Follow up after joint replacement surgery is crucial for a smooth recovery. This comprehensive guide covers everything from pre-operative expectations to post-operative care, physical therapy, pain management, diet, activity levels, medication, communication, home care, and potential complications. Understanding these aspects will empower you to navigate this significant life change with confidence and make informed decisions throughout your journey.
We’ll delve into the specifics of each phase, providing actionable insights and practical advice. From preparing for the surgery to managing potential complications, this guide will be your trusted companion as you embark on your path to recovery.
Pre-operative Steps and Expectations

Navigating the journey to joint replacement surgery can feel overwhelming. Understanding the pre-operative steps and what to expect during recovery can ease anxiety and empower you to take an active role in your health journey. This post Artikels the essential pre-operative procedures, the anticipated timeline, common concerns, and crucial distinctions between different joint replacements.The road to a successful joint replacement begins long before the operating room.
Thorough preparation, including a comprehensive medical evaluation, ensures the procedure is tailored to your individual needs and minimizes potential risks. A clear understanding of the pre-operative process and the recovery timeline will help you manage expectations and focus on your well-being throughout the entire experience.
Pre-operative Evaluations
A crucial aspect of preparing for joint replacement surgery is undergoing a thorough pre-operative evaluation. This process involves a series of assessments to ensure your health is optimal for the procedure. These evaluations aim to identify and address any potential complications and to tailor the surgical approach to your specific needs. Pre-operative evaluations often include:
- Medical history review: A detailed discussion of your medical history, including past illnesses, surgeries, allergies, and current medications, helps the surgical team understand your overall health status and identify any potential complications.
- Physical examination: A comprehensive physical examination evaluates your current physical condition, including your range of motion, muscle strength, and overall mobility. This assessment provides valuable data for the surgical plan.
- Blood tests and imaging: Blood tests and imaging scans, such as X-rays, CT scans, or MRIs, provide detailed images and data on the condition of your joints. This information assists in diagnosing the extent of the joint damage and aids in determining the best course of action.
- Cardiopulmonary evaluation: A thorough evaluation of your heart and lung health is essential, particularly for patients with underlying cardiovascular or respiratory conditions. This evaluation ensures the surgery is performed safely and minimizes potential risks.
Expected Recovery Timeline
The recovery process following joint replacement surgery varies based on individual factors like age, overall health, and the specific type of procedure. A realistic understanding of the recovery timeline can help you manage expectations and create a supportive environment for healing. While each patient’s journey is unique, a general timeline can offer a helpful framework.
- Initial recovery (first few weeks): The first few weeks post-surgery are crucial for managing pain, swelling, and mobility. Expect a gradual increase in activity levels, guided by your healthcare provider. Physical therapy plays a vital role in regaining strength and function.
- Mid-term recovery (several weeks to months): During this phase, you will continue physical therapy to improve range of motion and strength. Pain management will continue to be an important aspect of your recovery. Expect gradual improvements in mobility and daily activities.
- Long-term recovery (months to years): Long-term recovery focuses on maintaining the gains made during the mid-term phase. Ongoing physical therapy, regular check-ups, and lifestyle adjustments are crucial for long-term success.
Common Concerns and How to Address Them
Many patients experience anxiety and apprehension before joint replacement surgery. Addressing these concerns proactively can alleviate stress and promote a positive surgical experience.
- Pain management: Concerns about post-operative pain are common. The surgical team will develop a comprehensive pain management plan to ensure you are comfortable throughout the recovery process.
- Mobility limitations: Potential limitations in mobility can be daunting. Physical therapy and rehabilitation exercises are crucial in regaining strength and functionality.
- Surgical complications: Concerns about potential complications are valid. Open communication with your healthcare team can address these concerns and provide reassurance.
