Type 2 diabetes prognosis is a multifaceted topic, encompassing the outlook for individuals living with this chronic condition. This guide delves into the current understanding of long-term outcomes, exploring the interplay of lifestyle choices, medical treatments, monitoring strategies, and the impact of complications. We’ll examine the factors influencing the trajectory of the disease, from its typical progression to potential complications and how various interventions can affect the prognosis.
Understanding the different stages of type 2 diabetes and their associated prognoses is crucial. This will include a breakdown of lifestyle modifications, medical treatments, and management strategies, providing a holistic view of the possibilities available to those diagnosed. This exploration extends to the impact of complications on prognosis, along with future research and case studies to illustrate the variability in individual experiences.
Overview of Type 2 Diabetes Prognosis
Type 2 diabetes is a chronic condition that requires ongoing management. Understanding the prognosis, or expected course, of the disease is crucial for individuals and healthcare providers. This understanding allows for proactive strategies to minimize complications and improve quality of life. The prognosis is not a fixed outcome, but rather a spectrum influenced by various factors.The long-term outlook for individuals with type 2 diabetes is significantly impacted by factors like adherence to treatment plans, lifestyle choices, and early intervention.
Effective management strategies, including dietary changes, exercise, medication, and blood glucose monitoring, can significantly influence the course of the disease and prevent or delay complications.
Factors Influencing Long-Term Outlook
Several factors influence the long-term outlook for individuals with type 2 diabetes. These factors interact and can either improve or worsen the prognosis. Early diagnosis and prompt treatment play a critical role in preventing or delaying the development of complications.
- Age at Diagnosis: Individuals diagnosed with type 2 diabetes at a younger age may experience a more rapid progression of the disease compared to those diagnosed later in life. This is due to the longer duration of exposure to elevated blood glucose levels and the cumulative effect on organs.
- Pre-existing Conditions: Individuals with pre-existing conditions like high blood pressure, high cholesterol, or cardiovascular disease may experience a more accelerated progression of type 2 diabetes and its associated complications.
- Lifestyle Choices: A healthy lifestyle that includes a balanced diet, regular exercise, and stress management significantly improves the prognosis of type 2 diabetes. Conversely, unhealthy lifestyle choices can worsen the disease and increase the risk of complications.
- Adherence to Treatment Plan: Consistent adherence to prescribed medications, dietary recommendations, and exercise regimens is essential for effective management of type 2 diabetes and a positive prognosis. Consistency in blood glucose monitoring is also critical.
Typical Progression of Type 2 Diabetes
The progression of type 2 diabetes varies among individuals. Often, the disease starts with insulin resistance, where the body’s cells don’t respond properly to insulin. Over time, the pancreas may struggle to produce enough insulin to compensate for this resistance. This leads to elevated blood glucose levels.
- Early Stage: Characterized by insulin resistance, often asymptomatic or with mild symptoms. Regular checkups and lifestyle modifications are key to preventing progression.
- Intermediate Stage: Blood glucose levels gradually increase, and symptoms like increased thirst, frequent urination, and fatigue may become noticeable. Treatment with medication or lifestyle changes is crucial to control blood sugar and prevent further complications.
- Advanced Stage: Chronic hyperglycemia can lead to various complications, including nerve damage, kidney damage, cardiovascular disease, and eye damage. This stage requires intensive management with medications and lifestyle interventions.
Potential Complications
Several serious complications can arise from uncontrolled type 2 diabetes. These complications can significantly impact an individual’s quality of life and overall health. Early detection and management are critical to mitigating the risk and severity of these complications.
- Cardiovascular Disease: Elevated blood glucose levels contribute to the development of atherosclerosis, narrowing of the arteries, increasing the risk of heart attack and stroke. Individuals with type 2 diabetes often have an increased risk of these events.
- Neuropathy: Damage to the nerves can result in pain, numbness, tingling, and loss of sensation in the extremities. This can impact daily activities and require specialized care.
- Nephropathy: Damage to the kidneys can lead to kidney failure, requiring dialysis or kidney transplant. Close monitoring of kidney function is essential for individuals with type 2 diabetes.
