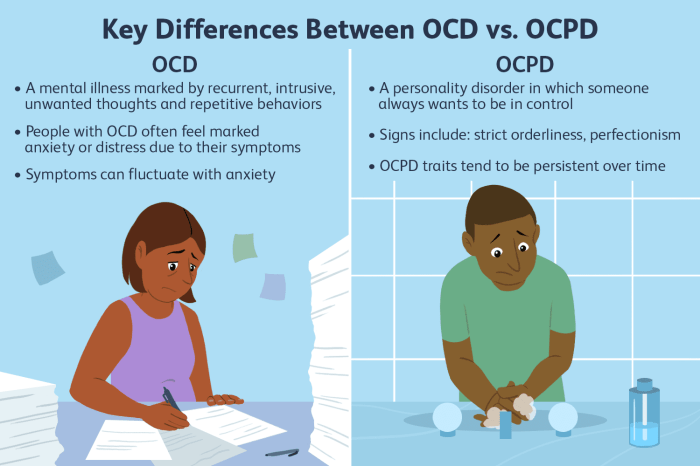
Comparison with Other Anxiety Disorders
OCD shares some overlapping symptoms with other anxiety disorders, such as generalized anxiety disorder (GAD) and panic disorder. However, OCD is distinguished by the presence of obsessions and compulsions. GAD, for example, focuses on general worry and anxiety, while panic disorder involves sudden, intense episodes of fear. OCD, on the other hand, is characterized by a specific cycle of obsessions and compulsions.
DSM-5 Criteria for OCD
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), provides specific criteria for diagnosing OCD. This standardized framework assists clinicians in accurately identifying and treating the disorder.
| Criterion | Description | Example |
|---|---|---|
| Presence of obsessions and/or compulsions | The individual experiences intrusive, unwanted thoughts (obsessions) and/or repetitive behaviors or mental acts (compulsions). | Repeatedly checking locks, washing hands excessively, or arranging objects in a specific order. |
| Obsessions cause marked distress or significantly interfere with daily life | The obsessions significantly disrupt the individual’s daily routine, relationships, or other important areas of life. | Spending hours each day checking and rechecking doors or washing hands to the point of skin irritation. |
| Compulsions are performed to reduce distress or prevent a feared event | The compulsions are performed to relieve the anxiety associated with obsessions. | Washing hands repeatedly to prevent imagined contamination. |
| Time spent on obsessions and compulsions is excessive | The amount of time spent on obsessions and compulsions is clinically significant, consuming a substantial portion of the day. | Spending over an hour each day checking and rechecking doors. |
| The obsessions and compulsions are not attributable to another medical or mental disorder | The symptoms are not better explained by another condition, such as body dysmorphic disorder or another anxiety disorder. | Symptoms are not due to a medical condition or another mental disorder. |
Types and Symptoms of OCD

OCD isn’t a monolithic disorder; it presents in diverse ways. Understanding the different types and their associated symptoms is crucial for accurate diagnosis and effective treatment. This knowledge empowers individuals and their support systems to navigate the complexities of OCD.Understanding the specific obsessions and compulsions can significantly improve the understanding and management of the condition. This knowledge can be vital in tailoring interventions and providing effective support to individuals grappling with OCD.
Types of OCD
OCD manifests in various forms, with recurring themes and patterns emerging. This diversity necessitates a nuanced approach to treatment. Different types of OCD focus on distinct obsessions and compulsions, although overlap is not uncommon. Recognizing these patterns allows for a more personalized and effective treatment strategy.
Common Obsessions in OCD
Obsessions are intrusive and unwanted thoughts, images, or urges that repeatedly pop into a person’s mind. These thoughts often cause significant distress and anxiety. Understanding the range of obsessions allows for better empathy and support for individuals struggling with OCD.
- Contamination: A pervasive fear of germs and contamination is a common theme. Individuals with this type of OCD often experience a heightened sensitivity to dirt, germs, and perceived threats of contamination.
- Doubts: Individuals with doubts-focused OCD may constantly question their actions, decisions, and intentions. This can lead to significant distress and a cycle of repetitive checking and reassurance-seeking.
- Symmetry: An intense need for order, symmetry, and exactness can characterize this type of OCD. The need for perfect alignment, arrangement, or repetition can dominate their thoughts and actions.