Types of Joint Replacements and Pre-operative Steps
| Joint Type | Description | Pre-operative Steps |
|---|---|---|
| Hip Replacement | Surgical procedure to replace the hip joint | Comprehensive medical history, physical examination, blood tests, imaging scans, and cardiopulmonary evaluation |
| Knee Replacement | Surgical procedure to replace the knee joint | Detailed medical history, physical examination, blood tests, imaging scans, and cardiopulmonary evaluation |
| Shoulder Replacement | Surgical procedure to replace the shoulder joint | Thorough medical history, physical examination, blood tests, imaging scans, and cardiopulmonary evaluation |
Post-operative Follow-up Plan
Following joint replacement surgery, a structured post-operative follow-up plan is crucial for successful recovery and long-term well-being. This plan ensures that any complications are detected early and that the patient’s progress is monitored closely. A dedicated team of healthcare professionals, including the surgeon, physical therapist, and other specialists, will work together to guide the patient through the recovery process.Regular follow-up appointments are vital in maintaining a smooth recovery.
Each visit provides an opportunity to assess the patient’s progress, address any concerns, and adjust the treatment plan as needed. This proactive approach minimizes potential risks and ensures the best possible outcome.
Follow-up Appointment Schedule
A well-defined schedule for follow-up appointments is essential to monitor recovery effectively. This schedule should be tailored to the individual patient’s needs and the specific type of joint replacement surgery performed. Initial follow-ups are typically more frequent, decreasing in frequency as the patient progresses.
- Initial Post-operative Visit (1-2 weeks): This visit focuses on assessing the surgical site, pain levels, and overall recovery. The patient’s mobility and range of motion are also evaluated. Any early complications, such as infection or excessive swelling, can be identified and addressed promptly.
- Follow-up Visits (1 month, 3 months, 6 months): These visits are critical in monitoring the healing process and identifying any long-term issues. The focus shifts to evaluating the patient’s long-term mobility, strength, and overall function. These visits also allow the healthcare team to provide necessary adjustments to the rehabilitation plan.
- Annual Check-ups (after 6 months): Annual check-ups allow for ongoing monitoring of the joint replacement. This helps detect any potential issues, such as loosening or wear, that might not manifest immediately.
Potential Complications
Post-operative complications can arise, although they are not common. Recognizing the potential signs and symptoms is vital for prompt intervention.
- Infection: Signs of infection include increased pain, swelling, redness, warmth, and drainage from the surgical site. Fever and chills are also possible indicators.
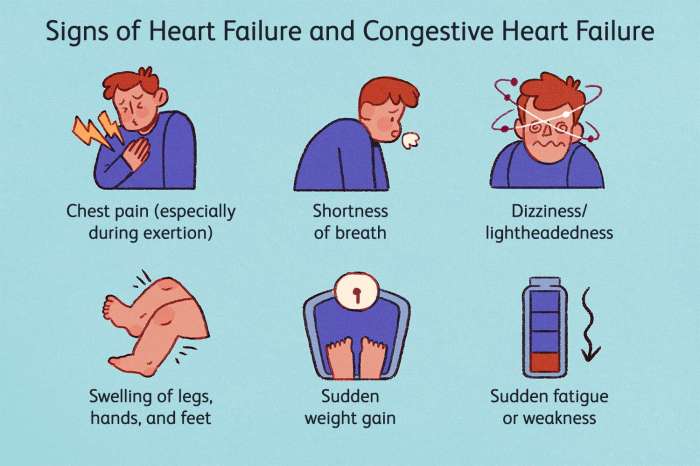
- Blood clots: Symptoms of blood clots include swelling, pain, and warmth in the leg. In severe cases, shortness of breath or chest pain might occur.
- Loosening of the implant: A loosening implant may cause increased pain, clicking, or grinding sensations during movement. Reduced range of motion and instability are also possible signs.
- Nerve damage: Nerve damage can manifest as numbness, tingling, or pain in the affected limb. The area may also feel weak or unresponsive.
Questions to Ask at Follow-up Visits
Patients should actively participate in their follow-up appointments by asking relevant questions. These questions help ensure that their concerns are addressed and that the best possible care is provided.
- Regarding Pain Management: “How can I further manage my pain effectively?” “Are there any alternative pain relief options?”
- Regarding Mobility and Rehabilitation: “What exercises should I be doing at home?” “Are there any modifications I should make to my daily activities?”
- Regarding Potential Complications: “What are the warning signs of infection or blood clots?” “What are the next steps if I experience any of these symptoms?”
