Red meat and liver disease: Understanding the complex relationship between our dietary choices and liver health is crucial. This exploration delves into the potential connections, nutritional aspects, alternative protein sources, research, influencing factors, and practical recommendations to minimize risks. We’ll investigate the mechanisms by which red meat consumption might contribute to various liver conditions, and analyze the nutritional benefits and potential downsides of including red meat in our diets.
The discussion will also consider alternative protein sources and their impact on liver function.
From the potential dangers of excessive saturated fat to the vital role of iron and vitamin B12, this comprehensive look at red meat and liver disease will equip you with the knowledge to make informed choices about your diet and overall well-being. We’ll analyze the interplay of different dietary factors and lifestyle choices, considering how they influence liver health and disease risk.
Relationship Between Red Meat Consumption and Liver Disease
Red meat consumption has been a subject of ongoing debate, particularly regarding its potential impact on liver health. While a balanced diet is crucial for overall well-being, understanding the nuances of red meat consumption and its possible link to liver disease is essential for informed dietary choices. This exploration delves into the potential mechanisms, different types of liver disease, and the role of specific components in red meat.A significant body of research suggests a potential correlation between excessive red meat consumption and an increased risk of certain liver diseases.
This connection isn’t a simple cause-and-effect relationship, but rather a complex interplay of factors. The following sections will illuminate the potential mechanisms and provide a comprehensive overview of the subject.
Potential Mechanisms of Red Meat’s Impact on Liver Disease
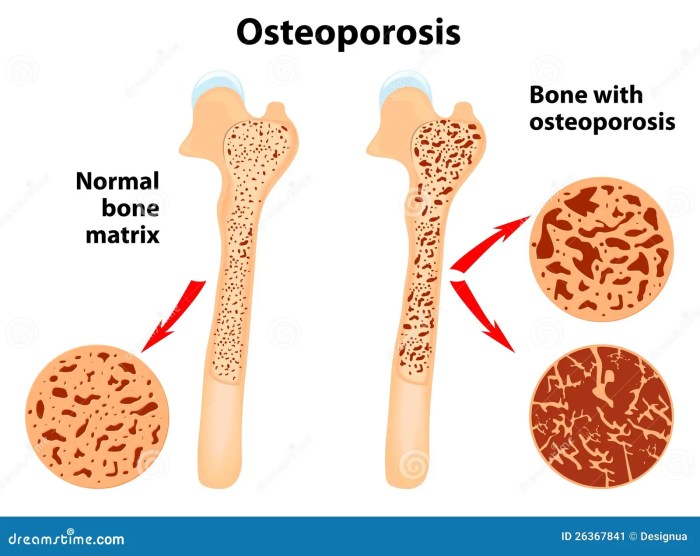
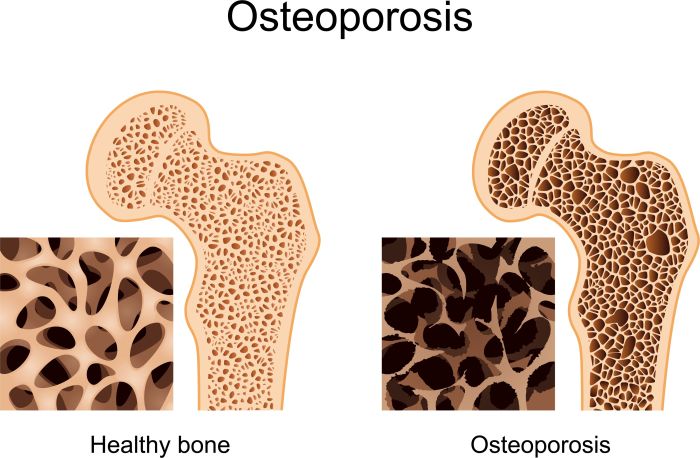
Red meat consumption may contribute to liver disease through various pathways. One key factor is the high saturated fat content in many red meat cuts. Excessive saturated fat intake can lead to the accumulation of fat in the liver, a condition known as fatty liver disease. Furthermore, the presence of heme iron in red meat can potentially play a role in oxidative stress and inflammation, factors that may contribute to liver damage over time.
