Latest weight loss drug Saxenda Liraglutide is a medication that’s gaining attention for its potential to help people achieve their weight loss goals. It works by targeting specific hormones in the body, leading to feelings of fullness and reduced appetite. Understanding the specifics of Saxenda, from dosage to potential side effects, is crucial for anyone considering this treatment option.
This comprehensive guide delves into the specifics of Saxenda, including its mechanism of action, effectiveness, potential side effects, patient considerations, and more. We’ll also explore the long-term effects and maintenance strategies, along with regulatory approvals, cost, and insurance coverage. Whether you’re a potential patient, a healthcare professional, or simply curious about this treatment, this resource aims to provide a thorough overview.
Overview of Saxenda (Liraglutide)
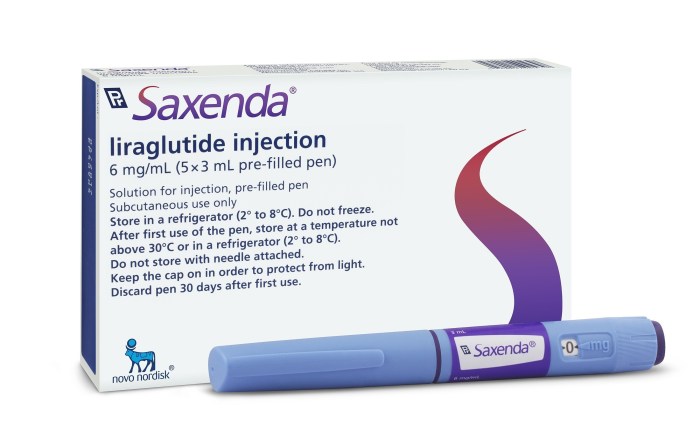
Saxenda, containing the active ingredient liraglutide, is a prescription weight-loss medication. It’s designed for individuals who struggle with obesity or overweight conditions, often in combination with a healthy diet and exercise regimen. This medication works differently from other weight-loss drugs, targeting specific biological pathways in the body to achieve weight management goals.Liraglutide mimics a natural hormone in the body called glucagon-like peptide-1 (GLP-1).
This hormone plays a crucial role in regulating appetite and blood sugar levels. By stimulating GLP-1 receptors, Saxenda helps to reduce hunger and increase feelings of fullness, leading to decreased calorie intake and, consequently, weight loss. The medication also affects the brain, reducing cravings and potentially altering the brain’s reward pathways associated with food.
Dosage and Administration
Saxenda is available in pre-filled injection pens, allowing for precise dosage control. The medication is administered subcutaneously (under the skin) once daily, typically at the same time each day. The dosage is gradually increased over several weeks to allow the body to adjust to the medication.
Available Dosages and Potential Benefits
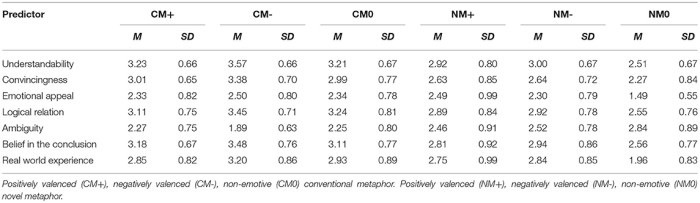
| Dosage (mg) | Administration | Potential Benefits |
|---|---|---|
| 0.6 mg | Once daily subcutaneous injection | Initial dosage, allowing the body to adjust gradually to the medication. |
| 1.2 mg | Once daily subcutaneous injection | Increased dosage, potentially leading to greater weight loss compared to the 0.6 mg dosage. |
| 1.8 mg | Once daily subcutaneous injection | Further increase in dosage, potentially resulting in even more pronounced weight loss. Individual response will vary. |
| 2.4 mg | Once daily subcutaneous injection | Highest dosage, designed for individuals who haven’t achieved sufficient weight loss with lower dosages. Requires careful monitoring. |
| 3.0 mg | Once daily subcutaneous injection | Highest dosage, designed for individuals who haven’t achieved sufficient weight loss with lower dosages. Requires careful monitoring. |
The table above Artikels the various dosages of Saxenda, highlighting the increasing strength as well as the administration method. The gradual increase in dosage allows the body to adapt and minimizes potential side effects. It’s crucial to remember that individual responses to Saxenda vary, and the most effective dosage will depend on the individual’s specific needs and response to treatment.