- Regarding Long-Term Outcomes: “What is the expected lifespan of the implant?” “How often should I schedule follow-up visits?”
Physical Therapy and Rehabilitation
Recovering from joint replacement surgery is a journey, and physical therapy is a crucial component of that journey. It’s designed to restore function, reduce pain, and improve your overall well-being. This comprehensive approach focuses on building strength, improving mobility, and regaining independence. It’s not just about exercises; it’s about tailoring a personalized plan to your specific needs and goals.Physical therapy plays a vital role in guiding you through the rehabilitation process, helping you safely regain strength and movement in your newly replaced joint.
It’s a partnership between you and your physical therapist, where you actively participate in your recovery. The therapy addresses any limitations you might have and helps you learn techniques for daily living activities.
Role of Physical Therapy
Physical therapy after joint replacement surgery is essential for regaining strength, flexibility, and mobility. It addresses pain management, improves range of motion, and enhances functional independence. The goal is to return you to your pre-surgery activities as safely and effectively as possible.
Types of Exercises and Techniques
A variety of exercises and techniques are employed in physical therapy for joint replacement recovery. These are carefully selected and progressively introduced to ensure optimal results. Common approaches include:
- Range-of-motion exercises: These exercises aim to increase the movement of the joint, improving flexibility and reducing stiffness. Examples include gentle bending, straightening, and rotating motions.
- Strengthening exercises: These exercises target specific muscles surrounding the replaced joint to improve strength and stability. Examples include isometric exercises (holding a position), isotonic exercises (moving a weight), and resistance band exercises.
- Balance exercises: These exercises help improve stability and reduce the risk of falls. Examples include standing on one leg, heel-toe walking, and exercises on an unstable surface.
- Functional exercises: These exercises mimic daily activities, such as walking, climbing stairs, and getting in and out of chairs. This helps prepare you for your return to normal activities.
- Manual therapy techniques: These techniques involve hands-on treatment methods such as massage, mobilization, and manipulation to address joint stiffness and pain.
Expected Progression of Physical Therapy Sessions
Physical therapy sessions typically begin immediately after surgery or as soon as the medical team deems it safe. The initial sessions focus on pain management, wound care, and gentle range-of-motion exercises. As you progress, the exercises become more challenging and incorporate strengthening and functional exercises. The progression is tailored to your individual recovery and response to treatment.
A common example is starting with simple seated exercises and progressing to standing exercises, and finally to exercises that mimic daily activities.
Comparison of Physical Therapy Approaches
Different physical therapy approaches may be used, each with its own strengths and weaknesses. The best approach is often determined by individual patient needs and preferences.
| Approach | Description | Strengths | Weaknesses |
|---|---|---|---|
| Manual Therapy | Focuses on hands-on techniques to address joint mobility and pain. | Can provide immediate pain relief and improve range of motion. | May not be suitable for all patients or injuries. |
| Exercise-Based Therapy | Emphasizes strengthening and functional exercises to improve joint function. | Effective for restoring strength and function. | May not address pain or stiffness as effectively as manual therapy. |
| Combination Approach | Combines manual therapy and exercise-based therapy for a holistic approach. | Addresses pain, improves mobility, and restores strength and function. | Requires more time and effort from the patient and therapist. |
Pain Management Strategies
Post-joint replacement surgery, managing pain effectively is crucial for a smooth recovery. A well-rounded approach encompassing medication, physical therapies, and alternative methods can significantly improve comfort and hasten the healing process. This section delves into various strategies, emphasizing the importance of individualized pain management plans and the escalation process should pain persist or worsen.Pain after joint replacement surgery can vary in intensity and duration, and managing it effectively is key to optimal recovery.
Strategies for pain management are tailored to the individual’s needs and response to treatment. A multi-faceted approach, combining medication, physical therapy, and alternative methods, is often the most successful.
Medication for Pain Relief
Effective pain management often relies on medication. Different types of medication offer varying levels of pain relief and side effects. Prescription pain relievers, like opioids, can provide strong pain relief but carry the risk of side effects, including addiction. Non-opioid medications, such as NSAIDs (nonsteroidal anti-inflammatory drugs) and acetaminophen, can be equally effective for moderate pain and often have fewer side effects.