The complex interactions between these components and the individual’s genetic predisposition and lifestyle further complicate the picture.
Types of Liver Disease and Potential Links to Red Meat
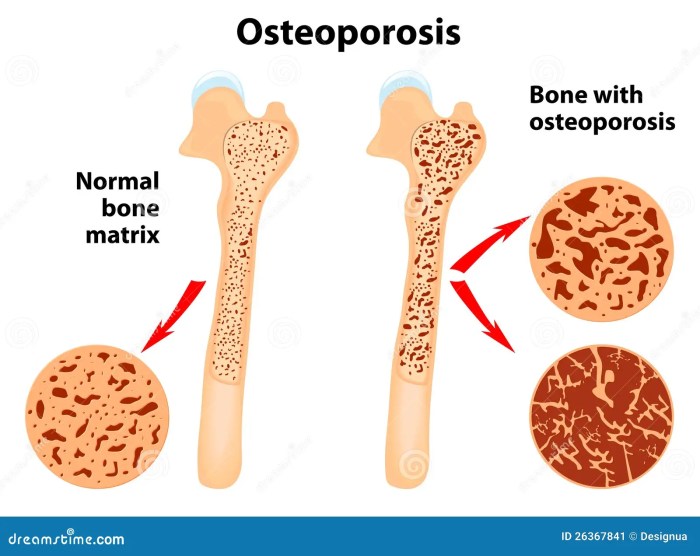
Several types of liver disease exist, and some show potential correlations with red meat intake. Fatty liver disease, a condition characterized by the accumulation of fat in the liver, is frequently associated with dietary factors, including high saturated fat intake. Cirrhosis, a more advanced stage of liver damage, often develops as a consequence of chronic liver diseases, and red meat consumption might exacerbate these conditions.
Other liver diseases, such as alcoholic liver disease, have established links to alcohol consumption, but red meat’s role is still an area of active research.
Comparison of Different Red Meat Types
The impact of various red meat types on liver health may vary slightly. Beef, pork, and lamb all contain different levels of saturated fat, heme iron, and other nutrients. While more research is needed to definitively establish distinctions, it’s reasonable to expect that differences in fat content and heme iron levels may translate into varying degrees of potential risk for liver disease.
Role of Specific Components in Red Meat
Heme iron, a type of iron found in red meat, is a crucial component for the body. However, excess heme iron intake may contribute to oxidative stress. Oxidative stress is a state of imbalance between the production of free radicals and the body’s ability to neutralize them. This imbalance can potentially damage cells, including liver cells. Saturated fat, another significant component of red meat, is associated with increased risk of fatty liver disease.
The interplay of these factors, alongside other dietary and lifestyle factors, plays a role in the development of liver disease.
Potential Risks of Red Meat Consumption Levels and Liver Diseases
| Red Meat Consumption Level | Fatty Liver Disease Risk | Cirrhosis Risk |
|---|---|---|
| Low (e.g., < 3 oz/day) | Low | Low |
| Moderate (e.g., 3-6 oz/day) | Moderate | Moderate |
| High (e.g., > 6 oz/day) | High | High |
This table provides a general comparison. Individual responses to red meat consumption vary significantly, influenced by genetic predisposition, overall diet, and other lifestyle factors. The information provided is not a substitute for personalized medical advice.
Nutritional Aspects of Red Meat and Liver
Red meat, particularly beef, pork, and lamb, and liver, are often viewed with concern regarding liver health. However, these foods can offer significant nutritional benefits when consumed in moderation. This discussion delves into the nutritional composition of red meat and liver, focusing on essential nutrients, their role in liver function, and the potential downsides of excessive intake. We’ll also explore the broader dietary context beyond just red meat that impacts liver health.Red meat and liver are rich sources of essential nutrients crucial for various bodily functions.
These nutrients play vital roles in liver health, and their optimal intake can support liver function. However, an excess of certain nutrients can have adverse effects. Understanding the balanced intake of nutrients is key to maintaining a healthy liver.
