Definition of progressive disease sets the stage for this enthralling narrative, offering readers a glimpse into the complex world of illnesses that gradually worsen over time. We’ll explore the defining characteristics, the factors influencing progression, the diagnostic processes, and the profound impact on patients and families. This journey will cover everything from the initial diagnosis to treatment strategies and the latest research.
Understanding the various stages of progression, the different types of progressive diseases, and the factors that influence their development is crucial. We will delve into the genetic, environmental, and lifestyle aspects that play a role. Furthermore, we will examine how medical interventions can potentially slow or halt the disease’s advance.
Defining Progressive Disease
Progressive diseases are a significant health concern, characterized by a gradual and often irreversible decline in the body’s function over time. Understanding their nature, progression, and diverse manifestations is crucial for effective diagnosis, treatment, and patient care. They contrast sharply with acute illnesses, which tend to have a rapid onset and resolution.Progressive diseases are distinguished by a consistent deterioration in health status, which can manifest in various ways depending on the specific condition.
This deterioration can involve physical, cognitive, or emotional capabilities. The underlying mechanisms of these diseases can be complex and often involve damage to cells, tissues, or organs.
Key Characteristics of Progressive Diseases
Progressive diseases are characterized by a steady decline in function. This decline is typically continuous, although the rate of decline may vary. Crucially, progressive diseases differ from acute conditions in their long-term nature and the persistent and ongoing impact on the individual. A crucial factor is that the disease’s progression is not typically reversed or cured through standard treatments, though the disease’s progression can sometimes be slowed.
Disease Progression in Progressive Diseases
Disease progression in progressive diseases is not linear; it can fluctuate in severity and rate. Factors such as genetics, environmental triggers, and the individual’s overall health can influence how the disease manifests and evolves over time. This concept of variable progression is critical for patient management and understanding the experience of those affected. While there is no uniform rate of progression, a clear pattern is observed in most cases, with stages of worsening symptoms.
Types of Progressive Diseases
Progressive diseases encompass a broad spectrum of conditions, each with its unique characteristics and patterns of progression. Neurodegenerative diseases, like Alzheimer’s and Parkinson’s, involve the gradual loss of nerve cells, leading to cognitive and motor impairments. Cardiovascular diseases, such as atherosclerosis, demonstrate a progressive buildup of plaque in blood vessels, increasing the risk of heart attacks and strokes.
Genetic disorders, like cystic fibrosis and Huntington’s disease, are often progressive, affecting multiple organs and systems throughout life. Autoimmune diseases, such as multiple sclerosis, also fall into this category.
Progressive diseases, like many conditions, often show up subtly at first. Understanding the progression is key, and sometimes, a simple urinalysis can be a crucial indicator of underlying issues. Checking your urinalysis results can give you a better insight into what’s happening within your body, helping you understand how a condition might be evolving. For a detailed explanation of what your urinalysis results might mean, check out this resource from Valley Ridge Health: what do your urinalysis results mean.
Ultimately, a better understanding of these results, and of the definition of progressive diseases, can help you make more informed decisions about your health.
Stages of Progression
Progressive diseases often progress through distinct stages, each marked by a worsening of symptoms and functional decline. A clear understanding of these stages is essential for monitoring disease progression and tailoring treatment strategies.
- Early Stage: Initial symptoms are subtle and may be easily missed or attributed to other causes. For example, in Alzheimer’s disease, early symptoms may include forgetfulness or difficulty with planning. Early detection is often crucial to slowing the rate of progression.
- Middle Stage: Symptoms become more pronounced and noticeable, impacting daily life. In Parkinson’s disease, this stage might include tremors, rigidity, and difficulty with movement. This stage is when support systems become vital for managing the condition.
- Late Stage: Symptoms reach their most severe form, significantly impairing the individual’s ability to function independently. At this stage, in conditions like amyotrophic lateral sclerosis (ALS), individuals may require extensive assistance for basic activities of daily living.
Illustrative Example: Alzheimer’s Disease
Alzheimer’s disease is a progressive neurodegenerative disorder. Its progression often follows a pattern of gradual cognitive decline. The early stage might involve mild memory loss and difficulty with planning. The middle stage involves greater challenges with daily tasks and communication. The late stage can result in severe memory loss, loss of communication skills, and significant dependence on others.