Your doctor will prescribe the most suitable medication based on your individual needs and medical history. It’s important to strictly follow the prescribed dosage and schedule.
Physical Therapies for Pain Relief
Physical therapy plays a vital role in pain management. Specific exercises and techniques can help strengthen muscles around the affected joint, improve range of motion, and reduce pain. These therapies can help you regain your mobility and function. Physical therapists guide you through these exercises, ensuring proper form and technique. Examples include range-of-motion exercises, strengthening exercises, and manual therapy techniques to reduce muscle spasms and joint stiffness.
Alternative Pain Management Methods
Alternative methods, such as heat therapy, cold therapy, and acupuncture, can complement conventional pain management strategies. Heat therapy, for instance, can ease muscle soreness and stiffness, while cold therapy can reduce inflammation. Acupuncture involves inserting thin needles into specific points on the body to stimulate nerve pathways and reduce pain. While these methods are often well-tolerated, it’s important to consult with your healthcare provider before incorporating them into your pain management plan.
Their efficacy in reducing pain can vary significantly from person to person.
Following up after joint replacement surgery is crucial for a smooth recovery. One common issue that can arise, often needing additional care, is an MCL tear, or medial collateral ligament injury. Understanding these injuries, like mcl tear medial collateral ligament injuries , is important for patients to ensure they’re getting the right support during their recovery and post-operative follow-up appointments.
This proactive approach helps in achieving optimal results and minimizing complications after joint replacement surgery.
Escalating Pain Management
If your pain persists or worsens despite the initial pain management plan, it’s essential to escalate the treatment. This involves consulting your physician to adjust your medication, explore additional therapies, or consider other options. The escalation process should be transparent and well-defined to ensure prompt intervention if needed. Your doctor will assess your pain level, review your medical history, and adjust the treatment plan as necessary.
Following up after joint replacement surgery is crucial for a smooth recovery. One aspect often overlooked is how lung function, like the FEV1/FVC ratio in spirometry tests, can impact recovery. Understanding this ratio, as detailed in this article on FEV1/FVC ratio of FEV1 to FVC spirometry , can help your doctor tailor your rehabilitation plan, ensuring optimal lung health alongside your joint recovery.
Ultimately, careful follow-up appointments are key to a successful post-surgery journey.
Dietary Recommendations: Follow Up After Joint Replacement Surgery
Following joint replacement surgery, proper nutrition plays a crucial role in the healing process. A balanced diet provides the essential nutrients needed for tissue repair, reduces inflammation, and supports overall recovery. Paying attention to your dietary intake can significantly impact your journey to regaining strength and mobility.A well-structured diet is key to a successful recovery from joint replacement surgery.
The right nutrients help the body repair tissues, combat inflammation, and support the overall healing process. This includes focusing on specific nutrients, avoiding certain foods, and understanding how portion sizes affect recovery. This section will provide detailed dietary recommendations and guidance on incorporating nutritious foods into your post-operative diet.
Nutritious Foods to Include
A diet rich in protein, vitamins, and minerals is essential for supporting tissue repair and overall recovery. Including a variety of nutrient-dense foods will provide your body with the building blocks it needs.
- Lean Protein Sources: Lean meats, poultry, fish, beans, lentils, and tofu are excellent sources of protein, crucial for muscle repair and overall healing. These foods should be incorporated into meals throughout the day.
- Fruits and Vegetables: Fruits and vegetables provide essential vitamins, minerals, and antioxidants, which contribute to a healthy immune response and aid in reducing inflammation. Aim for a variety of colors to ensure a wide range of nutrients.
- Whole Grains: Whole grains like brown rice, quinoa, and whole-wheat bread provide complex carbohydrates, fiber, and essential nutrients that support energy levels and digestive health.
- Healthy Fats: Monounsaturated and polyunsaturated fats, found in avocados, nuts, seeds, and olive oil, are vital for hormone production, nutrient absorption, and overall health. Incorporate these healthy fats into your diet in moderation.
Dietary Restrictions or Modifications
Certain foods or food groups might need to be restricted or modified to avoid potential complications or discomfort during the recovery process.