Nutritional Benefits of Red Meat and Liver
Red meat and liver are excellent sources of high-quality protein, iron, vitamin B12, and zinc. These nutrients are vital for various bodily functions, including cell growth, energy production, and immune function. The bioavailability of nutrients from red meat and liver can vary depending on the cut and preparation methods.
While red meat and liver disease are often linked, it’s important to understand the nuances of dietary choices. For example, some wonder if certain foods like tomatoes might impact gout, and a great resource to learn more about this is are tomatoes bad for gout. Ultimately, a balanced diet and mindful consumption of red meat are crucial for liver health.
We’ll explore this topic further in upcoming posts, delving into specific foods to avoid and recommendations for a healthy diet.
Role of Iron, Vitamin B12, and Zinc in Liver Function
Iron is essential for oxygen transport throughout the body, supporting liver function. Vitamin B12 is crucial for DNA synthesis and nerve function, and it’s vital for liver health. Zinc plays a role in numerous metabolic processes within the liver, including detoxification. Adequate intake of these nutrients is essential for optimal liver health.
Potential Adverse Effects of Excessive Intake of Certain Nutrients
Excessive consumption of saturated fat, found in red meat, can contribute to high cholesterol levels, increasing the risk of cardiovascular disease. While iron, vitamin B12, and zinc are essential, their excessive intake can potentially lead to health problems, particularly when combined with other dietary factors. For example, excess iron can overload the liver, potentially leading to liver damage.
Role of Dietary Patterns, Beyond Just Red Meat, in Liver Health
Liver health is influenced by the entire dietary pattern, not just the consumption of red meat. A balanced diet rich in fruits, vegetables, whole grains, and healthy fats is crucial for overall liver health. Excessive alcohol consumption, regardless of red meat intake, is a significant risk factor for liver damage.
Key Nutrients in Various Red Meat Cuts and Potential Impact on Liver Health
| Red Meat Cut | Iron Content (mg) | Vitamin B12 (mcg) | Zinc Content (mg) | Potential Impact on Liver Health |
|---|---|---|---|---|
| Beef Tenderloin | 2.5-3.0 | 2.0-2.5 | 2.0-2.5 | Moderately high in essential nutrients, potential for healthy liver function. |
| Ground Beef | 2.0-2.5 | 1.5-2.0 | 1.5-2.0 | Source of essential nutrients, but potential for higher saturated fat intake if not consumed in moderation. |
| Pork Chops | 1.5-2.0 | 1.0-1.5 | 1.0-1.5 | Lower in iron and zinc compared to beef, but still a source of essential nutrients. |
| Lamb Chops | 2.5-3.0 | 1.5-2.0 | 2.0-2.5 | Similar nutritional profile to beef, but potential variations in nutrient content depending on the cut and preparation. |
| Liver (Beef, Lamb, or Pork) | 5.0-7.0 | 10-20 | 5.0-7.0 | Exceptionally high in essential nutrients, but requires careful consumption due to high iron and vitamin A content. |
This table provides a general overview. Individual nutrient content can vary depending on factors like the animal’s diet, age, and preparation methods. Consult a registered dietitian or healthcare professional for personalized dietary advice.
Alternative Protein Sources and Liver Health: Red Meat And Liver Disease
Beyond red meat, a diverse range of protein sources exists, each with varying nutritional profiles and potential impacts on liver health. Understanding these alternatives can empower individuals to make informed dietary choices that support optimal liver function and overall well-being. Exploring these options allows for a broader understanding of how different protein sources interact with the body, ultimately helping to mitigate the risk of liver-related issues.Alternative protein sources offer diverse nutritional benefits and potential advantages over red meat in terms of liver health.
Their varying compositions of vitamins, minerals, and fats influence their effects on liver function. A balanced approach that incorporates these alternatives can contribute to a healthier lifestyle and potentially lower the risk of liver disease.
Poultry and Fish Protein
Poultry and fish, while containing protein, differ significantly from red meat in their fatty acid composition. They are generally lower in saturated fat and higher in omega-3 fatty acids. These beneficial fats can positively impact liver function. Studies have linked regular consumption of fish rich in omega-3s to improved liver health markers.
