General adaptation syndrome overview explores the body’s response to stress. This fascinating process, often overlooked, has profound implications for our well-being. We’ll delve into the three stages of this response – alarm, resistance, and exhaustion – and how our bodies react physiologically to various stressors. Understanding these stages can equip us with strategies to better manage stress and safeguard our health.
From the initial alarm reaction to the prolonged wear and tear of resistance, and finally the potentially damaging exhaustion phase, we’ll examine the complex physiological mechanisms at play. We’ll explore the impact of stressors, both acute and chronic, and how individual differences influence our responses. We’ll also investigate the crucial role of social support and lifestyle modifications in mitigating the negative effects of stress.
Introduction to General Adaptation Syndrome (GAS)
General Adaptation Syndrome (GAS) is a physiological response to stress. It describes the predictable ways the body adapts to various stressors, be they physical or psychological. Understanding GAS helps us appreciate the interconnectedness of our physical and mental well-being, and how chronic stress can impact our health. It’s a crucial concept in understanding how the body reacts to prolonged challenges.This model Artikels how the body copes with stressors.
It is characterized by three distinct stages: alarm, resistance, and exhaustion. Each stage involves specific physiological changes, which, if prolonged, can lead to adverse health outcomes. Understanding these stages is vital in managing stress and promoting overall health and well-being.
The Alarm Stage
The alarm stage is the initial response to a stressor. The body mobilizes its resources to combat the perceived threat. This stage is characterized by the activation of the sympathetic nervous system, triggering a cascade of physiological responses designed to prepare the body for “fight or flight.”Physiological responses in this stage include increased heart rate and blood pressure, elevated levels of adrenaline and cortisol, and a diversion of blood flow to the muscles.
These changes provide a surge of energy, preparing the body for immediate action. For example, encountering a sudden loud noise might cause an immediate increase in heart rate and blood pressure, preparing the body to respond quickly.
Understanding the general adaptation syndrome (GAS) is crucial for managing stress. It’s a fascinating three-stage response to stressors, but sometimes our bodies react in unexpected ways, like when using CBD oil and potentially facing issues with drug tests. For example, the effects of CBD oil on the body can sometimes be complex and may interact with standard drug-screening protocols, as detailed in this resource on cbd oil and failing drug tests.
Ultimately, understanding GAS helps us appreciate how our bodies cope with various challenges.
The Resistance Stage
The resistance stage follows the alarm stage, and it is characterized by the body’s attempt to adapt to the sustained stressor. The body continues to maintain an elevated level of physiological arousal, but the initial intense response subsides.During this stage, the body tries to return to homeostasis while still dealing with the stressor. This can involve the release of stress hormones, such as cortisol, to maintain energy levels.
The body’s resources are mobilized to cope with the stressor, which often leads to increased blood pressure and muscle tension. For example, someone enduring a prolonged period of work stress may exhibit elevated cortisol levels and a persistent feeling of tension.
The Exhaustion Stage
The exhaustion stage occurs when the body’s resources are depleted after prolonged exposure to a stressor. The body’s ability to adapt and resist further stress is significantly diminished.In this stage, the body’s coping mechanisms fail, and the physiological responses associated with the alarm and resistance stages become unsustainable. This leads to a range of negative health consequences, including immune system suppression, cardiovascular problems, and increased susceptibility to illness.
Chronic stress and prolonged exposure to high levels of stress hormones can lead to exhaustion, where the body’s ability to cope is overwhelmed.
Comparison of Physiological Responses Across Stages
| Stage | Physiological Response |
|---|---|
| Alarm | Increased heart rate and blood pressure, elevated adrenaline and cortisol levels, redirection of blood flow to muscles, heightened senses. |
| Resistance | Continued elevated cortisol levels, sustained muscle tension, increased blood pressure, and resource mobilization to cope with the stressor. |
| Exhaustion | Depleted resources, impaired immune function, increased vulnerability to illness, cardiovascular issues, and mental health problems. |
Factors Affecting GAS
The General Adaptation Syndrome (GAS) describes the body’s response to stress, a common experience in modern life. Understanding the factors influencing this response is crucial for recognizing and managing stress-related health issues. This section delves into the primary stressors, individual variations, and the impact of chronic versus acute stress on GAS, alongside the role of social support.Stressors are not uniform in their effects; some trigger mild responses, while others induce significant physiological changes.