- Harm: The fear of causing harm to oneself or others is a prominent obsession in some individuals with OCD. This can involve a constant fear of making mistakes or doing something harmful to oneself or those around them.
Common Compulsions in OCD
Compulsions are repetitive behaviors or mental acts that individuals feel driven to perform in response to obsessions. These behaviors are aimed at reducing anxiety, but they are often ineffective and can worsen the condition. Recognizing these compulsions is crucial for treatment planning and creating effective coping strategies.
- Excessive Handwashing: Repeated handwashing is a common compulsion, often driven by a fear of contamination. This behavior may be performed excessively and cause skin irritation or damage.
- Repeated Checking: Checking behaviors, such as repeatedly checking locks, appliances, or other things, are common compulsions. This can lead to significant time investment and interfere with daily activities.
- Arranging Objects: The need for meticulous arrangement or symmetry can result in compulsive organizing or arranging of objects. This can consume significant time and energy.
- Repetitive Mental Acts: Repetitive mental acts, like counting or praying, can be a compulsion. These mental rituals aim to neutralize the anxiety caused by obsessions but are often ineffective.
Obsessions and Compulsions Table
| Obsession Category | Example Obsession | Corresponding Compulsion |
|---|---|---|
| Contamination | Fear of germs, dirt, bodily fluids | Excessive handwashing, cleaning, avoiding public spaces |
| Doubts | Worrying about forgetting something important, making mistakes | Repeatedly checking things, asking for reassurance, seeking validation |
| Symmetry | Need for things to be perfectly aligned, ordered, or balanced | Arranging objects, counting, repeating actions |
| Harm | Fear of causing harm to oneself or others | Checking locks, repeating safety procedures, excessive apologizing |
| Religious/Moral | Fear of committing a sin, feeling impure | Praying excessively, seeking religious guidance, engaging in ritualistic behaviors |
Causes and Risk Factors
Understanding the root causes of obsessive-compulsive disorder (OCD) is crucial for effective treatment and support. While a single definitive cause remains elusive, research suggests a complex interplay of biological, psychological, and environmental factors. This intricate web of influences shapes the development and manifestation of OCD in individuals.The journey to comprehending OCD’s genesis involves examining various potential contributors, from genetic predispositions to learned behaviors and environmental stressors.
Dealing with obsessive-compulsive disorder (OCD) can be tough, and finding the right mental health care is crucial. Navigating the complexities of health insurance can be overwhelming, but understanding your health insurance provider network is key to finding affordable and accessible treatment options. Ultimately, the right support system is vital for managing OCD effectively.
Unraveling these factors allows for a more nuanced understanding of the condition and its impact on those affected.
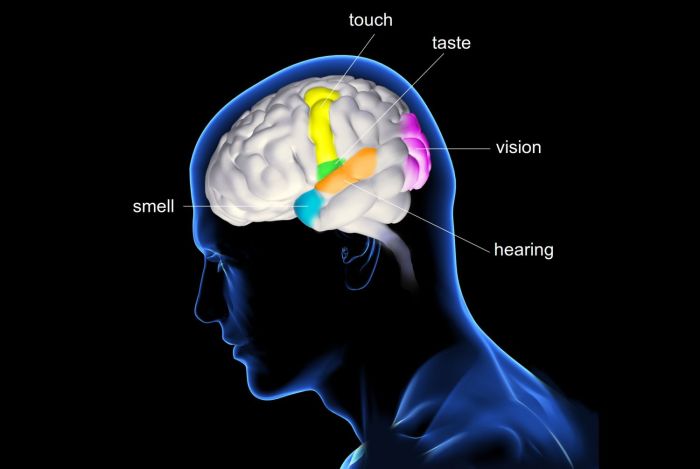
Biological Factors
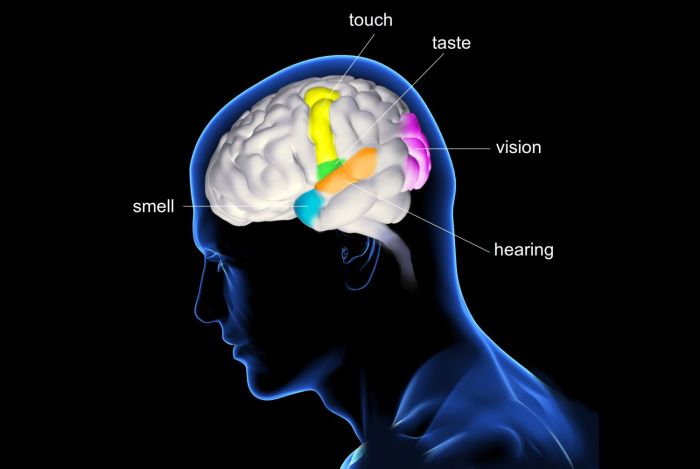
Biological factors are believed to play a significant role in the development of OCD. Neurochemical imbalances, particularly involving serotonin, are often implicated. Serotonin is a neurotransmitter crucial for regulating mood, and disturbances in its function are thought to contribute to obsessive thoughts and compulsive behaviors.Furthermore, structural and functional differences in specific brain regions, such as the orbitofrontal cortex and the caudate nucleus, have been observed in individuals with OCD.