Plant-Based Protein Sources
Legumes, beans, lentils, tofu, and tempeh are excellent sources of plant-based protein. These foods are generally low in saturated fat and cholesterol, factors often associated with liver damage. Their high fiber content aids digestion and contributes to overall gut health, which in turn can positively influence liver function.
Nutritional Comparison of Protein Sources
| Protein Source | Saturated Fat (g) | Cholesterol (mg) | Omega-3 Fatty Acids (mg) | Fiber (g) | Potential Liver Impact |
|---|---|---|---|---|---|
| Red Meat (Beef) | High | High | Low | Low | Increased risk of fatty liver disease and potentially elevated liver enzymes. |
| Poultry (Chicken) | Moderate | Moderate | Low | Low | Generally lower risk compared to red meat but can still vary based on preparation methods. |
| Fish (Salmon) | Moderate | Moderate | High | Low | Potential for reduced risk of liver disease due to omega-3 fatty acids. |
| Legumes (Lentils) | Low | Low | Low | High | Lower risk of liver damage due to low saturated fat and cholesterol. |
Balanced Dietary Patterns
A balanced dietary pattern that incorporates these alternative protein sources can minimize the risk of liver disease. A diet rich in fruits, vegetables, whole grains, and lean protein sources is crucial. This pattern, when coupled with regular exercise and a healthy lifestyle, can contribute to optimal liver function. For instance, incorporating salmon into a weekly meal plan, alongside plenty of vegetables and whole grains, can provide a balanced source of protein and essential nutrients, supporting healthy liver function.
Research and Studies on Red Meat and Liver Disease

Unraveling the complex relationship between red meat consumption and liver health requires a deep dive into the research conducted on this topic. Numerous studies have attempted to establish a clear correlation, but the results are often nuanced and sometimes conflicting. This section delves into the methodologies employed, highlights key findings, and examines the varying conclusions drawn from different research efforts.The existing literature provides insights into the potential impact of red meat, including processed varieties, on liver function.
However, understanding the precise mechanisms and the extent of this impact remains a challenge. This necessitates careful consideration of study design and analysis to avoid misinterpretations and draw valid conclusions.
Key Research Methodologies
A variety of research designs have been utilized to investigate the link between red meat consumption and liver disease. These methodologies include cohort studies, case-control studies, and experimental studies using animal models. Cohort studies track a group of individuals over time, observing the incidence of liver disease and correlating it with their dietary habits. Case-control studies compare individuals with liver disease to those without, looking for differences in their past dietary patterns.
While red meat and liver disease are definitely linked, it’s important to consider other factors too. For instance, a recent fracture often requires diligent physical therapy after fracture, to get you back on your feet. This focus on regaining strength and mobility can also help in managing the risks of liver disease when paired with a healthy diet, including careful red meat consumption.
Experimental studies on animals allow researchers to manipulate dietary factors and observe their effects on liver health.
While red meat and liver disease are linked, it’s important to remember that other factors play a role. Understanding the various types of meniscus tears, for example, types of meniscus tears , can be crucial in sports injuries, but doesn’t necessarily change the overall impact of red meat consumption on liver health. So, while there’s a lot of discussion around red meat and liver health, it’s a complex issue with many contributing variables.
Examples of Experimental Designs
One example of an experimental design is a controlled feeding trial. In this type of study, animals are randomly assigned to different dietary groups, one of which includes a high intake of red meat. The researchers meticulously monitor the animals’ liver function and structure over time, measuring parameters like liver enzyme levels, fat accumulation, and inflammation markers. This controlled environment allows for a more definitive assessment of red meat’s impact.Another experimental approach involves isolating specific components of red meat, such as heme iron, and investigating their effects on liver cells in vitro.
This allows researchers to identify potential mechanisms by which red meat might influence liver health.