Individual differences in coping mechanisms, personality traits, and prior experiences play a substantial role in determining the intensity and duration of the stress response. Furthermore, the nature of the stressor itself—whether acute or chronic—influences the body’s adaptation. The presence of social support systems can significantly moderate the GAS response, offering resilience and buffering against the negative consequences of stress.
Primary Stressors Triggering GAS
Various factors can act as stressors, initiating the GAS response. These include significant life events like job loss, relationship issues, or the death of a loved one. Daily hassles, such as traffic jams, financial worries, or interpersonal conflicts, can also contribute to stress. Environmental stressors, like natural disasters or exposure to pollution, can exert a substantial impact.
The perception of a stressor plays a critical role; what one person finds challenging, another may find manageable.
Understanding the general adaptation syndrome (GAS) is key to managing stress, but for those with type 2 diabetes, it’s especially important to have a clear medication reference chart. This helps patients navigate the complexities of their treatment plan, like the one found on medication reference chart for type 2 diabetes. Ultimately, a solid understanding of GAS, combined with a well-managed medication regimen, is crucial for overall health and well-being.
Individual Differences in GAS Responses
Individual variations in the GAS response are substantial. Factors such as personality traits, coping mechanisms, and prior experiences influence how individuals perceive and respond to stressors. For example, individuals with high levels of optimism and strong social support networks often exhibit a more resilient response to stress compared to those with lower levels of coping resources. Genetic predispositions may also contribute to varying stress responses, impacting the efficiency of physiological systems.
Impact of Chronic vs. Acute Stress on GAS
The duration of stress exposure significantly impacts the GAS response. Chronic stressors, such as ongoing financial difficulties or a strained relationship, lead to prolonged activation of the stress response. This sustained activation can have detrimental effects on physical and mental health, potentially leading to burnout, cardiovascular issues, or depression. Acute stressors, such as a sudden car accident or a public speaking engagement, trigger a more short-lived stress response.
While potentially intense, the acute response is typically less damaging if effectively managed.
Influence of Social Support on GAS
Social support plays a vital role in mitigating the impact of stress on the GAS response. Having supportive relationships, whether with family, friends, or community groups, provides emotional buffering and practical assistance during challenging times. Strong social connections provide a sense of belonging, reduce feelings of isolation, and foster a sense of control over the situation. This support can lessen the perceived threat and facilitate more effective coping strategies.
Categorization of Stressors and their Potential Impact on GAS
| Type of Stressor | Description | Potential Impact on GAS |
|---|---|---|
| Significant Life Events | Major life transitions (e.g., marriage, divorce, job loss, death of a loved one) | High potential for prolonged and intense GAS response, impacting physical and mental health. |