Effectiveness and Results
Saxenda, a prescription weight-loss medication, has shown promise in helping individuals achieve sustainable weight loss. Its mechanism of action differs from other weight loss drugs, and its impact varies from person to person. Understanding the typical outcomes, comparative effectiveness, and influencing factors is crucial for making informed decisions about this treatment option.Typical weight loss outcomes with Saxenda generally show a moderate degree of success.
Studies have indicated that individuals using Saxenda often experience a significant reduction in weight, which can vary depending on factors like lifestyle and individual metabolic responses. It’s important to remember that weight loss is not linear and may fluctuate throughout treatment.
Weight Loss Outcomes with Saxenda
Saxenda’s effectiveness in promoting weight loss is often measured by the percentage of weight loss compared to baseline. Clinical trials have demonstrated that a significant portion of patients using Saxenda experience a clinically meaningful reduction in weight. However, the degree of weight loss varies significantly among individuals. This variability underscores the importance of personalized approaches to treatment and lifestyle management.
For instance, a patient with a higher baseline weight might see a greater absolute weight loss than someone with a lower baseline weight, but the percentage of weight loss might be similar.
Comparison to Other Weight Loss Medications, Latest weight loss drug saxenda liraglutide
Saxenda’s effectiveness is often compared to other weight loss medications, such as Ozempic (semaglutide), Contrave, and Qsymia. Each medication has its own mechanism of action and associated side effects. While direct comparisons of effectiveness can be complex, some studies suggest that Saxenda can produce comparable weight loss results to other GLP-1 receptor agonists like Ozempic, but individual responses vary.
The optimal choice of medication depends on individual needs and health conditions. Factors like tolerability of side effects, cost, and individual patient characteristics should be considered.
Factors Influencing Saxenda Effectiveness
Several factors can impact the effectiveness of Saxenda. Lifestyle choices, such as diet and exercise, play a crucial role in achieving and maintaining weight loss. Patients who incorporate healthy dietary habits and regular physical activity alongside Saxenda treatment are more likely to experience significant and sustained weight loss. Adherence to the prescribed dosage and consistent lifestyle modifications are key components in optimizing results.
Additionally, underlying health conditions and other medications taken concurrently can influence a patient’s response to Saxenda. Consistent monitoring and communication with healthcare providers are essential.
Comparison Table of Weight Loss Medications
| Medication | Average Weight Loss (lbs) | Common Side Effects | Approximate Cost (per month) |
|---|---|---|---|
| Saxenda (liraglutide) | 10-15 lbs | Nausea, vomiting, diarrhea, constipation, headache, and injection site reactions. | $500-$800 |
| Ozempic (semaglutide) | 10-15 lbs | Nausea, vomiting, diarrhea, constipation, headache, and injection site reactions. | $500-$800 |
| Contrave | 5-10 lbs | Increased heart rate, high blood pressure, depression, anxiety. | $300-$500 |
| Qsymia | 5-10 lbs | Headache, dry mouth, insomnia, high blood pressure, anxiety. | $250-$400 |
Note: The provided cost figures are estimates and can vary based on insurance coverage and individual pharmacy pricing.
Potential Side Effects and Risks
While Saxenda (liraglutide) can be an effective tool for weight management, it’s crucial to understand the potential side effects and risks associated with its use. Knowing these beforehand can help you and your doctor make informed decisions about whether Saxenda is the right choice for you. Understanding the potential risks allows for proactive management and minimizes any negative impacts.The following sections will delve into the common and less common side effects, the potential risks, and the importance of monitoring during treatment.
So, I’ve been researching the latest weight loss drug, Saxenda liraglutide, and it’s fascinating how it works. One important thing to consider, especially when using weight loss medication, is what to eat when you experience side effects. For example, if you have diarrhea as a side effect, be sure to check out this helpful article on Foods to Avoid When You Have Diarrhea.
Understanding what to avoid can really help you manage these side effects effectively, so you can stick with your weight loss goals with Saxenda liraglutide.