These regions are involved in controlling impulses, planning, and decision-making, and dysregulation in these areas may contribute to the repetitive thoughts and behaviors characteristic of OCD. Studies have also shown increased activity in these brain regions during periods of heightened anxiety and compulsive behavior.
Psychological Factors
Psychological factors can also significantly influence the development and manifestation of OCD. Traumatic experiences, stressful life events, and learned behaviors can all contribute to the emergence of obsessive-compulsive symptoms.For example, a person might develop obsessions about cleanliness after a traumatic experience involving contamination. Similarly, learned behaviors, such as excessive handwashing due to a perceived need for cleanliness, can reinforce compulsive behaviors over time.
These behaviors, while initially possibly motivated by a desire to alleviate anxiety, can become ingrained and difficult to break free from.
Environmental Factors
Environmental factors, such as exposure to certain stressors, infections, or environmental toxins, may also increase the risk of developing OCD. A significant life change, like moving to a new home or the loss of a loved one, can trigger or exacerbate OCD symptoms. Exposure to certain infections during childhood may also be a factor, though more research is needed in this area.
Genetic Factors
Genetic predisposition plays a crucial role in OCD. Family and twin studies have consistently shown a higher concordance rate among individuals with a family history of OCD. This suggests a genetic component, although the exact genes involved are not yet fully understood. Research continues to identify specific genes and genetic variations that might increase vulnerability to OCD.
Interplay of Factors
The development of OCD is likely a complex interaction between biological, psychological, and environmental factors. For example, a genetic predisposition to OCD might make an individual more susceptible to developing the disorder, while a stressful life event could trigger the onset of symptoms. The interplay of these factors creates a unique profile for each individual, explaining why OCD manifests differently in different people.A person with a genetic predisposition might be more likely to experience OCD symptoms after a significant life stressor, compared to someone without that predisposition.
Dealing with obsessive-compulsive disorder (OCD) can be tough, but sometimes, focusing on physical health can be surprisingly helpful. For example, if you’re experiencing hyperpigmentation on your buttocks, understanding what causes it and finding effective solutions like the ones discussed in this helpful guide on hyperpigmentation on buttocks what it is and how to get rid of it can help take your mind off distressing thoughts and improve your overall well-being.
This can, in turn, positively impact your OCD management strategies.
Environmental stressors can exacerbate or trigger symptoms in individuals already genetically predisposed. In essence, the interplay of these factors contributes to the intricate tapestry of OCD’s development.
Diagnosis and Assessment
Unraveling the complexities of obsessive-compulsive disorder (OCD) requires a meticulous diagnostic process. Accurate diagnosis hinges on a thorough understanding of the individual’s experiences, symptoms, and their impact on daily life. This process goes beyond simply identifying symptoms; it aims to understand the underlying patterns and potential contributing factors to the disorder. A comprehensive assessment helps clinicians develop an effective treatment plan tailored to the specific needs of the patient.A comprehensive assessment isn’t a one-size-fits-all approach.
Mental health professionals employ various methods to gain a deep understanding of the individual’s condition. These methods consider the individual’s history, current symptoms, and overall well-being. The ultimate goal is to distinguish OCD from other conditions that might present with similar symptoms, ensuring the most appropriate and effective treatment strategy.