This example underscores the importance of early detection and ongoing support in managing progressive diseases.
Factors Influencing Progression
Progressive diseases, characterized by a gradual decline in function and increasing severity over time, are influenced by a complex interplay of factors. Understanding these influences is crucial for developing effective strategies to manage and potentially slow the progression of these conditions. This exploration delves into the genetic, environmental, lifestyle, and medical intervention factors that contribute to the trajectory of a progressive disease.Genetic predisposition, environmental triggers, and lifestyle choices all contribute to the progression of a progressive disease.
Medical interventions can play a crucial role in slowing or halting progression, though their effectiveness varies significantly based on the specific disease and the individual patient.
Genetic Predisposition
Genetic factors significantly contribute to an individual’s susceptibility to and the rate of progression of a progressive disease. Inherited variations in genes can alter an individual’s response to environmental triggers and their ability to repair cellular damage. For example, mutations in genes involved in DNA repair pathways can increase the risk of developing neurodegenerative diseases. Studies have shown that family history of a particular disease often correlates with a higher likelihood of developing that disease.
These genetic predispositions, however, do not always guarantee disease onset, highlighting the complex interaction between genes and the environment.
Environmental Influences, Definition of progressive disease
Environmental factors play a critical role in the progression of various progressive diseases. Exposure to toxins, pollutants, or infections can contribute to cellular damage and accelerate the progression of disease. For instance, exposure to certain pesticides or heavy metals has been linked to an increased risk of neurodegenerative disorders. Nutritional deficiencies or exposure to infectious agents can also impact the progression of a progressive disease.
Environmental factors can exacerbate genetic predispositions, creating a more potent effect on disease development.
Lifestyle Choices
Lifestyle choices can have a substantial impact on the progression of a progressive disease. Maintaining a healthy diet, engaging in regular physical activity, and avoiding smoking and excessive alcohol consumption can all contribute to a slower progression and overall better health. For instance, a diet rich in antioxidants and anti-inflammatory compounds may help mitigate cellular damage, potentially slowing the progression of certain neurodegenerative diseases.
Conversely, unhealthy habits can exacerbate the effects of genetic predispositions and environmental factors.
Medical Interventions
Medical interventions play a vital role in managing and potentially slowing or halting the progression of progressive diseases. These interventions may include medications, therapies, or surgical procedures designed to address specific symptoms, slow disease progression, or improve quality of life. The effectiveness of these interventions varies greatly depending on the specific disease, the stage of the disease, and the individual patient’s response.
For example, disease-modifying therapies for multiple sclerosis aim to slow the progression of the disease by reducing inflammation and preventing further damage to the nervous system.
Diagnosis and Monitoring
Progressive diseases, by their very nature, often present with subtle and gradual changes. Accurate diagnosis and consistent monitoring are crucial for managing these conditions effectively. Early detection allows for timely interventions, potentially slowing disease progression and improving quality of life. This involves a multifaceted approach, considering various factors and employing a range of diagnostic tools.
Diagnostic Process for Progressive Diseases
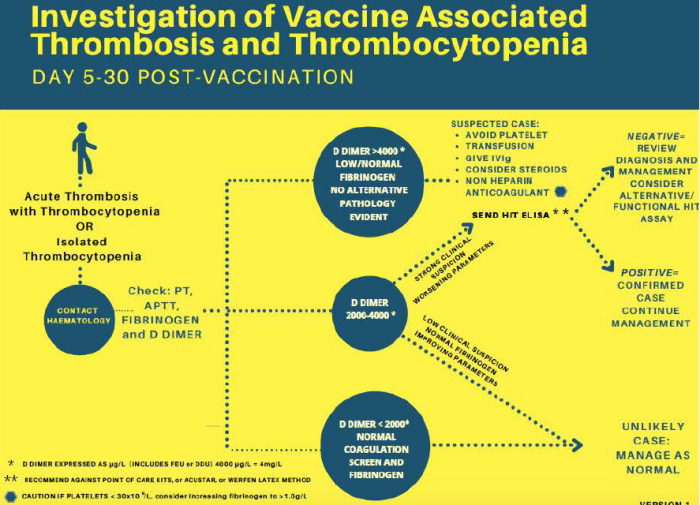
Diagnosing progressive diseases requires a thorough understanding of the patient’s medical history, including family history of similar conditions, and a detailed physical examination. Subsequent investigations are tailored to the suspected disease category. This may include blood tests, imaging studies, genetic testing, and biopsies, all carefully considered and performed in a stepwise manner. The diagnostic process frequently involves collaboration among specialists, such as neurologists, cardiologists, and oncologists, to achieve a comprehensive and accurate assessment.