This comprehensive overview is designed to empower you with the knowledge needed to navigate the treatment process safely and effectively.
Common Side Effects
Understanding the common side effects is essential for managing expectations and potential discomfort. These effects often subside as your body adjusts to the medication.
- Nausea: This is a frequent side effect, often described as an upset stomach feeling. It typically occurs early in treatment and can be managed with smaller meals, avoiding fatty foods, and taking the medication with food. For instance, some individuals may experience nausea after their first dose but experience no issues after subsequent doses.
- Vomiting: Similar to nausea, vomiting can be a common side effect, particularly during the initial phase of treatment. Strategies to mitigate vomiting include taking Saxenda with meals and avoiding excessive food intake.
- Diarrhea: Diarrhea can also be a common side effect, sometimes accompanied by abdominal cramps. Dietary adjustments and staying hydrated can help alleviate this discomfort.
- Constipation: Conversely, constipation can also occur, highlighting the diverse impact Saxenda can have on the digestive system. Increasing fiber intake and staying hydrated can be helpful in managing this.
- Headache: Headaches are another common side effect, varying in intensity and frequency. Managing stress and maintaining a regular sleep schedule can help.
Less Common Side Effects
These effects are less frequent but still possible. It’s important to be aware of these possibilities to recognize any unusual changes in your body.
I’ve been looking into the latest weight loss drug, Saxenda liraglutide, and it’s fascinating how it works. While researching potential side effects, I stumbled across some information about hematuria, or blood in the urine. It got me thinking about potential links between weight loss medications and urinary issues. If you’re curious about possible causes of hematuria in men, you can find more details on that here: Hematuria Blood in Urine Possible Causes in Men.
Understanding potential side effects like this is crucial when considering any weight loss drug, including Saxenda liraglutide.
- Pancreatitis: Although rare, pancreatitis, an inflammation of the pancreas, is a potential risk. Symptoms can include severe abdominal pain, nausea, and vomiting. Prompt medical attention is crucial if you experience these symptoms.
- Gallbladder problems: Saxenda can potentially affect gallbladder function. If you experience persistent abdominal pain, especially in the upper right quadrant, consult your doctor.
- Kidney problems: While rare, kidney problems have been reported in some individuals taking Saxenda. Regular monitoring of kidney function is crucial, especially for those with pre-existing kidney conditions.
- Thyroid problems: Saxenda may impact thyroid function. Regular thyroid function tests are recommended during treatment.
Potential Risks and Complications
Saxenda, like any medication, carries potential risks and complications. Careful monitoring and open communication with your healthcare provider are vital.
It is essential to report any unusual or concerning symptoms to your doctor immediately.
- Serious allergic reactions: While rare, serious allergic reactions are possible. Symptoms such as hives, swelling, difficulty breathing, or a rapid heartbeat necessitate immediate medical attention.
- Increased heart rate: Some individuals may experience an increase in heart rate. Monitoring this parameter is crucial, especially for those with pre-existing heart conditions.
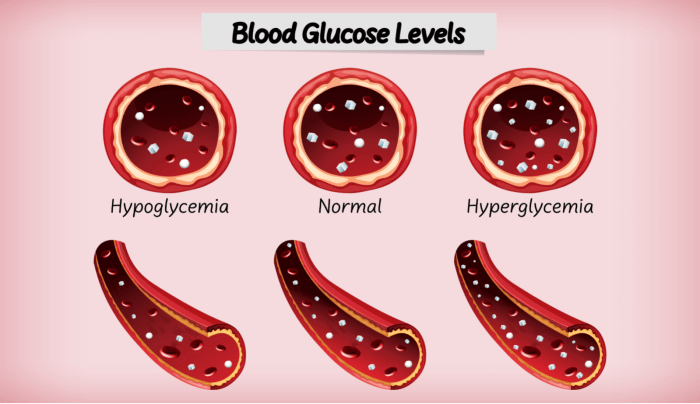
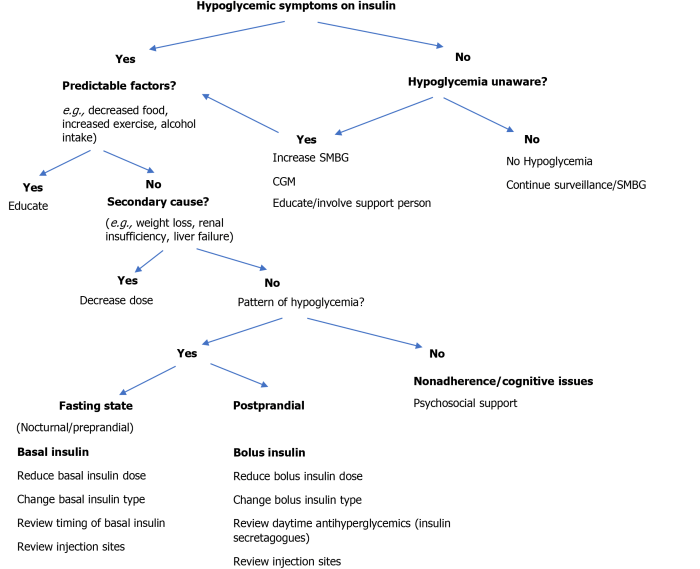
- Changes in blood sugar: Saxenda can affect blood sugar levels. Individuals with diabetes should monitor their blood sugar closely and adjust their medication as needed in consultation with their physician.