Diagnostic Process Overview
The diagnostic process for OCD typically involves a multi-faceted approach, incorporating interviews, questionnaires, and observations. The goal is to gather a detailed picture of the individual’s experiences and the impact of their symptoms on daily functioning. This holistic approach ensures a more accurate diagnosis and allows for the development of a personalized treatment plan.
Clinical Interviews
Thorough clinical interviews are crucial for understanding the patient’s perspective. Clinicians explore the individual’s history, including past experiences, family history, and any significant life events that might have contributed to the development or exacerbation of OCD symptoms. The interview delves into the nature of the obsessions and compulsions, examining their frequency, intensity, and impact on daily activities. Open-ended questions encourage the patient to elaborate on their experiences, providing valuable insights into the underlying anxieties and motivations behind their behaviors.
Standardized Questionnaires
Standardized questionnaires are employed to provide objective measures of OCD symptoms. These questionnaires assess the severity and frequency of obsessions and compulsions, enabling clinicians to quantify the impact of the disorder on the individual’s life. Examples of such tools include the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) and the Maudsley Obsessive-Compulsive Inventory (MO-CI). These tools provide a consistent and reliable way to assess the severity of symptoms and track progress throughout treatment.
Behavioral Observations
Behavioral observations provide valuable contextual information about the individual’s responses and coping mechanisms. Clinicians observe how the individual interacts with others, performs daily tasks, and manages stressful situations. This observation offers insight into the individual’s behaviors in a naturalistic setting. Observations may also be incorporated during interviews, such as observing the individual’s reactions to specific questions related to their obsessions or compulsions.
Importance of Comprehensive Assessment
A thorough and comprehensive diagnostic process is essential for accurate identification and effective treatment of OCD. Misdiagnosis can lead to inappropriate treatment, hindering progress and potentially exacerbating symptoms. A comprehensive assessment helps clinicians differentiate OCD from other conditions that may present with overlapping symptoms, such as anxiety disorders or tic disorders. This differentiation is critical for developing a targeted and effective treatment strategy.
By meticulously evaluating the individual’s experiences, clinicians can tailor treatment plans to address the specific needs and challenges faced by each patient.
Treatment Approaches for OCD
Unraveling the complexities of Obsessive-Compulsive Disorder (OCD) often leads to a search for effective treatment strategies. Fortunately, a range of evidence-based approaches have proven successful in helping individuals manage their symptoms and improve their quality of life. These methods target both the obsessions and compulsions, aiming to reduce their frequency and intensity.
Evidence-Based Therapies for OCD
Numerous evidence-based therapies demonstrate efficacy in treating OCD. These approaches focus on understanding the underlying mechanisms driving the disorder and providing tools for coping with symptoms. They are often integrated with each other for optimal results.
Cognitive Behavioral Therapy (CBT) for OCD
Cognitive Behavioral Therapy (CBT) is a cornerstone of OCD treatment. It helps individuals identify and challenge negative thought patterns and behaviors that contribute to their obsessions and compulsions. CBT techniques equip individuals with strategies to reframe unhelpful thoughts and develop more adaptive coping mechanisms. For example, through CBT, a person with OCD might learn to identify and challenge the irrational fear that leads to excessive handwashing.
The therapy will provide tools to reframe the fear, and ultimately reduce the compulsive behavior.
Exposure and Response Prevention (ERP) Techniques for OCD
Exposure and Response Prevention (ERP) is a highly effective component of CBT specifically designed for OCD. It involves gradually exposing the individual to feared situations or stimuli related to their obsessions, while simultaneously preventing the performance of their compulsive behaviors. This controlled exposure, combined with the refraining from compulsive acts, helps to break the cycle of obsessions and compulsions.
For example, if a person has an obsession with germs, ERP might involve touching a dirty object (under controlled conditions) and resisting the urge to wash their hands immediately.