Stages of Type 2 Diabetes and Prognosis
The following table Artikels different stages of type 2 diabetes and their associated prognoses. It is important to remember that this is a general overview, and individual outcomes can vary significantly.
| Stage | Description | Prognosis |
|---|---|---|
| Early Stage | Insulin resistance, mild symptoms | Favorable with lifestyle changes and early intervention |
| Intermediate Stage | Elevated blood glucose, noticeable symptoms | Favorable with medication and lifestyle changes, but risk of complications increases |
| Advanced Stage | Chronic hyperglycemia, significant complications | Requires intensive management, risk of severe complications and reduced life expectancy without aggressive intervention |
Impact of Lifestyle Modifications: Type 2 Diabetes Prognosis
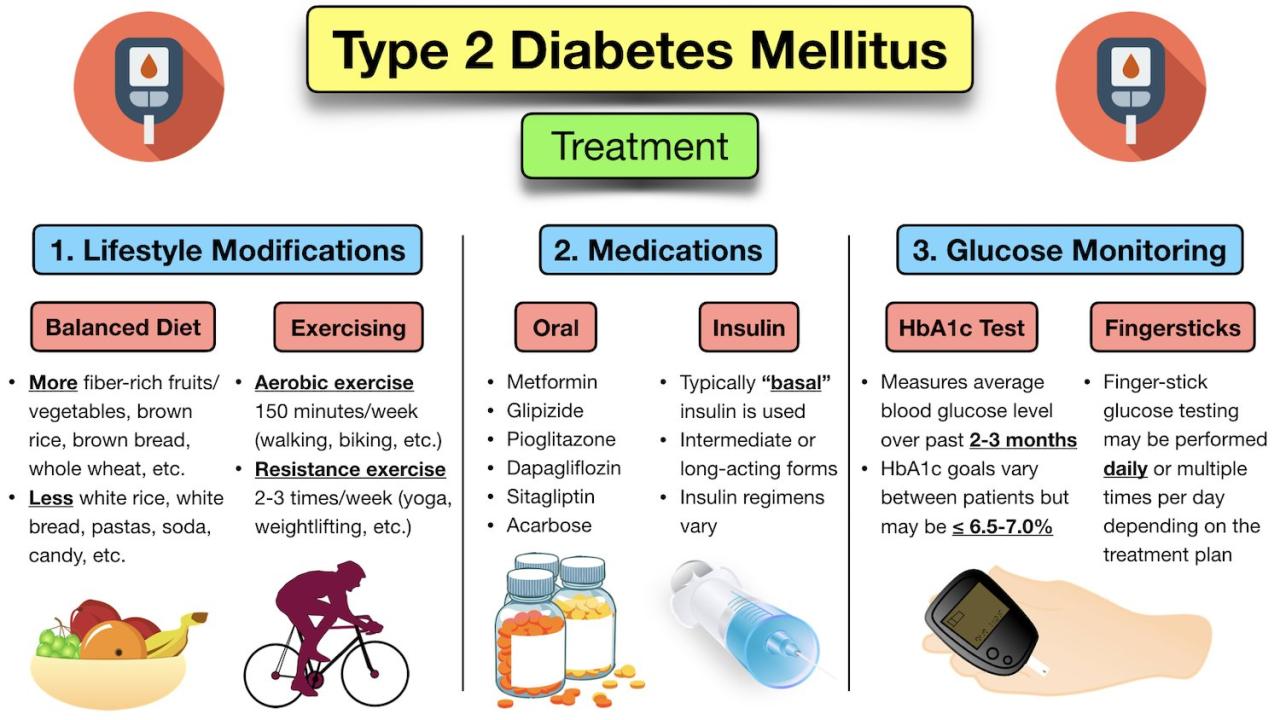
Type 2 diabetes, while a chronic condition, doesn’t have to dictate your life. Significant improvements in prognosis are often achievable through proactive lifestyle changes. Understanding how diet, exercise, and stress management influence the disease’s progression is key to taking control of your health. This empowers individuals to actively participate in their care and potentially mitigate the long-term complications associated with the disease.Lifestyle interventions are not just about symptom management; they can fundamentally alter the disease’s trajectory.