Importance of Regular Monitoring
Regular monitoring and follow-up appointments are crucial for safe and effective Saxenda treatment.
- Regular blood tests: Blood tests are essential to monitor kidney and liver function, blood sugar levels, and other relevant parameters.
- Follow-up appointments: Regular check-ups allow your doctor to assess your progress, address any concerns, and adjust the medication dosage as needed.
- Reporting side effects: Reporting any side effects, no matter how minor, is crucial for prompt intervention and adjustment to the treatment plan.
Side Effect Summary Table
| Side Effect | Frequency | Severity | Duration |
|---|---|---|---|
| Nausea | Common | Mild to Moderate | Usually temporary |
| Vomiting | Common | Moderate | Usually temporary |
| Diarrhea | Common | Mild to Moderate | Usually temporary |
| Headache | Common | Mild to Moderate | Usually temporary |
| Pancreatitis | Rare | Severe | Requires immediate medical attention |
| Gallbladder problems | Uncommon | Moderate to Severe | Can be persistent |
Patient Considerations and Selection Criteria
Choosing the right weight loss medication, like Saxenda, is a significant decision. It’s not a one-size-fits-all solution. Understanding your individual needs and potential responses is crucial for successful treatment. Careful consideration of your health history, lifestyle, and expectations is paramount.
Evaluating Potential Saxenda Candidates
Saxenda isn’t appropriate for everyone. Potential candidates must meet specific criteria to ensure the drug’s benefits outweigh the risks. This evaluation process involves a comprehensive assessment by a healthcare professional. Factors considered include body mass index (BMI), presence of other medical conditions, and the patient’s overall health status. Patients with a BMI of 30 or higher, or those with a BMI of 27 or higher with weight-related health concerns, may be considered candidates for Saxenda, but this is not a definitive rule.
The decision is always tailored to the individual patient’s specific circumstances.
Questions to Ask Your Doctor
Before initiating Saxenda treatment, patients should thoroughly discuss potential benefits and risks with their physician. Key questions to explore include the expected outcomes, potential side effects, duration of treatment, and lifestyle modifications needed to maximize efficacy. Understanding the potential for long-term use, or the need for adjustments to the dosage, is also vital. The conversation should encompass potential interactions with existing medications and a thorough review of your medical history.
Furthermore, inquire about the support system available, including dieticians or lifestyle coaches, during and after the treatment period.
Importance of Lifestyle Modifications
Saxenda, like other weight loss medications, works best when combined with healthy lifestyle changes. This includes a balanced diet, regular exercise, and stress management techniques. These lifestyle modifications play a crucial role in long-term weight management and overall health improvement. Maintaining a consistent routine for exercise and nutrition is crucial. It is important to be realistic about potential changes and to find strategies that are sustainable and fit your lifestyle.
A dietitian can provide valuable guidance in developing a tailored meal plan and an exercise routine.