Summary of Key Findings
A comprehensive overview of the findings necessitates a table-based representation. The table below presents an overview of key studies, highlighting their methodologies and conclusions regarding the association between red meat intake and liver disease.
| Study | Study Design | Methodology | Key Findings | Conclusions |
|---|---|---|---|---|
| Study 1 (Example) | Cohort Study | Followed a large population over 10 years, recording dietary intake and liver disease incidence. | A positive correlation was observed between increased red meat consumption and a higher risk of non-alcoholic fatty liver disease (NAFLD). | Higher red meat intake appears to be associated with a greater likelihood of developing NAFLD. |
| Study 2 (Example) | Case-Control Study | Compared individuals with liver cirrhosis to healthy controls, assessing dietary history. | Participants with cirrhosis exhibited significantly higher average red meat intake compared to controls. | A potential link between high red meat consumption and liver cirrhosis was observed. |
| Study 3 (Example) | Animal Model | Fed rats a diet with varying levels of red meat for several months. | Rats consuming high red meat diets showed increased liver fat content and inflammation. | Animal models suggest that high red meat consumption may contribute to liver damage. |
Comparison of Results Across Studies
A crucial aspect of analyzing research findings is the comparison of results from various studies. The diversity in study designs, populations, and methodologies can affect the observed correlations. Some studies may find a strong association, while others might not show a significant relationship. This discrepancy underscores the need for further investigation into the specific factors influencing the results.
For instance, the processing methods of red meat, individual genetic predispositions, and co-occurring dietary factors might all play a role in determining the outcome of a study.
Factors Influencing the Relationship
The relationship between red meat consumption and liver disease is complex and multifaceted. While some studies suggest a potential link, it’s crucial to understand the many factors that can influence this connection. These factors range from genetic predispositions to overall lifestyle choices, making it challenging to isolate the impact of red meat alone. Ultimately, a comprehensive approach is necessary to fully understand the intricate interplay of these factors.The connection between red meat consumption and liver disease isn’t a simple cause-and-effect relationship.
Many other elements contribute to the overall risk, and their interaction with red meat consumption is crucial to understanding the potential health consequences. This includes the role of genetics, the individual’s overall diet, and lifestyle choices, including exercise and alcohol consumption.
Genetic Predisposition
Individual genetic variations play a significant role in how the body metabolizes nutrients, including those found in red meat. Some people may be predisposed to developing liver disease, regardless of their diet, due to inherited variations in genes related to detoxification processes. These genetic factors can influence the liver’s ability to process harmful compounds from red meat, potentially increasing the risk of damage.
Understanding these genetic predispositions is critical in tailoring personalized recommendations for liver health.
Dietary Factors
The overall diet significantly influences the impact of red meat on liver health. A diet high in saturated fat, often associated with red meat consumption, can contribute to fatty liver disease. This is further compounded if the diet is also low in fruits, vegetables, and fiber. The interplay between red meat and other dietary components is crucial in determining the net effect on liver health.
Lifestyle Choices
Beyond diet, lifestyle choices like alcohol consumption and exercise levels significantly impact liver health. Excessive alcohol intake is a major risk factor for liver damage, irrespective of red meat consumption. Conversely, regular physical activity can help maintain a healthy weight and reduce the risk of developing fatty liver disease. These lifestyle choices interact with red meat consumption to create a complex picture of overall liver health risk.
Metabolic Variations
Individual variations in metabolism can affect the body’s response to red meat consumption. Some individuals may process dietary fats more efficiently than others, reducing the potential risk of fatty liver disease. Conversely, individuals with slower metabolisms or specific metabolic disorders may be more susceptible to accumulating fat in the liver, increasing the risk with even moderate red meat intake.