By addressing the root causes of insulin resistance and metabolic imbalances, individuals can often see a reduction in blood glucose levels, improved blood pressure and cholesterol, and a lessened risk of complications. This proactive approach to managing type 2 diabetes emphasizes the power of individual choices in positively impacting their health outcomes.
Dietary Approaches for Type 2 Diabetes Management
Dietary choices play a crucial role in managing blood sugar levels and overall health for individuals with type 2 diabetes. Various dietary approaches have shown promise in managing the condition. Understanding the effectiveness of different approaches allows individuals to tailor their diets to their specific needs and preferences.
- The Mediterranean Diet emphasizes fruits, vegetables, whole grains, legumes, and healthy fats like olive oil. This approach has been linked to improved glycemic control, reduced inflammation, and better cardiovascular health. Studies show that adherence to the Mediterranean diet can lead to significant improvements in blood glucose levels and reduced risk of cardiovascular complications.
- The DASH (Dietary Approaches to Stop Hypertension) diet focuses on reducing sodium intake and increasing fruits, vegetables, and low-fat dairy products. This diet is not only beneficial for blood pressure control but also demonstrates positive effects on blood sugar management and weight control. Many individuals find that incorporating DASH principles into their meals can lead to improved insulin sensitivity.
- Low-carbohydrate diets restrict carbohydrate intake, aiming to reduce blood glucose spikes. While effective for some, these diets may not be suitable for everyone. Individualized approaches are crucial for navigating the potential challenges and ensuring nutritional adequacy.
Impact of Exercise Regimens on Type 2 Diabetes Prognosis
Regular physical activity is essential for improving insulin sensitivity and managing blood glucose levels. Different exercise regimens can have varying effects on type 2 diabetes prognosis. Choosing the right exercise routine can be a powerful tool for managing the condition.
| Exercise Regimen | Impact on Type 2 Diabetes Prognosis | Example |
|---|---|---|
| Aerobic Exercise (e.g., brisk walking, jogging, swimming) | Improves insulin sensitivity, reduces blood glucose levels, and enhances cardiovascular health. | A 30-minute brisk walk most days of the week. |
| Resistance Training (e.g., weightlifting, bodyweight exercises) | Increases muscle mass, improves insulin sensitivity, and helps with weight management. | Two sessions per week of weightlifting targeting major muscle groups. |
| Combined Aerobic and Resistance Training | Offers the benefits of both types of exercise, leading to greater improvements in blood glucose control, weight management, and overall health. | A combination of brisk walking for 30 minutes and weightlifting for 30-45 minutes, 3 times per week. |
Role of Medical Treatments
Managing type 2 diabetes effectively hinges on a combination of lifestyle changes and medical interventions. While lifestyle modifications are crucial for achieving and maintaining optimal blood glucose control, medications play a vital role in achieving and maintaining target blood sugar levels, especially as the disease progresses. This section will explore the various medications used to treat type 2 diabetes, their mechanisms of action, and how they influence the prognosis of the disease.
Impact of Medications on Prognosis
Medications for type 2 diabetes aim to lower blood glucose levels, either by increasing insulin production, improving insulin sensitivity, or reducing glucose absorption. The effectiveness of these medications, and their impact on the overall prognosis, depends on individual factors like the severity of the disease, the presence of other health conditions, and patient adherence to the treatment plan. Successful management of type 2 diabetes through medication can significantly reduce the risk of developing serious complications such as heart disease, stroke, kidney disease, and nerve damage.
Mechanisms of Action of Different Medication Classes
Different classes of medications target different aspects of glucose metabolism. Oral hypoglycemics, such as metformin, sulfonylureas, and thiazolidinediones, work by increasing insulin sensitivity, stimulating insulin secretion, or inhibiting glucose production in the liver. Insulin therapy, on the other hand, directly replaces or supplements the body’s own insulin production.
- Metformin is generally the first-line medication for type 2 diabetes. It works by reducing glucose production in the liver and improving insulin sensitivity in the muscles and fat tissues. Studies have shown that metformin can significantly reduce the risk of cardiovascular events in patients with type 2 diabetes. A common example is a patient with a history of prediabetes who started metformin, resulting in sustained normal blood sugar levels and a significant reduction in the risk of developing type 2 diabetes.