Methods Used to Monitor Disease Progression
Monitoring disease progression is essential for tailoring treatment plans and evaluating response to interventions. Various methods are employed, each offering valuable insights into the trajectory of the disease. These methods often involve repeated assessments of specific symptoms, functional abilities, and physiological markers.
Diagnostic Tools and Procedures
A range of diagnostic tools and procedures are employed in the assessment and monitoring of progressive diseases. These include:
- Neurological Examinations: These assessments evaluate cognitive function, motor skills, reflexes, and sensory perception. Variations in these functions can indicate disease progression or response to treatment. For example, regular assessments of gait and balance in patients with Parkinson’s disease can help track motor deterioration.
- Imaging Techniques: Techniques like MRI (Magnetic Resonance Imaging), CT (Computed Tomography), and PET (Positron Emission Tomography) provide detailed anatomical and functional information. Changes in brain structure or activity over time can be crucial in evaluating neurodegenerative diseases. For instance, MRI scans can reveal the progression of amyloid plaques in Alzheimer’s disease.
- Biochemical Tests: Blood tests and other biochemical analyses can detect specific biomarkers indicative of disease progression or response to treatment. These tests are particularly important in conditions like cardiovascular disease, where elevated cholesterol or inflammatory markers can signal worsening conditions. Examples include measuring C-reactive protein (CRP) levels for inflammation in various conditions.
- Genetic Testing: In some progressive diseases, genetic predisposition plays a significant role. Genetic testing can identify specific gene mutations that contribute to disease development and progression. This is crucial for early detection and personalized risk assessment.
Common Diagnostic Criteria for Different Progressive Diseases
The diagnostic criteria for various progressive diseases are often based on a combination of factors. This includes specific symptoms, physical findings, and laboratory results. A precise diagnosis is critical to initiate the most appropriate and effective treatment strategy.
Impact on Patients and Families
Progressive diseases, by their very nature, profoundly impact not only the individuals diagnosed but also their families. The relentless progression, often unpredictable course, and the varying degrees of physical, emotional, and social challenges can create a complex and demanding environment. Understanding these impacts is crucial for developing effective support systems and strategies for coping.The physical, emotional, and social toll of progressive diseases can vary significantly depending on the specific condition, its rate of progression, and the individual’s resilience.
The challenges extend far beyond the patient to encompass the entire family unit. Caregivers often face immense strain, juggling their own lives and responsibilities with the demands of providing care.
Physical Impact on Patients
Progressive diseases frequently cause debilitating physical symptoms. These can range from muscle weakness and pain to loss of mobility and sensory function. The increasing dependence on others for daily activities can be profoundly distressing, affecting the patient’s sense of autonomy and dignity. For example, individuals with multiple sclerosis (MS) might experience significant difficulties with walking, balance, and fine motor skills, impacting their ability to perform basic tasks like dressing and eating.
The progression of these symptoms can lead to isolation and a decline in overall well-being.
Emotional Impact on Patients
The emotional toll of progressive diseases is often underestimated. Patients frequently experience anxiety, depression, fear, and grief as they grapple with the anticipated loss of independence, the potential for future complications, and the uncertainty of the disease’s trajectory. Coping with the gradual decline in physical abilities can lead to feelings of helplessness and frustration. The experience can significantly affect the patient’s self-esteem and overall emotional well-being.
Social Impact on Patients and Families
Progressive diseases can also have a significant social impact. Patients may experience social isolation due to limitations in mobility and participation in social activities. The need for ongoing medical care and treatments can also place a strain on social relationships and daily routines. Families may also experience social isolation as they navigate the demands of caregiving.