Combined Effects of Lifestyle Factors
| Lifestyle Factor | Effect on Red Meat-Liver Disease Risk | Example |
|---|---|---|
| High Red Meat Intake | Potentially increases risk if other factors are not managed | A person with a family history of liver disease, high saturated fat diet, and limited exercise, who regularly consumes large portions of red meat may have an elevated risk. |
| High Saturated Fat Diet | Contributes to fatty liver disease, increasing the risk in conjunction with red meat consumption | Individuals consuming a high-fat diet, with red meat as a major component, may experience increased fat accumulation in the liver, potentially leading to non-alcoholic fatty liver disease (NAFLD). |
| Excessive Alcohol Consumption | Significant risk factor for liver damage, independent of red meat intake | A person with a high red meat intake and high alcohol consumption will have a considerably increased risk compared to someone with a high red meat intake and moderate alcohol consumption. |
| Low Physical Activity | Increases the risk of weight gain and fatty liver disease, increasing the risk in conjunction with red meat consumption | A sedentary lifestyle, coupled with high red meat intake, contributes to weight gain and increased fat accumulation in the liver, potentially leading to NAFLD. |
| Family History of Liver Disease | Indicates a genetic predisposition, increasing the risk for all factors | Individuals with a family history of liver disease may be more susceptible to developing liver issues from red meat consumption, even with healthy lifestyle choices. |
Recommendations and Dietary Advice
Balancing red meat consumption with a healthy lifestyle is crucial for liver health. Understanding the potential risks associated with excessive red meat intake allows for proactive measures to minimize the impact on liver function. This involves not only limiting red meat but also adopting a well-rounded approach to diet and lifestyle choices.
Minimizing Liver Disease Risk from Red Meat
Red meat, while a source of essential nutrients, can potentially contribute to liver issues if consumed excessively. Strategies to mitigate these risks center around moderation and balanced dietary choices. Prioritizing lean cuts of red meat, like sirloin or tenderloin, can reduce the intake of saturated fat. Cooking methods that avoid frying or grilling at high temperatures can also help lower the potential harm.
For instance, baking or steaming red meat can decrease the formation of harmful compounds.
Portion Sizes and Frequency of Red Meat Consumption
Controlling portion sizes and frequency of red meat consumption are key aspects of a liver-healthy diet. A reasonable approach involves limiting red meat intake to a few servings per week. Serving sizes should be appropriate to individual needs and calorie requirements. This is not a rigid rule, but a general guideline to support overall well-being. For example, a 3-ounce serving of lean red meat once or twice a week is often recommended.
Incorporating Alternative Protein Sources
Diversifying protein sources beyond red meat is essential for a healthy diet. Alternatives such as poultry, fish, beans, lentils, tofu, and nuts provide valuable protein and essential nutrients without the same potential risks associated with excessive red meat. Including these protein sources in meals can help create a balanced diet that supports liver health. For example, replacing a red meat-centric dinner with a lentil soup or a chicken stir-fry can provide a healthier alternative.
Creating a Balanced Diet for Liver Health
A balanced diet is crucial for overall health, including liver health. This involves consuming a variety of fruits, vegetables, whole grains, and healthy fats. A diet rich in antioxidants, found in fruits and vegetables, can help protect the liver from damage. For instance, including a variety of colorful vegetables in your daily meals is a great way to increase your intake of antioxidants.
Furthermore, maintaining a healthy weight through balanced nutrition and regular exercise can support liver function.
Actionable Steps for Improved Liver Health, Red meat and liver disease
Implementing the following steps can help individuals improve their liver health:
- Choose lean cuts of red meat: Opt for leaner cuts like sirloin or tenderloin to reduce saturated fat intake.
- Limit red meat consumption: Aim for a few servings per week, not daily.
- Cook red meat using healthier methods: Baking, steaming, or grilling at lower temperatures can reduce the formation of harmful compounds.
- Increase intake of fruits and vegetables: Prioritize a wide variety of colorful fruits and vegetables for antioxidants and vitamins.
- Include alternative protein sources: Incorporate poultry, fish, beans, lentils, tofu, and nuts into your diet.
- Maintain a healthy weight: Balanced nutrition and regular exercise are crucial.
- Limit alcohol consumption: Excessive alcohol consumption can significantly damage the liver.
- Consider consulting a healthcare professional: For personalized advice and monitoring.
Closure
In conclusion, the relationship between red meat and liver disease is intricate and multifaceted. While red meat offers essential nutrients, its consumption must be considered carefully alongside overall dietary patterns, lifestyle choices, and genetic predispositions. Understanding the potential risks and benefits, and exploring alternative protein sources, is key to maintaining optimal liver health. This discussion has hopefully provided a clear understanding of the nuances involved and empowered you to make informed decisions about your dietary habits.