- Sulfonylureas stimulate the pancreas to release more insulin. While effective in lowering blood glucose, their use may be associated with a higher risk of hypoglycemia (low blood sugar) compared to metformin. This is particularly important for patients with a history of hypoglycemic episodes.
- Thiazolidinediones improve insulin sensitivity in muscle and fat tissue. These medications have been linked to a potential increased risk of heart failure in some individuals. Patients with pre-existing heart conditions should be closely monitored when considering this class of medications.
- Insulin is used when other medications are not sufficient to control blood sugar levels. Various types of insulin are available, each with a different onset and duration of action. Insulin therapy is often necessary for patients with severe or rapidly progressing type 2 diabetes. An example would be a patient with uncontrolled blood sugar despite other medications, who transitioned to insulin therapy and saw a significant improvement in their A1C levels.
Comparative Analysis of Treatment Strategies
Different treatment strategies for type 2 diabetes may lead to varying prognoses. Combination therapy, which involves using two or more medications simultaneously, often yields better blood glucose control than monotherapy (using a single medication). This can be beneficial for patients who have difficulty achieving target blood sugar levels with a single medication. However, combination therapy may also increase the risk of side effects.
Individualized treatment plans are essential, taking into account factors such as patient preferences, cost considerations, and potential side effects. The selection of a particular medication or treatment strategy is ultimately a shared decision between the patient and their healthcare provider.
The prognosis for Type 2 diabetes can be significantly improved with lifestyle changes. A key part of that is focusing on a low-cholesterol diet, which includes choosing the right types of grains. For example, a diet rich in whole grains, rather than refined grains, can help manage blood sugar levels and overall health, as seen in resources like lowcholesterol diet which whole or refined grains.
Ultimately, a holistic approach, including dietary choices, can play a major role in positive outcomes for Type 2 diabetes.
Summary of Medications and their Effects, Type 2 diabetes prognosis
| Medication Class | Mechanism of Action | Benefits | Potential Side Effects |
|---|---|---|---|
| Metformin | Reduces glucose production, improves insulin sensitivity | Generally well-tolerated, low risk of hypoglycemia, may reduce cardiovascular risk | Gastrointestinal upset (e.g., diarrhea, nausea), vitamin B12 deficiency |
| Sulfonylureas | Stimulates insulin release | Effective in lowering blood glucose | Higher risk of hypoglycemia, weight gain |
| Thiazolidinediones | Improves insulin sensitivity | Effective in lowering blood glucose | Potential for heart failure, fluid retention, weight gain |
| Insulin | Replaces or supplements insulin production | Effective for severe or rapidly progressing type 2 diabetes | Risk of hypoglycemia, weight gain, potential for injection site reactions |
Monitoring and Management Strategies
Managing type 2 diabetes effectively hinges on consistent monitoring and proactive management strategies. Regular check-ups and meticulous tracking of blood glucose levels, along with other key vital signs, are crucial for identifying potential complications early on and adjusting treatment plans as needed. A personalized approach tailored to individual needs and lifestyle is essential for optimal outcomes.
The prognosis for type 2 diabetes can be significantly impacted by lifestyle choices and adherence to treatment plans. While managing this condition is a long-term commitment, proactive measures like diet and exercise are key. Interestingly, similar dedication to treatment, such as exploring options like treatment for metastatic castration resistant prostate cancer , demonstrates how crucial consistent care is across various health challenges.
Ultimately, a positive outlook and a personalized approach to care can lead to a better prognosis for type 2 diabetes.
Importance of Regular Monitoring
Regular monitoring of blood glucose levels is paramount in managing type 2 diabetes. This allows for early detection of fluctuations and adjustments to medication or lifestyle choices. Frequent monitoring also helps in identifying patterns and trends in blood sugar levels, enabling individuals to understand their responses to various factors like diet, exercise, and stress. This knowledge empowers patients to make informed decisions about their health and well-being.