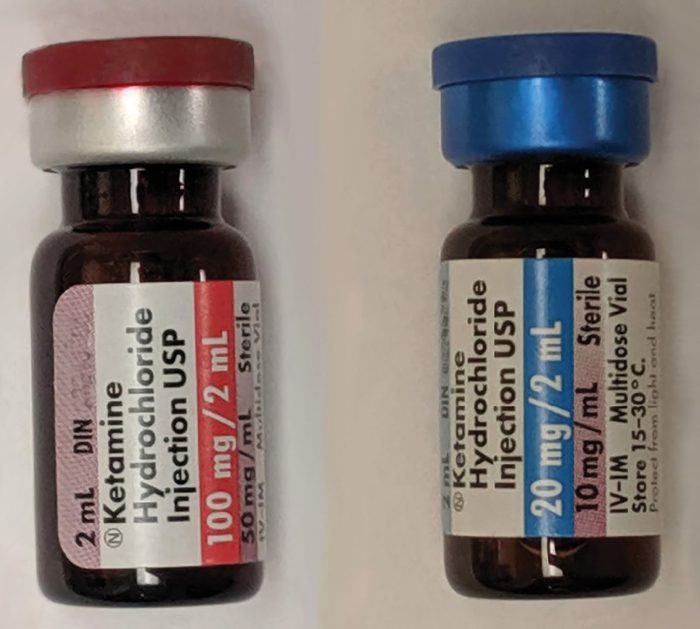
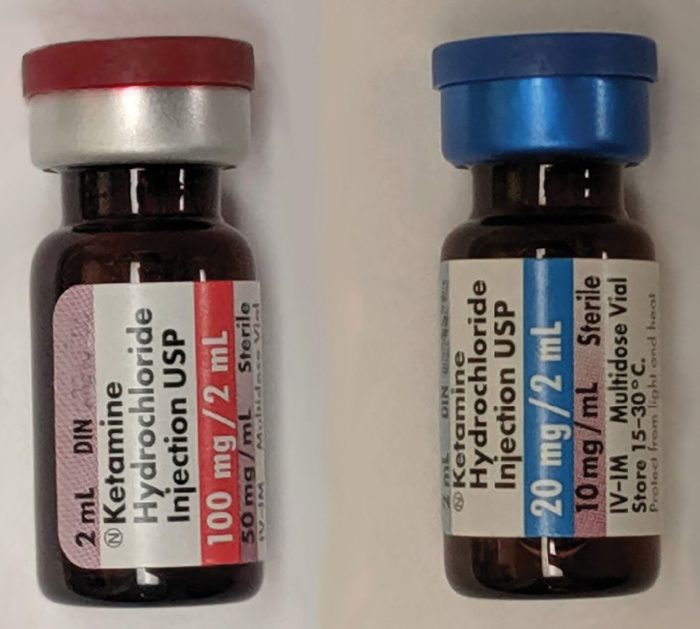
The Role of Medication in Treating OCD
Medication can play a valuable role in conjunction with therapy for some individuals with OCD. Selective serotonin reuptake inhibitors (SSRIs) are frequently prescribed to help regulate serotonin levels in the brain. Serotonin is a neurotransmitter linked to mood and anxiety. By increasing serotonin levels, medication can help reduce the intensity of obsessions and compulsions. Medication is often most effective when combined with behavioral therapies.
Comparison of Treatment Approaches
While CBT, particularly ERP, is often the first-line treatment for OCD, medication may be used to supplement or complement these therapies. CBT equips individuals with coping mechanisms and challenges maladaptive thought patterns, while ERP focuses on breaking the cycle of obsessions and compulsions through exposure and prevention. Medication addresses the neurobiological aspects of the disorder, aiming to reduce the intensity of symptoms.
Table of Treatment Options and Effectiveness
Living with OCD
Living with Obsessive-Compulsive Disorder (OCD) can be challenging, but it’s crucial to remember that effective management is possible. This journey requires understanding your specific symptoms, developing coping mechanisms, and fostering a supportive environment. Acceptance, patience, and a proactive approach are key components in navigating the ups and downs of living with OCD.Living with OCD involves a multifaceted approach to managing symptoms and improving overall well-being.
It’s essential to tailor strategies to individual needs and preferences, recognizing that what works for one person might not work for another. Consistent effort and open communication with healthcare providers are fundamental to progress.
Managing OCD Symptoms
Effective management of OCD symptoms involves a combination of techniques. It’s important to remember that the goal isn’t to eliminate symptoms entirely, but to reduce their impact on daily life. Strategies include exposure and response prevention (ERP), cognitive behavioral therapy (CBT), and mindfulness techniques. These approaches help individuals challenge obsessive thoughts and develop healthier coping mechanisms.