Following up after joint replacement surgery is crucial for a smooth recovery. One often overlooked aspect of post-operative care is skin health, especially if you’re prone to conditions like eczema, particularly on areas that have undergone significant changes. Understanding how eczema manifests on dark skin can be particularly helpful in recognizing potential issues early on. For more information, check out this insightful resource on eczema on dark skin.
Regular check-ups and communication with your healthcare team remain key to a successful recovery journey.
- Sodium Restriction: High sodium intake can lead to water retention, which can cause swelling and discomfort. Consult with your healthcare provider to determine the appropriate sodium intake for your specific needs.
- Limited Sugar Intake: Excessive sugar intake can negatively impact inflammation and overall recovery. Opt for natural sugars from fruits instead of processed sugars.
- Hydration: Maintaining proper hydration is critical. Drink plenty of water throughout the day to support the healing process and prevent dehydration.
Impact of Diet on Healing
Proper nutrition significantly impacts the healing process. A balanced diet provides the building blocks for tissue repair and reduces inflammation, thus contributing to a faster and more comfortable recovery. Furthermore, it enhances the immune system’s ability to fight infection. This can prevent complications and contribute to overall well-being.
Activity Level and Mobility
Recovering from joint replacement surgery involves a gradual return to normal activity levels. This process is crucial for regaining strength, flexibility, and independence. A well-structured approach to increasing activity, utilizing assistive devices where needed, and understanding the limitations of the early recovery phase are key to a successful rehabilitation journey.
Importance of Gradual Progression
A gradual increase in activity levels is essential to prevent complications such as dislocations, infections, and excessive pain. Rushing the process can lead to setbacks and prolong the recovery time. Each individual’s healing process is unique, and a personalized approach is crucial for optimal results.
Safe and Effective Methods for Improving Mobility
Improving mobility after joint replacement surgery requires a combination of physical therapy exercises, assistive devices, and gradual increases in daily activities. A personalized exercise program, developed by a physical therapist, will target specific muscle groups and promote functional movement. Regular practice and adherence to the program are crucial for success.
Guide to Gradually Increasing Activity Levels
The following guide provides a framework for gradually increasing activity levels after joint replacement surgery. It is crucial to consult with a healthcare professional before starting any new activity and to modify the plan based on individual needs and progress.
- Early Phase (First few weeks): Focus on gentle movements, such as range-of-motion exercises, short walks with assistance, and seated exercises. The goal is to maintain joint flexibility and promote circulation without straining the newly replaced joint.
- Intermediate Phase (Weeks 4-8): Gradually increase the duration and intensity of activities. Introduce more complex exercises, longer walks, and light household chores under supervision. This stage involves building strength and endurance while maintaining safety.
- Advanced Phase (Weeks 8 onwards): Return to more demanding activities, such as gardening, climbing stairs, and engaging in hobbies. The focus shifts towards regaining pre-surgery functional levels and maintaining a healthy lifestyle. Careful monitoring and adjustments to the activity level are crucial to avoid setbacks.
Using Assistive Devices to Aid Mobility
Assistive devices, such as canes, walkers, and crutches, play a vital role in maintaining stability and reducing strain on the newly replaced joint during the recovery process. Proper use of these devices is essential for preventing falls and injuries. These devices are meant to be used temporarily and should be gradually discontinued as strength and mobility improve.
| Assistive Device | Description | Appropriate Use |
|---|---|---|
| Cane | A single-point support device. | Provides stability during walking and reduces stress on the operated leg. |
| Walker | A four-point support device. | Offers more stability than a cane and is useful for individuals with limited balance. |
| Crutches | Support the weight of the body through the arms. | Used during the initial stages of recovery, particularly for weight-bearing limitations. |
Remember, each patient’s experience is unique, and a personalized approach is crucial for a safe and effective recovery.
Medication Management
Proper medication management is crucial for a smooth recovery after joint replacement surgery. Adhering to the prescribed regimen, understanding potential side effects, and knowing when to contact your healthcare provider are vital for optimal healing and preventing complications. Consistent medication use, as directed, plays a significant role in pain control, preventing infection, and promoting the body’s natural healing process.Medication management after joint replacement surgery is more than just taking pills.