Methods for Monitoring and Managing Type 2 Diabetes
Numerous methods are employed to monitor and manage type 2 diabetes. These range from self-monitoring of blood glucose (SMBG) using glucometers to continuous glucose monitoring (CGM) systems. Regular blood pressure and lipid checks are also essential components of comprehensive management. Dietary adjustments, exercise regimens, and adherence to prescribed medications are all integral parts of the management strategy.
Key Indicators Predicting Disease Progression
Several indicators can provide insights into the potential progression of type 2 diabetes. These include the HbA1c levels, which reflect average blood glucose control over several months. Elevated fasting blood glucose levels, inconsistent blood sugar control, and the presence of associated complications like neuropathy or nephropathy are all crucial indicators that warrant prompt attention. For example, a patient with consistently high HbA1c levels and elevated blood pressure may be at a higher risk of developing cardiovascular complications.
Patient Education and Self-Management
Patient education plays a vital role in improving the prognosis of type 2 diabetes. Empowering patients with knowledge about their condition, treatment options, and lifestyle modifications is essential. Self-management techniques, such as meal planning, regular exercise, and medication adherence, are crucial for achieving and maintaining good blood sugar control. Understanding the impact of various lifestyle factors on blood glucose levels allows patients to actively participate in their management.
This approach fosters a sense of ownership and accountability, leading to better outcomes.
Monitoring Tools and Accuracy
| Monitoring Tool | Accuracy in Assessing Prognosis | Description |
|---|---|---|
| Self-Monitoring of Blood Glucose (SMBG) | Moderate | Measures blood glucose levels at specific points in time. Results are immediate but may not reflect long-term trends. |
| Continuous Glucose Monitoring (CGM) | High | Provides a continuous record of glucose levels over time, offering insights into trends and patterns. This can be particularly useful in identifying episodes of hypoglycemia or hyperglycemia. |
| HbA1c Test | High | Measures average blood glucose levels over the past 2-3 months, providing a more comprehensive picture of long-term control. |
| Lipid Panel | Moderate | Evaluates cholesterol and triglyceride levels, crucial for assessing cardiovascular risk associated with diabetes. |
| Blood Pressure Monitoring | High | Regular blood pressure checks are essential for identifying and managing hypertension, a common complication of diabetes. |
Note: Accuracy levels are relative and may vary depending on individual factors and the specific monitoring device used. Consulting with a healthcare professional is crucial for interpreting results and developing a personalized management plan.
Impact of Complications on Prognosis
Type 2 diabetes, while manageable, can lead to serious complications that significantly impact a person’s overall health and prognosis. These complications often develop gradually, and their presence can dramatically alter the course of the disease, making long-term management more challenging and potentially shortening lifespan. Understanding the link between complications and prognosis is crucial for effective patient care and empowering individuals to make informed decisions about their health.
Cardiovascular Disease
Cardiovascular disease (CVD) is a major concern for individuals with type 2 diabetes. High blood sugar levels can damage blood vessels, increasing the risk of heart attack, stroke, and peripheral artery disease. The presence of CVD significantly reduces life expectancy and impacts the quality of life due to limitations in daily activities and increased risk of future health issues.
Early detection and management of CVD risk factors, such as high blood pressure, high cholesterol, and smoking, are vital for improving prognosis.
Nephropathy
Kidney disease, or nephropathy, is another serious complication of type 2 diabetes. Chronic high blood sugar damages the delicate filtering structures of the kidneys, leading to impaired function and potentially requiring dialysis or kidney transplantation. The severity of kidney damage directly correlates with the prognosis, with more advanced stages associated with a shorter lifespan and reduced quality of life.
Aggressive blood sugar control, blood pressure management, and careful monitoring of kidney function are essential for preventing and delaying the progression of nephropathy.
Type 2 diabetes prognosis can seem daunting, but consistent monitoring plays a crucial role. Understanding my blood sugar levels is key to managing the condition, and that’s why I test my blood sugar regularly. why i test my blood sugar helps me understand how my body reacts to different foods and activities. Ultimately, consistent monitoring and a proactive approach significantly improve my long-term type 2 diabetes prognosis.