Self-Care Techniques for OCD
Self-care is crucial for individuals with OCD. Prioritizing physical and mental well-being is vital for managing stress and reducing the intensity of OCD symptoms. Regular exercise, a balanced diet, sufficient sleep, and relaxation techniques are integral parts of self-care. Engaging in hobbies and activities that bring joy and a sense of accomplishment also contributes significantly to overall well-being.
Coping Mechanisms for OCD Triggers
Identifying and understanding OCD triggers is essential for developing effective coping mechanisms. Triggers can vary from specific thoughts or situations to environmental factors. Developing a toolbox of coping strategies, such as deep breathing exercises, meditation, or engaging in a calming activity, can help manage the distress associated with triggers. This includes anticipating potential triggers and preparing for them proactively.
Importance of Social Support and Building a Strong Support Network
A strong support network is invaluable for individuals living with OCD. Sharing experiences with others who understand can significantly reduce feelings of isolation and provide encouragement. Open communication with family members, friends, and support groups can foster a sense of belonging and provide practical advice. Connecting with others who share similar struggles can be tremendously beneficial.
Resources for Support Groups or Online Communities
Numerous support groups and online communities cater to individuals with OCD. These platforms offer a space for sharing experiences, providing encouragement, and receiving support from others facing similar challenges. Joining a support group can provide valuable insights, practical strategies, and a sense of community. Online communities offer accessible and convenient support, fostering connections with others who understand the struggles of OCD.
Examples of online communities include specialized forums, social media groups, and support websites.
Understanding OCD from Different Perspectives
OCD isn’t just a set of symptoms; it’s a complex experience shaped by various factors. Understanding these different perspectives – cultural, interpersonal, and personal – is crucial for effective support and treatment. Recognizing how OCD manifests differently across cultures, how it impacts relationships and daily life, and the pervasive nature of stigma are key steps in fostering empathy and providing comprehensive care.Cultural factors significantly influence the expression and experience of OCD.
Different societies may have varying interpretations of obsessive thoughts and compulsive behaviors, which can affect how individuals perceive and address their symptoms. For example, in some cultures, excessive hand-washing might be attributed to religious practices, while in others, it could be perceived as a sign of cleanliness obsession. This can lead to delays in diagnosis and treatment if cultural norms overshadow the need for professional help.
Cultural Influences on OCD
Cultural norms significantly influence how OCD symptoms are perceived and addressed. Cultural values around cleanliness, order, and religion can shape the types of obsessions and compulsions that individuals experience. In cultures emphasizing meticulousness and order, obsessive thoughts about cleanliness and orderliness might be more prevalent. Conversely, in cultures that prioritize spirituality, religious rituals might be misinterpreted as OCD compulsions.
This highlights the importance of culturally sensitive assessments to accurately diagnose and treat OCD.
Impact of OCD on Relationships and Daily Life
OCD can profoundly impact relationships and daily life. The time and energy devoted to obsessions and compulsions can lead to significant disruptions in work, school, and social activities. Individuals with OCD may struggle to maintain healthy relationships as their behaviors can be distressing to partners, family members, and friends. For instance, a person with cleaning compulsions might spend excessive time cleaning, neglecting other responsibilities and impacting their social life.
This illustrates the necessity of support systems and understanding from loved ones.
Impact of Stigma on Individuals with OCD, Obsessive compulsive disorder ocd
The stigma surrounding OCD can significantly hinder individuals’ ability to seek help and maintain a healthy lifestyle. Fear of judgment and misunderstanding can prevent individuals from disclosing their condition, leading to isolation and feelings of shame. This fear of judgment can manifest as reluctance to seek help from a mental health professional or share their experience with others.
This isolation further exacerbates the symptoms and negatively impacts their overall well-being. It’s crucial to combat this stigma through education and awareness campaigns.
Importance of Understanding Diverse Perspectives on OCD
A holistic understanding of OCD requires considering diverse perspectives. This involves recognizing the influence of cultural factors, the impact on relationships, and the pervasive nature of stigma. By understanding these diverse perspectives, healthcare professionals can develop more effective treatment plans tailored to individual needs and cultural contexts. This personalized approach ensures that the treatment addresses not just the symptoms but also the broader challenges faced by individuals with OCD.