It’s about understanding the purpose of each medication, recognizing potential side effects, and communicating openly with your healthcare team. This allows for adjustments and proactive management of any issues that may arise. A clear understanding of your medication regimen will empower you to take an active role in your recovery.
Common Medications Prescribed
A variety of medications are commonly prescribed after joint replacement surgery. These medications are tailored to individual needs and are crucial for managing pain, preventing blood clots, and controlling inflammation.
- Pain relievers (e.g., opioids, nonsteroidal anti-inflammatory drugs (NSAIDs)): These medications help manage post-operative pain. Opioids, while effective, can have potential side effects, such as constipation and nausea. NSAIDs can also have side effects, including stomach upset and potential kidney issues. Following the prescribed dosage and reporting any discomfort to your doctor is essential.
- Blood thinners (e.g., warfarin, heparin): These medications prevent the formation of blood clots, which are a serious concern after surgery. Blood thinners require careful monitoring, and it’s important to follow the prescribed dosage and any dietary restrictions. For instance, some blood thinners can interact with certain foods and beverages, and it’s important to inform your doctor about any dietary changes.
- Antibiotics: These medications are often prescribed to prevent or treat infections. Following the full course of antibiotics is critical to ensure the infection is fully addressed and prevent recurrence.
- Anti-inflammatory medications (e.g., corticosteroids): These medications can reduce inflammation and swelling, contributing to faster recovery and improved mobility. The dosage and duration of these medications are tailored to the individual patient’s needs.
Potential Side Effects and Management
It’s crucial to be aware of potential side effects associated with the prescribed medications. Recognizing these effects allows you to take proactive steps and seek medical attention when necessary.
- Pain relievers: Common side effects include nausea, vomiting, constipation, and dizziness. Consuming foods rich in fiber, drinking plenty of water, and communicating with your healthcare provider about these side effects are important steps in managing them.
- Blood thinners: Side effects may include bleeding, bruising, or unusual nosebleeds. Contact your doctor immediately if you experience excessive bleeding or bruising.
- Antibiotics: Side effects may include diarrhea, nausea, or allergic reactions. Report any unusual symptoms to your doctor promptly.
- Anti-inflammatory medications: Potential side effects include stomach upset, fluid retention, or mood changes. Proper hydration, dietary modifications, and communicating any discomfort to your healthcare provider can help manage these effects.
When to Contact Your Healthcare Provider
It’s essential to know when to seek immediate medical attention regarding your medications. Open communication with your healthcare team is crucial for a smooth and successful recovery.
- Severe or persistent pain that is not relieved by the prescribed medication.
- Excessive bleeding or bruising.
- Signs of infection, such as fever, redness, swelling, or pus.
- Significant side effects that interfere with daily activities or cause discomfort.
- Any questions or concerns about the medication.
Communication Strategies
Effective communication is crucial for a successful joint replacement recovery journey. Open and honest dialogue with your healthcare team ensures your needs are met, concerns addressed, and your progress tracked accurately. This section will provide valuable insights into how to communicate effectively throughout your recovery process.Clear communication fosters a collaborative partnership between you and your healthcare providers. This involves actively participating in your care, asking questions, expressing concerns, and accurately reporting your symptoms.
Understanding how to communicate effectively can significantly improve your recovery experience and lead to better outcomes.
Effective Communication Techniques
Open and honest communication is key to successful recovery after joint replacement surgery. This involves actively listening to your healthcare providers and expressing your concerns clearly and concisely. The following strategies can help you communicate effectively with your healthcare team.
- Active Listening: Pay close attention to what your healthcare providers are saying, ask clarifying questions if needed, and demonstrate your understanding by summarizing their points.
- Proactive Questioning: Don’t hesitate to ask questions about your recovery, treatment plan, or any aspect that you don’t understand. Specific and clear questions will allow for more thorough and informative answers. Examples include: “What are the potential complications of this procedure?” or “How can I best manage my pain medication?”