Neuropathy
Neuropathy, characterized by nerve damage, is a common complication of type 2 diabetes. This damage can affect various parts of the body, leading to pain, numbness, tingling, and impaired motor function. The severity of neuropathy directly influences the prognosis. Severe cases can cause significant disability and reduce the ability to perform daily tasks. Maintaining optimal blood sugar control, adopting healthy lifestyle habits, and seeking prompt medical attention for any symptoms are crucial for managing and preventing neuropathy.
Correlation Between Complications and Reduced Life Expectancy
The following table demonstrates the approximate correlation between specific complications and reduced life expectancy in individuals with type 2 diabetes. It is important to note that these are estimates and individual outcomes vary significantly based on numerous factors including adherence to treatment plans, lifestyle choices, and overall health status.
| Specific Complications | Approximate Impact on Life Expectancy |
|---|---|
| Cardiovascular Disease (e.g., heart attack, stroke) | Significant reduction, often 5-10 years or more |
| Nephropathy (advanced kidney disease) | Significant reduction, often 5-15 years or more, depending on the stage |
| Neuropathy (severe cases) | Reduced quality of life, potential impact on lifespan (varies significantly) |
Future Research Directions
Understanding type 2 diabetes prognosis requires ongoing research to refine our knowledge and improve patient outcomes. The complexity of the disease, coupled with the evolving nature of lifestyle and treatment options, necessitates a proactive approach to future research. This involves exploring innovative strategies and leveraging advancements in technology to better predict, prevent, and manage this prevalent condition.
Unraveling the Genetic Predisposition
Genetic factors play a crucial role in the development and progression of type 2 diabetes. Further research into the specific genetic variations associated with varying responses to lifestyle modifications and treatments is essential. Identifying these genetic markers could allow for personalized risk assessments and targeted interventions, potentially preventing the onset of the disease or mitigating its progression. Studies focusing on gene-environment interactions are also important, as they can shed light on how environmental factors like diet and physical activity influence the expression of these genes.
This understanding will help develop more effective strategies for risk reduction and prevention.
Improving Predictive Modeling
Current models for predicting type 2 diabetes progression often have limitations. Research should focus on developing more sophisticated predictive models that incorporate a wider range of factors, including lifestyle choices, psychological well-being, and social determinants of health. For example, models that consider the interplay between genetics, lifestyle, and environmental factors could offer more accurate estimations of individual risk and progression.
This improved prediction capability would be invaluable in tailoring interventions to maximize their effectiveness and prevent long-term complications. A key component would be the incorporation of real-time data from wearable devices and other monitoring technologies to refine these models.
Leveraging Technological Advancements
Wearable devices, continuous glucose monitors, and artificial intelligence (AI) offer unprecedented opportunities for monitoring and managing type 2 diabetes. Research is needed to optimize the use of these technologies for continuous glucose monitoring, automated insulin delivery, and remote patient management. The development of AI algorithms capable of analyzing vast amounts of data from these devices could identify patterns indicative of impending complications or treatment inefficiencies, allowing for timely interventions.
This proactive approach to management has the potential to significantly improve outcomes. For example, a real-time monitoring system that alerts a patient to potential hyperglycemia issues could allow them to make immediate adjustments to their diet or insulin dose.
Longitudinal Studies for Long-Term Outcomes
Longitudinal studies are crucial for evaluating the long-term impact of different lifestyle interventions and treatment strategies on type 2 diabetes prognosis. These studies follow individuals over extended periods, allowing researchers to observe the cumulative effects of various factors and the development of complications. By tracking patients’ responses to treatments and lifestyle changes over time, researchers can identify patterns and trends, and gain a deeper understanding of how these factors influence long-term outcomes.
Such data is essential for creating evidence-based recommendations and refining clinical guidelines for the management of type 2 diabetes. Examples of this include studies that follow patients from diagnosis through the development of diabetic retinopathy or nephropathy. These longitudinal observations allow for a more comprehensive understanding of the disease progression.