| Daily Hassles | Everyday frustrations and annoyances (e.g., traffic, deadlines, interpersonal conflicts) | Can contribute to chronic stress and gradual wear and tear on the body. |
| Environmental Stressors | External factors like natural disasters, pollution, or extreme temperatures | Potentially trigger acute or chronic GAS depending on the severity and duration of exposure. |
| Work-Related Stress | Job demands, pressure, and lack of control over work | Can lead to chronic stress and impact various aspects of physical and mental well-being. |
| Relationship Conflicts | Disagreements and difficulties in interpersonal relationships | Can trigger acute or chronic stress, depending on the severity and frequency of conflicts. |
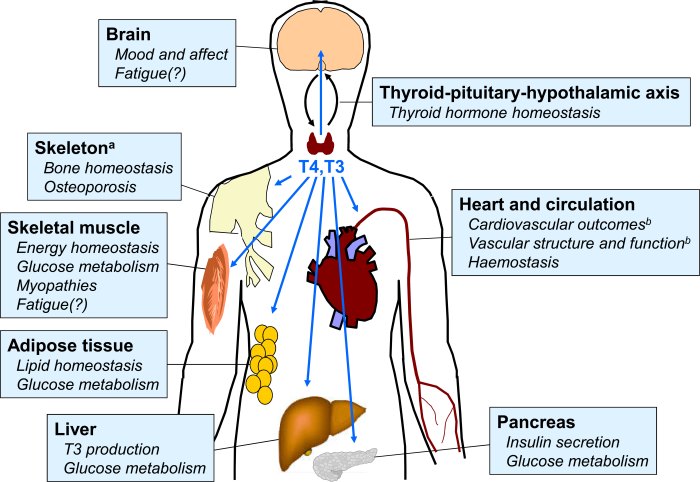
Physiological Mechanisms in GAS
The General Adaptation Syndrome (GAS) isn’t just about feeling stressed; it’s a complex physiological response involving intricate hormonal and nervous system mechanisms. Understanding these processes helps us grasp how our bodies react to stressors, from everyday hassles to major life events. This intricate interplay of systems shapes our response to stress, and its dysregulation can contribute to various health problems.The physiological mechanisms underpinning GAS are deeply interconnected.
Hormonal responses, the autonomic nervous system, and the hypothalamic-pituitary-adrenal (HPA) axis all play critical roles in orchestrating the body’s stress response. The activation of these systems is triggered by perceived threats, and their intensity is often proportional to the perceived severity of the stressor.
Hormonal Responses in Each Stage
The body’s hormonal responses shift dramatically across the three stages of GAS. In the alarm stage, the primary hormonal surge is driven by the release of catecholamines, particularly adrenaline and noradrenaline. These hormones prepare the body for immediate action, increasing heart rate, blood pressure, and blood flow to muscles. During the resistance stage, the body tries to adapt to the chronic stressor.
Cortisol, a steroid hormone released by the adrenal cortex, plays a key role in this phase, providing the body with energy and suppressing the immune system. The exhaustion stage sees the body’s resources depleted, leading to a decline in hormonal production and a vulnerability to illness and disease.
Role of the Autonomic Nervous System
The autonomic nervous system is the primary orchestrator of the body’s fight-or-flight response, a crucial component of the alarm stage of GAS. It’s divided into two branches: the sympathetic and parasympathetic nervous systems. The sympathetic nervous system activates the “fight-or-flight” response, mobilizing the body’s resources for immediate action. The parasympathetic nervous system, conversely, is responsible for returning the body to a state of rest and relaxation.
This delicate balance between the two systems is essential for maintaining homeostasis.
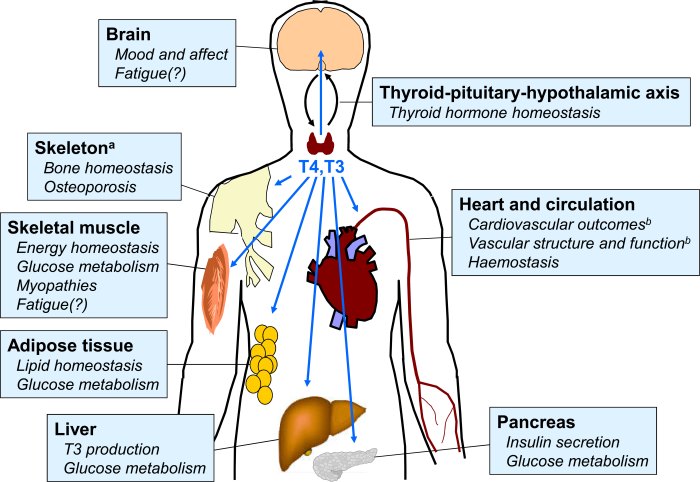
Impact of the HPA Axis
The hypothalamic-pituitary-adrenal (HPA) axis is a complex neuroendocrine pathway that plays a central role in the body’s stress response, especially in the resistance and exhaustion stages of GAS. The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH then triggers the release of cortisol from the adrenal cortex. This cascade of hormonal releases provides the body with sustained energy and helps regulate various physiological functions.