- Expressing Concerns: Feel free to voice any concerns, worries, or questions, no matter how small they may seem. Your healthcare team is there to support you and address your concerns promptly. For instance, if you are experiencing unexpected side effects, share this information with your doctor immediately.
- Accurate Symptom Reporting: Provide detailed descriptions of your pain levels, other symptoms, and any changes you notice. This information is essential for your healthcare providers to monitor your progress and adjust your treatment plan as needed. Use a pain scale (numerical or visual) to provide a quantitative measure of your pain intensity, along with a description of the location and characteristics of the pain.
This will assist your healthcare providers in understanding the nature of your pain.
Strategies for Communicating Pain Levels, Follow up after joint replacement surgery
Accurate pain reporting is critical for effective pain management. A clear understanding of your pain allows healthcare professionals to adjust your treatment plan appropriately. This can significantly improve your recovery experience and help you avoid unnecessary pain.
- Using a Pain Scale: Employ a numerical or visual pain scale to quantify your pain level. This standardized approach allows your healthcare team to track changes in your pain over time. A visual analog scale (VAS) uses a line to measure pain intensity, while a numerical rating scale (NRS) uses numbers. Choose the scale that you find most comfortable and effective.
- Describing Pain Characteristics: Beyond the intensity, describe the quality of your pain. Is it sharp, dull, throbbing, or aching? Include information about the location, duration, and factors that seem to aggravate or relieve the pain. This detailed information will help your healthcare team determine the underlying cause and tailor a more effective treatment plan.
- Timing and Frequency of Pain: Note when the pain occurs (e.g., during specific activities, at rest, or at night). Keeping a pain diary can be helpful for tracking patterns and identifying triggers. This information can assist in identifying potential causes and implementing appropriate interventions.
Examples of Asking Questions and Expressing Concerns
Effective communication includes asking specific and clear questions and expressing concerns in a constructive manner.
- Specific Questions: Instead of asking “How am I doing?”, ask “What can I expect for pain management in the first week after surgery?”
- Expressing Concerns: Instead of saying “I’m worried,” express your concern with a specific example: “I’m concerned about the possibility of infection given the presence of this wound.”
Home Care s
Post-joint replacement surgery, your home becomes your sanctuary for recovery. A well-structured and supportive environment is crucial for healing and regaining mobility. This section Artikels key home care considerations to ensure a smooth transition and successful recovery.
Maintaining a Safe and Supportive Home Environment
Creating a safe and supportive home environment is paramount for a successful recovery. This involves minimizing potential hazards and maximizing accessibility. Clear pathways free of clutter are essential for safe movement. Remove any tripping hazards such as loose rugs or cords. Install grab bars in the bathroom and near the toilet to prevent falls.
Ensure adequate lighting throughout the home to improve visibility.
Wound Care
Proper wound care is critical for preventing complications and promoting healing. Follow your surgeon’s specific instructions meticulously. This includes keeping the incision site clean and dry, and reporting any signs of infection immediately. The wound should be inspected daily for any redness, swelling, drainage, or unusual odor. Keep the dressing clean and intact, changing it only as directed by your healthcare provider.
Avoid harsh scrubbing or applying any products not prescribed by your physician.
Bathing and Hygiene
Bathing and hygiene routines need adjustments to accommodate your recovery. Avoid submerging the surgical site in water until instructed by your surgeon. For the first few days, gentle sponge baths are often recommended. Use mild, fragrance-free soap and pat the skin dry thoroughly. Once you can shower, ensure the water temperature is lukewarm and avoid harsh scrubbing of the incision site.
Use a long-handled sponge or shower attachment to avoid bending over too much. Use a chair or stool for support during bathing and dressing.
Potential Complications and Prevention
Joint replacement surgery, while offering significant relief from pain and improved mobility, carries potential risks. Understanding these risks and preventative measures is crucial for a successful recovery. By actively participating in your care and following your healthcare team’s recommendations, you can minimize these risks and achieve optimal outcomes.
Potential Complications
Joint replacement surgery, like any major surgical procedure, carries a range of potential complications. These complications can vary in severity and impact the recovery process. Recognizing potential complications and understanding how to address them is vital for a smooth and successful recovery.