I’ve been reading up on the latest weight loss drug, Saxenda liraglutide, and its potential side effects. It’s a complex topic, and understanding underlying conditions like Hypothyroidism and Adrenal Insufficiency A Deep Dive can be crucial when considering such treatments. For a comprehensive look at these conditions, check out this helpful resource: Hypothyroidism and Adrenal Insufficiency A Deep Dive.
Ultimately, consulting a doctor is essential before starting any weight loss medication, especially if you suspect any underlying health issues.
Patient Considerations
- Thorough medical evaluation: A complete medical history, including any pre-existing conditions or allergies, is essential for determining suitability for Saxenda. This includes a discussion of any other medications you are currently taking.
- Realistic expectations: Saxenda is a tool, not a magic bullet. Success with the drug requires a commitment to lifestyle changes and consistent effort.
- Regular monitoring: Ongoing monitoring of blood sugar levels, blood pressure, and other relevant parameters is necessary during treatment to track progress and identify any potential complications.
- Supportive environment: Building a support system that includes a healthcare team, family, or friends can significantly impact the success of treatment.
- Potential side effects: Be prepared to discuss potential side effects, such as nausea, vomiting, or constipation. A proactive discussion about managing these side effects with your physician is crucial.
- Lifestyle modifications: A commitment to healthy dietary habits, regular exercise, and stress management is vital for optimizing results and long-term weight maintenance. The development of sustainable habits is key.
Medical Professional Considerations
Prescribing Saxenda (liraglutide) requires careful consideration of individual patient needs and potential risks. Healthcare providers must thoroughly assess patients’ medical history, current health status, and lifestyle factors to determine suitability for this medication. This includes a comprehensive evaluation of potential contraindications and precautions, as well as an understanding of potential drug interactions. Understanding these factors is crucial for optimizing treatment outcomes and minimizing adverse events.Healthcare professionals play a pivotal role in guiding patients toward successful weight management.
The decision to prescribe Saxenda should be based on a detailed evaluation of the patient’s specific circumstances and goals, taking into account their individual response to treatment, potential side effects, and the possibility of interactions with other medications.
Contraindications
Contraindications are situations where a medication should absolutely not be used. In the case of Saxenda, contraindications are carefully defined to prevent serious health risks. These restrictions are designed to protect patients with specific medical conditions that may be negatively impacted by the medication.
- Patients with a known hypersensitivity or allergy to liraglutide or any of the excipients in Saxenda should not receive the medication. This is a critical safety measure to prevent allergic reactions.
- Individuals with a history of pancreatitis or those currently experiencing acute pancreatitis should avoid Saxenda, as it may exacerbate the condition.
- People with a history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 should not use Saxenda. This is due to a potential link between these conditions and the risk of thyroid cancer.
Precautions
Precautions are important considerations that necessitate careful monitoring and adjustments to treatment plans. Healthcare providers must be vigilant about these factors to mitigate potential risks.
- Patients with a history of gallbladder disease, renal impairment, or cardiovascular issues should be carefully monitored during Saxenda treatment. Close monitoring of vital signs and potential complications is crucial.
- Patients with a history of depression or suicidal ideation should be closely monitored for any worsening of these conditions. The patient’s mental health status should be regularly assessed during Saxenda treatment.
- Individuals with a history of diabetic retinopathy should be aware that Saxenda may potentially affect their eye condition and may require careful monitoring and adjustments to their diabetic treatment plan.
Potential Drug Interactions
Understanding potential interactions between Saxenda and other medications is crucial for optimizing treatment outcomes and minimizing adverse effects. Carefully assessing concomitant medications is vital to ensure patient safety.
- Saxenda may interact with medications affecting the gastrointestinal tract, potentially altering the absorption or metabolism of other drugs. This is particularly relevant when prescribing Saxenda alongside medications for other conditions.
- There is a potential interaction with medications that may lower blood pressure, requiring close monitoring of blood pressure readings during treatment. The healthcare professional must adjust the dosage or treatment plan as necessary.
- Saxenda may influence the efficacy of other diabetes medications, which necessitates a careful review of the patient’s current treatment plan to adjust the dose and monitor for appropriate response.