Diagram of the HPA Axis
<img src="hpa_axis_diagram.png" alt="Diagram of the HPA Axis" width="400" height="300">
The diagram above illustrates the HPA axis, depicting the hypothalamus, pituitary gland, and adrenal glands. Arrows indicate the direction of hormonal signals. The hypothalamus releases CRH, which triggers the pituitary to release ACTH. ACTH then stimulates the adrenal glands to produce cortisol.
Implications of GAS in Health

The General Adaptation Syndrome (GAS) provides a framework for understanding how the body responds to stress. However, prolonged or excessive stress, as dictated by the GAS stages, can have significant and detrimental effects on various aspects of health. Understanding these implications is crucial for developing strategies to mitigate the negative consequences of stress.The body’s response to stress, while initially adaptive, can become detrimental if the stressor persists.
This prolonged activation of the stress response system, as Artikeld in the GAS model, can lead to a cascade of physiological changes that contribute to various health problems. These changes range from minor discomfort to severe diseases, highlighting the importance of managing stress effectively.
Relationship between GAS and Health Problems
The continuous activation of the stress response, characteristic of prolonged stress, can lead to a weakening of the body’s systems. This can manifest in a variety of health problems, impacting both physical and mental well-being. Chronic stress has been linked to a heightened risk of cardiovascular diseases, weakened immunity, and even certain types of cancers.
Impact of Prolonged Stress on Physical Health
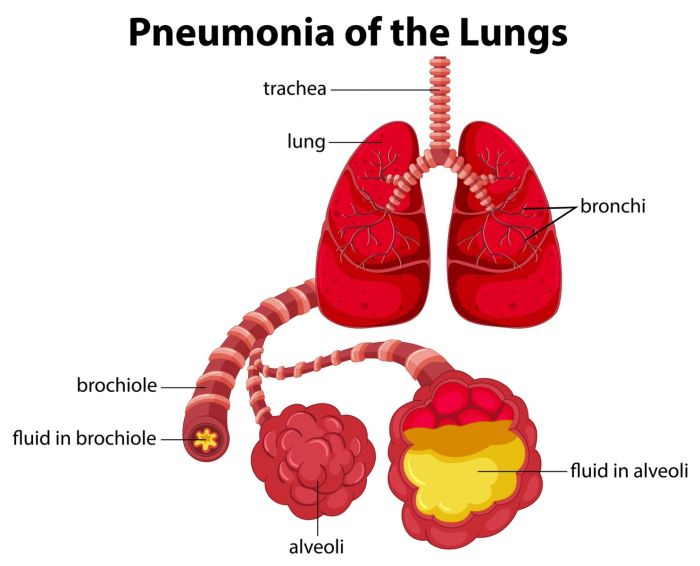
Prolonged stress, a key factor in GAS, has a substantial impact on physical health. The sustained release of stress hormones like cortisol can lead to various physical ailments. For example, individuals experiencing chronic stress may exhibit hypertension (high blood pressure), leading to cardiovascular complications. Furthermore, the immune system can become compromised, increasing susceptibility to infections and slowing wound healing.
Gastrointestinal issues, such as ulcers and irritable bowel syndrome, are also frequently associated with prolonged stress. This highlights the need for stress management techniques to prevent these negative consequences.
Role of GAS in Mental Health Disorders
Chronic stress, a central element in the GAS model, is a significant risk factor for the development of mental health disorders. Prolonged activation of the stress response system can disrupt the delicate balance of neurochemicals in the brain, potentially leading to conditions like anxiety disorders, depression, and post-traumatic stress disorder (PTSD). The cumulative impact of stress on the brain over time can significantly affect emotional regulation and mental well-being.
Understanding this relationship is crucial for early intervention and effective treatment strategies.