Impact of OCD on Self-Esteem and Confidence
OCD’s relentless nature can significantly affect self-esteem and confidence. The constant cycle of obsessions and compulsions can lead to feelings of inadequacy, shame, and self-criticism. Individuals may experience low self-worth and difficulty believing in their ability to manage their symptoms. This is because OCD’s demands often feel overwhelming, leading to a sense of being trapped and powerless.
This reinforces the need for supportive environments and therapeutic interventions to foster a sense of self-worth and empowerment.
Illustrative Case Studies
Understanding OCD through real-life scenarios helps us connect with the challenges individuals face. Case studies, while fictional, provide a glimpse into the complexities of living with OCD and the various forms it can take. They highlight the importance of support systems and effective treatment approaches.Case studies are crucial for illustrating the range of experiences associated with OCD. By presenting a fictional yet relatable individual’s journey, we can better comprehend the emotional and practical struggles of those affected.
This, in turn, fosters empathy and a more nuanced understanding of the condition.
A Fictional Case Study: Sarah’s Struggle
Sarah, a 27-year-old graphic designer, experienced a sudden onset of intrusive thoughts about contamination. These thoughts, often triggered by mundane situations like touching a public doorknob, caused significant anxiety. She developed elaborate cleaning rituals, spending hours meticulously sanitizing her workspace and home, frequently washing her hands, and avoiding public spaces. These compulsive behaviors severely impacted her daily life, leading to missed deadlines at work and strained relationships.
The constant anxiety and time commitment associated with her compulsions left her exhausted and emotionally drained.
Challenges Faced by Individuals with OCD
The challenges faced by individuals with OCD are multifaceted. They often include:
- Intrusive Thoughts and Obsessions: Intrusive thoughts and obsessions, such as fears of contamination, harm, or symmetry, can be pervasive and distressing. These thoughts often trigger intense anxiety and lead to compulsive behaviors.
- Compulsive Behaviors: Compulsive behaviors, like excessive cleaning, checking, or counting, are often employed to reduce the anxiety associated with obsessions. However, these behaviors are often time-consuming and interfere with daily functioning, leading to feelings of helplessness and isolation.
- Impact on Relationships and Daily Life: OCD can significantly impact relationships, work, and overall daily life. Individuals might isolate themselves to avoid triggers or spend excessive time on compulsive behaviors, leading to strained social connections and missed opportunities.
- Emotional Distress: The emotional distress associated with OCD can be significant. Individuals experience anxiety, fear, shame, and guilt, which can affect their self-esteem and mental well-being.
Support Systems for Individuals with OCD
Effective support systems are essential for individuals struggling with OCD. These include:
- Family and Friends: Understanding and supportive family members and friends can provide a crucial emotional safety net. Educating them about OCD can help them offer appropriate support and understanding.
- Professional Help: Seeking professional help from therapists, psychiatrists, or support groups is crucial. Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) are evidence-based treatments that can be highly effective in managing OCD.
- Support Groups: Support groups offer a safe space for individuals with OCD to connect with others who understand their experiences. Sharing stories and coping strategies can provide valuable support and encouragement.
Treatment and Recovery Process
The treatment and recovery process for OCD is a journey that often requires commitment and patience. It typically involves:
- Assessment and Diagnosis: An accurate assessment and diagnosis are crucial for developing a personalized treatment plan. This often involves evaluating the individual’s obsessions, compulsions, and their impact on daily life.
- Therapy: Therapy, such as CBT and ERP, is often a core component of treatment. These therapies aim to challenge obsessive thoughts and reduce compulsive behaviors by gradually exposing individuals to their fears in a controlled environment.
- Medication: In some cases, medication, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed to help manage the symptoms of OCD. Medication is often used in conjunction with therapy.
- Self-Care: Self-care strategies, such as stress management techniques, healthy lifestyle choices, and mindfulness practices, can be helpful adjuncts to treatment.
Summary
In conclusion, Obsessive Compulsive Disorder (OCD) is a complex condition requiring a comprehensive understanding of its various facets. This exploration has provided a framework for understanding the different aspects of OCD, from its defining characteristics to the available treatment options. It’s crucial to remember that seeking professional help is paramount in managing OCD effectively, and building a strong support network is vital for individuals navigating this condition.