Challenges Faced by Families
Caring for individuals with progressive diseases presents numerous challenges for families. The demands of providing care, including assistance with daily living activities, medical appointments, and emotional support, can significantly impact family dynamics and resources. Financial strain is a common concern, as medical costs, home modifications, and lost income can accumulate rapidly. The emotional burden on caregivers, including feelings of stress, anxiety, and guilt, can also be substantial.
The long-term nature of the condition can lead to burnout and strained relationships.
A progressive disease, essentially, is one that gets worse over time. Think of it like a slow-burn fire; the damage escalates gradually. A prime example of this is congenital adrenal hyperplasia, a condition where the adrenal glands don’t produce enough hormones. Learning more about this fascinating and complex condition can be incredibly insightful, and you can find a detailed overview here.
Ultimately, understanding the progression of these types of conditions is crucial for developing effective treatment strategies.
Support Systems for Patients and Families
Numerous support systems are available to assist patients and families coping with progressive diseases. These include:
- Support Groups: These groups provide a safe space for sharing experiences, offering emotional support, and learning from others facing similar challenges. Support groups can offer a sense of community and reduce feelings of isolation.
- Professional Counseling: Counseling can help patients and families cope with the emotional and psychological challenges associated with progressive diseases. This can include individual, couples, or family therapy.
- Caregiver Resources: Caregiver support programs can provide practical assistance, education, and respite care to alleviate the burden on caregivers.
- Financial Assistance Programs: Various organizations offer financial assistance to help cover medical expenses and other related costs.
Impact on Quality of Life
Progressive diseases can significantly impact the quality of life for patients and their families. The physical limitations, emotional distress, and social challenges can lead to a decline in overall well-being. Maintaining a positive outlook and adapting to the changing circumstances are crucial for maintaining a good quality of life. For example, adapting daily routines to accommodate physical limitations and fostering social connections can help patients and families maintain a fulfilling life.
Importance of Patient Advocacy
Patient advocacy plays a crucial role in managing progressive diseases. Advocates can raise awareness, advocate for better access to resources, and improve the quality of care for those affected. Patient advocacy can help ensure that patients’ voices are heard and their needs are addressed. Active participation in support groups and advocating for policies that improve access to care can empower individuals and families.
Treatment Strategies

Navigating the complexities of progressive diseases requires a multifaceted approach that extends beyond symptom management. Effective treatment strategies aim to slow disease progression, mitigate its impact, and enhance the quality of life for individuals and their families. This involves a careful consideration of various treatment options, personalized to each patient’s unique needs and the specific disease.A holistic framework for managing progressive diseases emphasizes a combination of medical interventions, supportive care, and lifestyle adjustments.
This strategy prioritizes proactive management, early intervention, and ongoing monitoring to optimize outcomes and minimize the burden of the disease. The success of treatment hinges on a strong partnership between healthcare providers, patients, and their families, ensuring that the treatment plan aligns with individual goals and values.
Framework for Managing Progressive Diseases
A comprehensive framework for managing progressive diseases typically involves several key elements. These include accurate diagnosis, a clear understanding of the disease trajectory, and a personalized treatment plan tailored to the patient’s specific needs. This framework also considers the patient’s physical, emotional, and social well-being. Proactive monitoring, adjustments to the treatment plan as the disease progresses, and access to support groups are crucial components of this framework.
Treatment Strategies for Slowing Disease Progression
Various treatment strategies are employed to slow or manage disease progression, depending on the specific condition. These approaches range from medications targeting disease mechanisms to therapies aimed at mitigating symptoms and preserving function. Some strategies focus on slowing the rate of damage to affected organs, while others aim to enhance the body’s natural defenses.
Progressive diseases, like many health conditions, gradually worsen over time. Understanding how much creatine you need daily can be important for overall health, and how it might impact a person’s ability to manage a progressive disease is something to consider. Finding the right dosage of creatine, as detailed in this guide on how much creatine per day , is key to managing any health concerns.
This ultimately helps in understanding how best to treat and manage a progressive disease.
Examples of Supportive Care Options
Supportive care is integral to the management of progressive diseases, offering crucial assistance to patients and their families. These options address the physical, emotional, and social needs that arise alongside the disease. Examples include physical therapy to maintain mobility, occupational therapy to adapt daily living, and nutritional counseling to optimize nutrition. Furthermore, counseling services can address emotional challenges and provide support to both the patient and their caregivers.