Connection between Stress and the Immune System
The immune system is significantly influenced by the body’s stress response. Prolonged stress, as predicted by GAS, can suppress the immune system’s function. This suppression can lead to a weakened defense against pathogens, increasing susceptibility to illnesses. Stress hormones like cortisol can interfere with the production and activity of immune cells, creating a vulnerable environment for infections.
This emphasizes the critical link between mental and physical health and the importance of stress management in maintaining a robust immune response.
Potential Health Consequences of Prolonged Stress
| Health Problem | Connection to GAS |
|---|---|
| Cardiovascular Disease | Sustained stress response elevates blood pressure and cholesterol levels, increasing risk of heart disease and stroke. |
| Gastrointestinal Issues | Chronic stress can disrupt the digestive system, leading to conditions like ulcers, irritable bowel syndrome, and indigestion. |
| Weakened Immunity | Prolonged stress suppresses the immune system, making individuals more susceptible to infections and slower wound healing. |
| Mental Health Disorders | Chronic stress can contribute to the development of anxiety, depression, and PTSD by disrupting the brain’s neurochemistry. |
| Sleep Disturbances | The physiological arousal associated with chronic stress can interfere with the body’s natural sleep-wake cycle, resulting in insomnia or poor sleep quality. |
Coping Strategies and Interventions
Navigating the stress response and mitigating the impact of General Adaptation Syndrome (GAS) requires proactive coping mechanisms and lifestyle adjustments. Understanding the physiological processes involved allows for the development of personalized strategies to foster resilience and well-being. Effective interventions often involve a combination of techniques to manage stress triggers and promote overall health.
Understanding the general adaptation syndrome (GAS) is key to comprehending how our bodies react to stress. It’s a fascinating process, but what about something like allergy shots? Recent research has explored the safety of 3-month allergy shots, which you can find more info on here. Ultimately, understanding GAS helps us recognize how our bodies react to stressors, big or small, including those triggered by medical treatments like allergy shots.
It’s all connected!
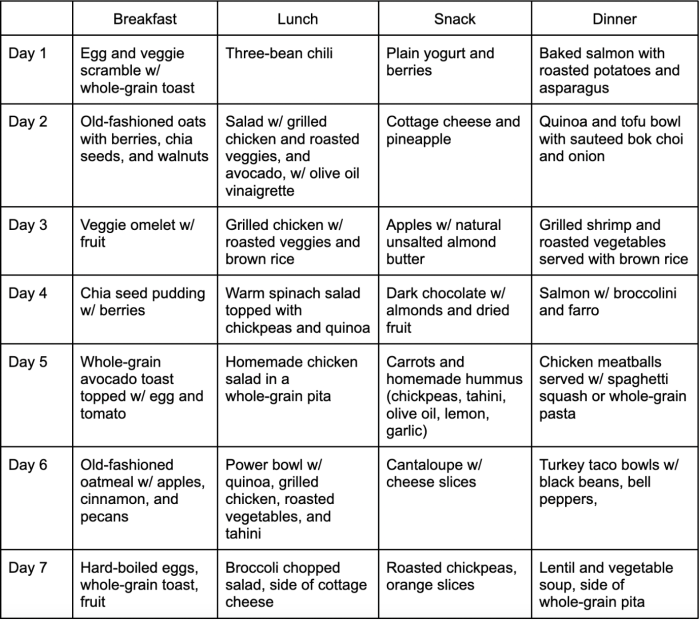
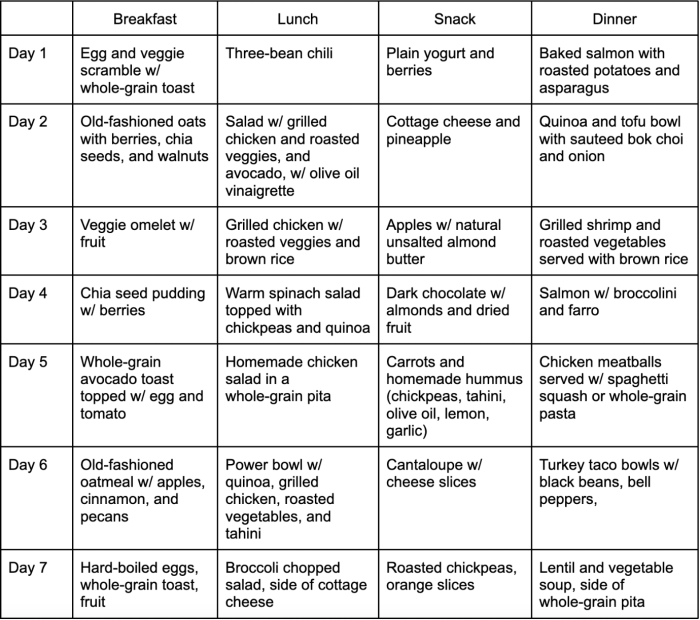
Lifestyle Modifications for Stress Management
Lifestyle modifications play a pivotal role in stress management and reducing the impact of GAS. Adopting healthy habits, such as regular exercise, balanced nutrition, and adequate sleep, can significantly influence the body’s ability to cope with stress. These modifications can contribute to overall well-being, creating a stronger foundation against stressors.