- Infection: Infection at the surgical site is a serious concern. It can manifest as redness, swelling, warmth, pain, or pus drainage around the implant. Prompt treatment is essential to prevent the spread of infection and potential implant failure.
- Blood clots (Deep Vein Thrombosis – DVT): Blood clots can form in the deep veins of the leg after surgery. These clots can dislodge and travel to the lungs (pulmonary embolism), causing significant respiratory distress. Proper anticoagulant therapy and mobility exercises can help prevent blood clots.
- Implant Loosening or Failure: Over time, the implant may loosen or fail due to various factors, including infection, excessive wear and tear, or improper bone healing. This can necessitate a revision surgery, a more complex procedure. Maintaining a healthy weight and engaging in recommended exercises can help support bone health and implant longevity.
- Nerve Damage: Nerve damage near the surgical site is a rare but possible complication. Symptoms can include numbness, tingling, or pain in the affected area. Nerve damage is usually temporary, but in rare cases, it can be permanent. Careful surgical technique and postoperative monitoring are crucial to minimize this risk.
- Stiffness: Stiffness in the joint is a common post-operative concern, particularly in the initial stages. Regular physical therapy is essential for maintaining range of motion and reducing stiffness.
Strategies for Preventing Complications
Proactive steps can significantly reduce the likelihood of complications. Adhering to prescribed medications, maintaining a healthy lifestyle, and following your physical therapist’s guidance are crucial for a successful recovery.
- Medication Adherence: Strictly adhering to the prescribed medication regimen, including antibiotics and blood thinners, is paramount. This helps prevent infections and blood clots. Never adjust your medication dosage without consulting your doctor.
- Healthy Lifestyle: Maintaining a healthy weight and following a balanced diet can support bone health and overall recovery. Smoking cessation is crucial, as smoking can negatively impact bone healing and increase the risk of complications.
- Early and Consistent Physical Therapy: Starting physical therapy as directed by your doctor and physical therapist is essential for regaining joint mobility and strength. Regular exercises can promote blood circulation and reduce the risk of blood clots.
- Proper Wound Care: Following instructions on wound care, including keeping the incision clean and dry, can help prevent infection. Be vigilant about signs of infection, such as redness, swelling, or drainage.
- Regular Follow-up Appointments: Regular follow-up appointments with your doctor are essential for monitoring your progress, addressing any concerns, and catching potential complications early. Do not hesitate to call your doctor if you have any questions or concerns.
Recognizing Early Warning Signs
Knowing the early warning signs of complications can enable swift intervention. Be aware of any changes in your condition and report them to your healthcare provider immediately.
- Increased Pain: Sudden or significantly increased pain that is not relieved by medication could indicate a problem. Document the pain’s characteristics (location, intensity, duration) for your doctor.
- Swelling or Redness: Increased swelling or redness around the surgical site can signal infection. Document any changes in appearance and report them immediately.
- Fever or Chills: Fever or chills can indicate infection. These symptoms should be reported to your doctor immediately.
- Numbness or Tingling: Any changes in sensation, such as numbness or tingling, near the surgical site should be reported to your doctor. This could indicate nerve damage.
- Shortness of Breath or Chest Pain: If you experience shortness of breath or chest pain, seek immediate medical attention, as this could be a sign of a pulmonary embolism.
Importance of Seeking Immediate Medical Attention
Prompt medical attention is critical if any of the aforementioned complications occur. Do not hesitate to call your doctor or seek emergency medical care if you experience concerning symptoms.
- Prompt Action Saves Lives: In cases of severe complications, such as a pulmonary embolism, prompt medical intervention can save lives.
- Early Intervention: Addressing potential complications early can often prevent them from escalating into more serious issues.
- Expert Medical Care: Your healthcare provider is best equipped to diagnose and treat complications, ensuring the best possible outcome.
Closing Notes
In conclusion, a successful recovery following joint replacement surgery hinges on a proactive and well-informed approach. This guide has equipped you with the knowledge and strategies needed to manage various aspects of your recovery journey, from pre-operative preparation to post-operative care. Remember, open communication with your healthcare team, consistent adherence to the recovery plan, and a positive mindset are essential ingredients for a fulfilling and successful outcome.