Potential Future Studies
A potential future study could involve a randomized controlled trial comparing the efficacy of a novel combination therapy (e.g., a specific drug regimen combined with a tailored dietary intervention) versus standard care in preventing the development of microvascular complications in patients with early-stage type 2 diabetes. Another study might focus on utilizing AI algorithms to analyze patient-reported outcomes (PROs) from wearable devices to identify early warning signs of treatment failure and adjust management strategies proactively.
These are just a few examples of the many possibilities for future research that hold the promise of significant advancements in understanding and managing type 2 diabetes.
Illustrative Case Studies
Understanding type 2 diabetes is not just about statistics; it’s about the real-life experiences of individuals. This section delves into specific case studies to highlight the variability in responses to the disease, demonstrating how lifestyle choices, treatment approaches, and complications intertwine to shape the prognosis. These narratives provide a human face to the often-complex landscape of managing type 2 diabetes.Case studies offer valuable insights into the diverse ways individuals navigate the challenges of type 2 diabetes.
Each case reveals how a combination of factors—from dietary habits and exercise routines to the effectiveness of medication and the presence of potential complications—influence the overall health trajectory. By examining these individual stories, we gain a richer appreciation for the personalized nature of managing this chronic condition.
Case Study 1: Emphasis on Lifestyle Modifications
Sarah, a 45-year-old woman with a family history of type 2 diabetes, was diagnosed at age 42. Initially, her blood sugar levels were moderately elevated. She embraced a comprehensive lifestyle intervention program that included a balanced Mediterranean diet rich in fruits, vegetables, and whole grains, coupled with regular exercise, including brisk walking for 30 minutes most days of the week.
Her weight gradually decreased, and her blood glucose levels normalized. Regular check-ups and adherence to the prescribed lifestyle plan became integral to her long-term management. This demonstrates that early intervention and consistent lifestyle changes can significantly improve the prognosis for type 2 diabetes.
Case Study 2: Impact of Delayed Diagnosis and Treatment
John, a 60-year-old man with a sedentary lifestyle and a history of high blood pressure, experienced symptoms like increased thirst and frequent urination for several months before seeking medical attention. His diagnosis was delayed, resulting in elevated blood sugar levels. Initial treatment focused on medication, but John struggled with adherence. Eventually, he developed diabetic neuropathy, leading to pain and numbness in his feet.
His blood glucose control remained challenging, and he experienced recurrent episodes of hyperglycemia. This case illustrates how delayed diagnosis and treatment can negatively affect the prognosis by increasing the risk of developing severe complications.
Case Study 3: Effective Management with Comprehensive Care
Maria, a 55-year-old woman with type 2 diabetes, consistently engaged in self-management practices. Her treatment plan incorporated medication, regular monitoring of blood sugar levels, a healthy diet, and consistent exercise. She actively participated in diabetes support groups and educated herself about the condition. She also prioritized stress management techniques. As a result, Maria maintained excellent blood glucose control and avoided significant complications.
This case underscores the crucial role of patient engagement, active participation in treatment, and a comprehensive approach to diabetes management.
Summary of Case Studies
| Case Study | Key Factors Affecting Prognosis | Outcome | Key Takeaway |
|---|---|---|---|
| Case Study 1 | Early diagnosis, consistent lifestyle modifications (diet and exercise) | Normalized blood glucose levels, improved overall health | Lifestyle changes can significantly improve outcomes in early stages. |
| Case Study 2 | Delayed diagnosis, inconsistent treatment adherence, development of neuropathy | Elevated blood sugar levels, development of complications (neuropathy) | Early diagnosis and consistent treatment are crucial to avoid long-term complications. |
| Case Study 3 | Consistent self-management (medication, diet, exercise, support groups), proactive engagement in care | Excellent blood glucose control, avoidance of significant complications | Patient engagement and a comprehensive approach to management are vital for optimal outcomes. |
Summary
In conclusion, type 2 diabetes prognosis is a complex equation influenced by a multitude of factors. While the disease can significantly impact an individual’s life, proactive lifestyle choices, appropriate medical interventions, and vigilant monitoring can significantly improve outcomes. The variability in individual responses highlights the importance of personalized approaches to care. Future research and innovative technologies hold the promise of further advancements in understanding and managing this condition, ultimately leading to improved prognoses for those affected.