Stress Reduction Techniques
Effective stress-reduction techniques encompass a range of approaches targeting both the mind and body. These strategies are designed to calm the nervous system, promote relaxation, and build resilience to stress. Employing a combination of techniques can create a comprehensive strategy for managing stress.
- Mindfulness and Meditation: Mindfulness practices, including meditation, focus on present-moment awareness, reducing rumination on stressful thoughts and anxieties. Regular practice can cultivate a sense of calm and emotional regulation, enhancing resilience.
- Physical Activity: Engaging in regular physical activity, such as brisk walking, jogging, swimming, or yoga, can effectively reduce stress hormones like cortisol. Exercise releases endorphins, which have mood-boosting effects, and promotes relaxation.
- Progressive Muscle Relaxation: This technique involves systematically tensing and releasing different muscle groups in the body. This process promotes physical relaxation and reduces the physical manifestations of stress, such as muscle tension and headaches.
- Deep Breathing Exercises: Deep, slow breathing techniques, such as diaphragmatic breathing, can regulate the autonomic nervous system, promoting a sense of calm and reducing feelings of anxiety and panic. Controlled breathing can help in managing stress responses.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients to support the body’s ability to cope with stress. Nutrient deficiencies can exacerbate stress responses. Conversely, a healthy diet supports the body’s physiological functions, improving stress resilience.
- Time Management Techniques: Effective time management strategies can reduce feelings of overwhelm and control over time. Prioritization, scheduling, and delegation can help manage daily tasks, minimizing stressors related to time constraints and deadlines.
- Social Support: Maintaining strong social connections and seeking support from friends, family, or support groups can buffer the impact of stress. Sharing experiences and feelings can provide emotional support and reduce feelings of isolation.
Relaxation and Resilience Promotion
Promoting relaxation and resilience involves a multifaceted approach addressing both physical and psychological aspects. Techniques that enhance relaxation and promote resilience can help individuals navigate stressful situations more effectively.
- Establishing a Routine: A consistent daily routine, including sleep, meals, and work/study schedules, can provide a sense of structure and predictability, reducing uncertainty and associated stress.
- Setting Boundaries: Learning to set boundaries in relationships and commitments helps to manage expectations and avoid overcommitment, preventing burnout and associated stress.
- Positive Self-Talk: Replacing negative thoughts with positive affirmations can improve self-esteem and emotional regulation. Positive self-talk can contribute to stress resilience.
- Seeking Professional Help: If stress becomes overwhelming or persistent, seeking professional help from a therapist or counselor can provide personalized strategies and support in managing stress effectively.