Social work interventions facilitate access to resources and support systems, while palliative care focuses on symptom management and improving quality of life.
Comparison of Treatment Approaches
Treatment approaches for progressive diseases vary considerably based on the specific condition. For example, treatments for neurodegenerative diseases often focus on slowing the progression of neuronal damage, while those for chronic respiratory conditions prioritize symptom management and improving lung function. The selection of a treatment strategy requires careful consideration of the disease’s unique characteristics and the patient’s individual needs.
A comparative analysis of these approaches should be made in the context of each specific disease, considering factors such as disease progression rate, symptom severity, and patient preferences.
Potential Benefits and Limitations of Treatment Approaches
Each treatment approach has its own set of potential benefits and limitations. For instance, medications aimed at slowing disease progression may show promising results in clinical trials but may have significant side effects or only produce modest improvements. Supportive care, while not directly targeting disease mechanisms, plays a vital role in improving the patient’s quality of life and minimizing the impact of the disease.
The limitations of these approaches must be carefully considered in conjunction with the potential benefits, especially when considering the long-term implications of a particular treatment plan.
Illustrative Examples: Definition Of Progressive Disease
Progressive diseases, encompassing a wide spectrum of conditions, affect individuals across various life stages and impact diverse bodily systems. Understanding these diseases through real-world examples provides crucial insights into their complexities and the challenges faced by those living with them. Examples of progressive diseases, detailed case studies, and a look at the long-term outlook offer valuable perspectives.
Examples Categorized by Body System
Progressive diseases can affect various systems within the human body. Here are examples across several systems:
- Neurological System: Conditions like Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis progressively impair cognitive function, motor skills, and sensory perception. These conditions can lead to significant challenges in daily life and require comprehensive management.
- Musculoskeletal System: Osteoarthritis and rheumatoid arthritis are examples of progressive diseases that affect joints, causing pain, stiffness, and reduced mobility. These conditions often lead to chronic pain and functional limitations.
- Cardiovascular System: Heart failure, a progressive condition, results in the heart’s inability to pump blood effectively. Over time, this leads to a decline in the heart’s capacity and can result in significant health risks.
- Respiratory System: Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by airflow obstruction. This can lead to shortness of breath and a decline in lung function over time, requiring ongoing medical management.
- Renal System: Chronic kidney disease (CKD) is a progressive condition where the kidneys gradually lose their ability to filter waste products from the blood. This can lead to a buildup of toxins and other health complications.
Detailed Information on Alzheimer’s Disease
Alzheimer’s disease is a progressive neurodegenerative disorder characterized by a gradual decline in cognitive function.
Symptoms: Early symptoms often include subtle memory loss, difficulty with language, and impaired judgment. As the disease progresses, symptoms intensify, leading to severe memory loss, disorientation, and behavioral changes. Individuals may experience challenges with daily tasks, including dressing, eating, and personal hygiene.
Progression: Alzheimer’s disease typically progresses over several years, with varying rates of decline among individuals. The progression can be categorized into different stages, each marked by escalating cognitive and functional impairments. The initial stages often involve mild memory problems, while later stages lead to complete dependence on others for care.
Treatment Options: Currently, there is no cure for Alzheimer’s disease. Treatment focuses on managing symptoms and slowing the progression of the disease. Medications may help to improve cognitive function and manage behavioral symptoms. Therapies, such as cognitive stimulation programs and support groups, can also play a crucial role in improving quality of life for individuals with Alzheimer’s disease and their families.
Case Study of a Patient with Parkinson’s Disease
A 62-year-old man, Mr. Smith, was diagnosed with Parkinson’s disease at age 55. His initial symptoms included mild tremors in his left hand and slight stiffness in his posture. Over the following years, the tremors worsened, affecting both hands and progressing to involve his legs. He also experienced slowness of movement (bradykinesia) and rigidity in his limbs.
Medication helped manage his symptoms initially, allowing him to maintain some independence. However, as the disease progressed, he required more frequent medication adjustments and eventually assistance with daily activities. He participated in physical therapy to maintain mobility and balance, and support groups to cope with the emotional and social challenges.