Summary Table
| Category | Description |
|---|---|
| Contraindications |
|
| Precautions |
|
| Potential Drug Interactions |
|
Long-Term Effects and Maintenance

Saxenda, while effective for initial weight loss, requires a commitment to long-term strategies for sustained results. Understanding the potential long-term effects and developing a plan for maintenance is crucial for those considering or using this medication. Simply stopping Saxenda doesn’t guarantee that the weight loss will be permanent. Maintaining a healthy lifestyle, including dietary habits and exercise, is essential for long-term weight management.The effects of Saxenda on weight loss can vary, with some individuals experiencing a significant reduction in weight, while others might see more moderate changes.
Understanding the factors that contribute to individual outcomes is critical for realistic expectations and developing a tailored approach to long-term weight management.
Maintaining Weight Loss After Discontinuing Saxenda
Weight loss achieved with Saxenda is often not maintained indefinitely after the medication is stopped. This is a common observation in many weight management strategies. Individuals must adopt long-term lifestyle changes to prevent regaining the lost weight.
Strategies for Long-Term Weight Management Beyond Saxenda
Beyond the use of Saxenda, long-term weight management involves a multifaceted approach encompassing dietary modifications, physical activity, and behavioral strategies. These strategies are designed to create sustainable habits that promote and maintain a healthy weight.
Dietary Adjustments for Long-Term Weight Management
Adopting a balanced and nutritious diet is fundamental to long-term weight management. A balanced diet should be low in processed foods, sugary drinks, and unhealthy fats, while being rich in fruits, vegetables, lean proteins, and whole grains. A registered dietitian can provide personalized dietary plans tailored to individual needs and preferences.
- Prioritize whole, unprocessed foods over highly processed options.
- Control portion sizes to avoid overeating.
- Focus on nutrient-dense foods to maximize satiety.
- Reduce intake of sugary drinks and desserts.
- Include lean protein sources in each meal to support satiety and muscle maintenance.
- Choose healthy fats, such as avocados, nuts, and olive oil.
Physical Activity and Exercise
Regular physical activity is essential for maintaining weight loss and improving overall health. This includes incorporating a variety of activities that you enjoy, such as brisk walking, jogging, swimming, cycling, or dancing.
- Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Incorporate strength training exercises two or more times per week to build muscle mass.
- Find activities that you enjoy to make exercise sustainable.
- Gradually increase the intensity and duration of workouts as your fitness improves.
Behavioral Strategies for Long-Term Weight Management
Behavioral strategies are essential for maintaining motivation and healthy habits over time. These strategies help individuals develop coping mechanisms and address potential challenges in weight management.
- Seek support from friends, family, or support groups to stay motivated.
- Develop coping mechanisms to manage stress and emotional eating.
- Establish realistic goals and celebrate small victories.
- Schedule regular check-ups with your healthcare provider to monitor progress and address any concerns.
Regulatory Approvals and Safety Data
Saxenda, a liraglutide-based weight loss medication, has undergone rigorous scrutiny by regulatory bodies worldwide. Understanding the approval process and the long-term safety data is crucial for anyone considering this treatment. This section delves into the details of these approvals and the safety profile emerging from extensive clinical trials.
Regulatory Approvals by Region
The approval of Saxenda varies across different countries due to differing regulatory requirements and healthcare priorities. These approvals are based on evidence from clinical trials demonstrating the drug’s effectiveness and safety. Different countries may impose specific usage guidelines or restrictions based on their unique health landscapes.
- The European Medicines Agency (EMA) approved Saxenda for use in several European countries, citing its efficacy in weight management and its safety profile.
- In the United States, the Food and Drug Administration (FDA) approved Saxenda for chronic weight management, based on trials showing the drug’s effectiveness and tolerability.
- Various other countries, including Australia and Canada, have also approved Saxenda, reflecting a global consensus on its potential benefits.
Long-Term Safety Studies
Extensive long-term studies are essential to assess the potential long-term effects of Saxenda. These studies monitor participants over several years, analyzing potential side effects, drug interactions, and overall health outcomes. Findings from these trials contribute to a comprehensive understanding of the drug’s safety profile.
- Long-term safety studies have generally shown a positive safety profile, with reported side effects largely aligning with those observed during shorter-term trials. However, specific patient populations may exhibit different responses.