Effective Stress-Reduction Techniques
These techniques can aid in managing stress, reducing the impact of GAS, and fostering resilience.
| Technique | Description |
|---|---|
| Mindfulness Meditation | Focusing on the present moment without judgment. |
| Progressive Muscle Relaxation | Systematically tensing and releasing muscle groups. |
| Deep Breathing Exercises | Regulating the autonomic nervous system through controlled breathing. |
| Yoga | Combining physical postures, breathing techniques, and meditation. |
| Physical Exercise | Engaging in activities like running, swimming, or dancing. |
Case Studies and Examples: General Adaptation Syndrome Overview
Understanding the General Adaptation Syndrome (GAS) is crucial for recognizing and managing stress-related issues. Real-world examples illustrate how GAS manifests in individuals, highlighting the importance of early intervention and effective coping mechanisms. These case studies reveal the physiological changes and behavioral responses associated with prolonged stress, showcasing the impact on overall well-being.
Hypothetical Case Study: Sarah’s Experience
Sarah, a 30-year-old project manager, experienced significant stress due to a demanding work environment and the recent loss of her grandmother. She had been working long hours, consistently missing deadlines, and struggling to maintain a healthy lifestyle. This intense pressure triggered a cascade of physiological changes, impacting her physical and mental health.
Physiological Changes Observed
Sarah exhibited a range of physiological responses associated with the alarm, resistance, and exhaustion stages of GAS. Initially, she experienced heightened anxiety, sleep disturbances, and a significant increase in heart rate and blood pressure. This initial alarm phase manifested as a heightened awareness of her surroundings, yet also leading to a decrease in appetite and fatigue. During the resistance stage, she developed coping mechanisms to deal with the stress, but her body struggled to fully recover, resulting in muscle tension, headaches, and gastrointestinal issues.
Prolonged stress, without effective coping, led to exhaustion, characterized by chronic fatigue, difficulty concentrating, and emotional instability. Her immune system weakened, increasing her susceptibility to infections.
Coping Mechanisms Employed, General adaptation syndrome overview
Initially, Sarah relied on avoidance and denial, avoiding social interaction and neglecting her personal needs. As the stress intensified, she began engaging in unhealthy coping mechanisms, such as overeating and excessive caffeine intake. However, she gradually recognized the need for healthier strategies. She sought support from her friends and family, practicing mindfulness exercises, and incorporating regular exercise into her routine.
Importance of Early Intervention
Early intervention is critical in managing stress-related issues. Addressing the root causes of stress and promoting healthy coping mechanisms can prevent the progression to more severe conditions. Recognizing the signs of stress and seeking support from professionals or support groups can significantly improve outcomes. If Sarah had sought help earlier, the severity of her symptoms might have been mitigated.
Treatment Strategies Used
Sarah sought help from a therapist who helped her develop coping mechanisms, identify the root causes of her stress, and manage her emotional responses. She also engaged in cognitive behavioral therapy (CBT) to modify negative thought patterns and develop more adaptive responses. The therapist also provided stress management techniques, including relaxation exercises and mindfulness practices. Her doctor also provided advice on dietary adjustments and exercise recommendations to improve her overall health.
Summary of Key Findings
| Category | Description |
|---|---|
| Triggering Factors | Demanding work environment, loss of grandmother |
| Physiological Responses | Elevated heart rate, blood pressure, anxiety, sleep disturbances, muscle tension, headaches, gastrointestinal issues, weakened immune system |
| Coping Mechanisms | Avoidance, denial, overeating, excessive caffeine intake, seeking support, mindfulness exercises, regular exercise |
| Treatment Strategies | Therapy (CBT), stress management techniques, relaxation exercises, mindfulness, dietary adjustments, exercise recommendations |
| Importance | Early intervention is crucial for preventing severe stress-related issues. |
Final Thoughts
In conclusion, general adaptation syndrome overview highlights the intricate connection between stress and our physical and mental health. By understanding the body’s response to stress, we can develop healthier coping strategies and interventions. The physiological mechanisms and the varied impact of stressors, coupled with the importance of social support and resilience, all contribute to a comprehensive understanding of this critical process.
Ultimately, this knowledge empowers us to better manage stress and maintain optimal well-being.