Long-Term Outlook for Progressive Diseases
The long-term outlook for progressive diseases varies significantly depending on the specific condition and the individual’s response to treatment. While some diseases may lead to a gradual decline in function and quality of life, others may allow individuals to maintain a relatively stable level of functioning for extended periods. Factors such as the age of onset, genetic predisposition, and access to appropriate medical care all influence the long-term trajectory of these diseases.
Summary Table of Progressive Diseases
| Disease | Symptoms | Progression | Treatment |
|---|---|---|---|
| Alzheimer’s Disease | Memory loss, confusion, disorientation | Gradual decline in cognitive function | Medications, therapies, support groups |
| Parkinson’s Disease | Tremors, rigidity, slowness of movement | Slow, progressive decline in motor skills | Medications, therapies, lifestyle modifications |
| Multiple Sclerosis | Vision problems, numbness, muscle weakness | Variable, relapsing-remitting or progressive | Medications, physical therapy, assistive devices |
| Chronic Obstructive Pulmonary Disease (COPD) | Shortness of breath, chronic cough | Progressive decline in lung function | Medications, pulmonary rehabilitation, oxygen therapy |
Research and Future Directions
Unraveling the complexities of progressive diseases requires a multifaceted approach, combining innovative research strategies with a commitment to patient-centered care. Ongoing research efforts are vital for developing more effective treatments, improving diagnostic tools, and ultimately enhancing the lives of those affected by these debilitating conditions. This exploration delves into current research, emerging therapies, and the future of progressive disease management.
Current Research Efforts
Research into progressive diseases is actively exploring diverse avenues. Genetic studies are identifying specific genes and pathways implicated in disease progression, leading to potential targets for therapeutic intervention. Epigenetic modifications, environmental factors, and interactions between different biological systems are also being investigated to understand the intricate mechanisms underlying disease development and progression. Advanced imaging techniques are used to monitor disease progression, enabling earlier detection and personalized treatment strategies.
Promising New Treatments or Therapies
Several promising new treatments and therapies are in development. Targeted therapies, designed to specifically address the underlying biological mechanisms driving disease progression, show significant potential. Immunotherapies are being explored to modulate the immune response and potentially slow or halt disease progression. Gene therapies are aiming to correct genetic defects or enhance the body’s ability to combat the disease.
Stem cell therapies are also showing promise in repairing damaged tissues and organs, potentially restoring lost function.
Long-Term Goals of Research
Long-term research goals include achieving a better understanding of the intricate biological mechanisms behind progressive diseases. This knowledge will enable the development of more effective preventive strategies, early detection methods, and personalized treatment plans. The ultimate aim is to delay or even halt disease progression, thereby improving quality of life and reducing the burden on patients and their families.
For example, in neurodegenerative diseases, the goal is not just to alleviate symptoms but to discover and implement therapies that directly combat the underlying causes of neuronal death.
Challenges and Opportunities for Future Research
Challenges in future research include the complexity of the diseases themselves, the diversity of patient populations, and the ethical considerations surrounding new treatments. However, these challenges also present opportunities. The development of innovative technologies, such as artificial intelligence and machine learning, offers the potential to analyze large datasets and identify patterns that could lead to breakthroughs in diagnosis, prognosis, and treatment.
Collaboration between researchers, clinicians, and patients is essential to address these challenges and realize the opportunities.
Role of Technology in Advancing Research and Treatment
Technology plays a crucial role in advancing progressive disease research and treatment. Advanced imaging techniques, such as MRI and PET scans, provide detailed visualizations of disease progression, enabling earlier diagnosis and monitoring. High-throughput screening technologies are accelerating the identification of potential drug targets. Bioinformatics and data analysis tools facilitate the analysis of complex biological data, leading to a deeper understanding of disease mechanisms.
Furthermore, telemedicine and remote monitoring technologies empower patients to actively participate in their care and enable more efficient data collection. For instance, wearable sensors can monitor physiological parameters in real-time, offering valuable insights into disease progression and treatment response.
Last Recap

In conclusion, progressive diseases are multifaceted conditions that demand a holistic approach to understanding and managing. From the initial definition to the latest research, this exploration has highlighted the complex interplay of factors involved. The impact on patients and families is undeniable, emphasizing the importance of support systems and patient advocacy. This discussion underscores the need for continued research, innovative treatment strategies, and unwavering support for those facing these challenges.