- Some of the side effects reported in clinical trials include nausea, vomiting, and diarrhea. These are often manageable with lifestyle adjustments and appropriate medical intervention.
- Studies on cardiovascular outcomes have not shown an increased risk of serious cardiovascular events, but more research is always needed to further confirm this.
Summary of Latest Research Findings
Recent research continues to investigate the long-term effects of Saxenda and its potential impact on various health parameters. The focus is on understanding the long-term safety profile and optimizing the drug’s efficacy for specific patient groups.
- Research is ongoing to investigate the potential impact of Saxenda on diabetes management and other related health conditions.
- Scientists are also studying how Saxenda affects specific metabolic pathways, providing deeper insight into its mechanism of action.
- New studies are exploring the potential use of Saxenda in combination with other therapies for improved weight loss outcomes.
Regulatory Approvals Table
| Country | Regulatory Body | Approval Date | Conditions of Use |
|---|---|---|---|
| United States | FDA | [Insert Date] | Chronic weight management in adults with obesity or overweight with a related health condition |
| European Union | EMA | [Insert Date] | Weight management in adults with obesity or overweight with a related health condition |
| Australia | TGA | [Insert Date] | Weight management in adults with obesity or overweight with a related health condition |
| Canada | Health Canada | [Insert Date] | Weight management in adults with obesity or overweight with a related health condition |
Note: Specific dates and conditions of use are subject to change. Consult official regulatory documents for precise information.
Cost and Insurance Coverage: Latest Weight Loss Drug Saxenda Liraglutide
Saxenda, while potentially effective for weight loss, can be a significant financial investment. Understanding the cost and available insurance coverage is crucial for patients considering this treatment. This section delves into the typical pricing, insurance options, and the broader financial implications of using Saxenda.
Typical Cost of Saxenda
The cost of Saxenda varies depending on the prescription dosage and the pharmacy. It’s important to note that prices are not publicly listed, and the out-of-pocket cost for a patient will depend on their specific insurance coverage. Patients should contact their pharmacy or healthcare provider to determine the exact price.
Insurance Coverage Options for Saxenda
Insurance coverage for Saxenda, like any prescription medication, can vary significantly. Coverage is not guaranteed and depends on individual plans and provider networks. The specifics of coverage are complex and often dependent on factors like pre-authorization requirements, prior authorization for coverage, and the patient’s specific medical history and needs. Patients should contact their insurance provider directly to confirm coverage.
Financial Implications of Using Saxenda
The financial implications of using Saxenda extend beyond the medication’s price. Co-pays, deductibles, and out-of-pocket maximums can add to the overall cost. Additionally, if Saxenda is not fully covered, patients may face significant expenses. The total cost often includes not only the medication but also potential costs associated with follow-up appointments, lifestyle changes, and other related medical expenses.
Patients should carefully assess their individual financial situations and weigh the costs against the potential benefits.
Potential Insurance Coverage Options Table
| Insurance Plan Type | Coverage Criteria | Potential Financial Implications |
|---|---|---|
| High-deductible health plans (HDHPs) | Often require meeting a high deductible before coverage begins. Co-pays and coinsurance may apply. | High upfront costs before coverage begins, potentially leading to significant out-of-pocket expenses. |
| PPO plans | Generally offer broader coverage networks, but coverage for Saxenda might still depend on specific formulary inclusions. | Potential for co-pays and coinsurance, but broader coverage than other plans. |
| HMO plans | Typically require using in-network providers and may have specific formulary restrictions for Saxenda. | Potential for higher costs if Saxenda is not on the plan’s formulary. Requires adherence to the in-network provider system. |
| Medicare/Medicaid | Coverage depends on specific plan provisions and the patient’s medical needs. Detailed review of individual plans is essential. | Potential for limited or partial coverage. Contacting the respective plan provider is crucial. |
Outcome Summary
In conclusion, Saxenda Liraglutide offers a targeted approach to weight management, but it’s not a magic bullet. Understanding the nuances of this medication, including its potential benefits, side effects, and long-term considerations, is essential. Ultimately, the decision to use Saxenda should be made in consultation with a healthcare professional. Remember, a healthy lifestyle, including a balanced diet and regular exercise, is crucial for long-term weight management, regardless of any medication used.