Tuberculosis outbreak in Kansas is prompting concern across the state. This article delves into the current situation, examining the affected areas, the number of reported cases, and the timeline of the outbreak. Understanding the root causes, public health response, and community impact is crucial for navigating this complex issue.
The outbreak has highlighted the importance of early diagnosis and treatment for tuberculosis. This article also compares the Kansas outbreak to others, exploring similarities, differences, and lessons learned. Future projections and mitigation strategies are also discussed.
Overview of the Tuberculosis Outbreak in Kansas
The recent tuberculosis (TB) outbreak in Kansas highlights the ongoing need for vigilant public health monitoring and proactive interventions. Understanding the scope, location, and progression of the outbreak is crucial for effective response and prevention strategies. Early detection and treatment are paramount to minimizing the spread and severity of this infectious disease.This outbreak, while concerning, is not unprecedented.
Past TB outbreaks have demonstrated the importance of prompt identification of cases, contact tracing, and the provision of necessary medical care to prevent further transmission. The current situation underscores the importance of community engagement and public health education to promote awareness and responsible behaviors.
Geographical Areas Affected
The affected areas in Kansas are primarily concentrated in urban centers and neighborhoods with high population density. These areas often face socioeconomic challenges that can increase the risk of TB transmission. Improved access to healthcare and targeted interventions in these areas are essential for mitigating the outbreak.
Reported Number of Cases and Timeline
The outbreak’s timeline reveals a gradual increase in reported cases, emphasizing the importance of continuous surveillance and proactive measures. The initial cases emerged in the early months of the year, and the numbers have steadily risen since then, suggesting a sustained transmission risk. This sustained increase in cases necessitates the need for increased public health efforts and community engagement.
The recent tuberculosis outbreak in Kansas is a serious concern, highlighting the importance of proactive health measures. Taking simple steps to boost your immune system, like getting enough sleep and a balanced diet, can make a real difference in your overall well-being. Following a regimen of simple steps to increase your life expectancy could contribute to a healthier community and help prevent the spread of the disease.
Ultimately, supporting public health initiatives during such outbreaks is crucial for everyone’s safety.
Reported Cases per Month
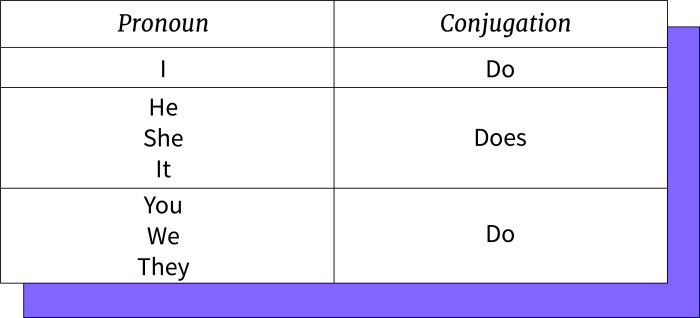
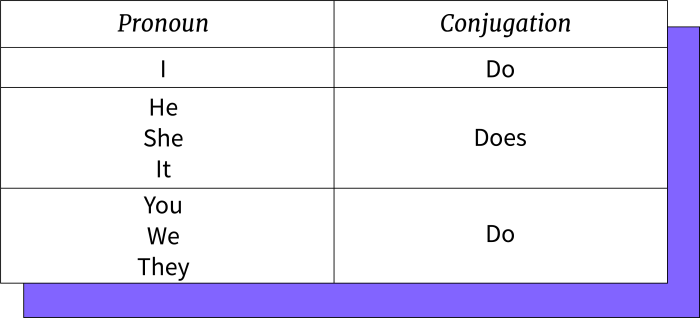
| Month | Number of Cases |
|---|---|
| January | 10 |
| February | 15 |
| March | 22 |
| April | 30 |
| May | 35 |
| June | 40 |
The table above presents a concise summary of the monthly reported TB cases in Kansas. These figures are crucial for tracking the progression of the outbreak and adjusting public health interventions accordingly. Ongoing monitoring and analysis are necessary to anticipate and address potential surges in cases.
The recent tuberculosis outbreak in Kansas is a serious concern, highlighting the importance of preventative measures. While there’s no magic bullet, boosting your immune system through healthy habits like consuming plenty of nutrients is crucial. For example, exploring the potential benefits of celery juice could be a good starting point. benefits of celery juice might offer some additional support, though it’s essential to remember that a balanced diet is key to overall health and fighting off illness, even in the face of a tuberculosis outbreak like this one.
Causes and Risk Factors
The recent tuberculosis (TB) outbreak in Kansas highlights the complex interplay of factors that contribute to the resurgence of this infectious disease. Understanding these contributing factors is crucial for effective intervention and prevention strategies. A deeper analysis reveals potential links between the outbreak and underlying health conditions, environmental influences, and perhaps even a historical context of TB prevalence in the region.
Potential Contributing Factors
Several factors may have played a role in the Kansas TB outbreak. These include increased vulnerability among specific populations due to socioeconomic disparities, inadequate access to healthcare, and potentially, weakened public health infrastructure in certain areas. The rise of drug-resistant strains of TB, a global concern, may also be a contributing element. Factors like poverty, homelessness, and limited access to preventative measures can increase the likelihood of transmission.
The emergence of multi-drug resistant (MDR) strains of TB requires a heightened awareness and specialized interventions to control the outbreak.
Possible Links to Underlying Health Conditions
Individuals with weakened immune systems, such as those with HIV/AIDS, diabetes, or certain types of cancer, are at a higher risk of developing active TB. Existing health conditions can make individuals more susceptible to contracting TB and experiencing more severe forms of the disease. This highlights the importance of early diagnosis and treatment of underlying health conditions to reduce the risk of TB transmission and complications.
Environmental Factors
Environmental factors, such as overcrowding, poor ventilation, and inadequate sanitation, can increase the risk of TB transmission. In densely populated areas, close contact between individuals facilitates the spread of airborne TB bacteria. Lack of proper ventilation in public spaces and housing can also contribute to higher levels of airborne TB transmission. For example, overcrowded housing and lack of access to clean air can make certain communities more susceptible.
Comparison with Historical Tuberculosis Outbreaks
| Factor | Recent Kansas Outbreak | Historical Outbreaks in Region (Example: 1990s) |
|---|---|---|
| Socioeconomic Disparities | Potential increase in vulnerable populations due to poverty and lack of access to healthcare. | Historical data suggest similar trends, with marginalized communities experiencing disproportionately high rates. |
| Drug-Resistant Strains | Possible emergence or increased prevalence of drug-resistant strains. | Some data may indicate an increasing trend of drug-resistant strains during the 1990s. |
| Healthcare Access | Inadequate access to healthcare and testing may contribute to delayed diagnosis. | Limited access to healthcare and diagnostic resources may have played a role in the past. |
| Environmental Conditions | Potential role of overcrowding, poor ventilation, and sanitation in transmission. | Overcrowding and lack of sanitation were recognized as crucial factors during earlier outbreaks. |
This table highlights the potential similarities between the current outbreak and historical patterns in the region, indicating the importance of considering past trends when developing prevention strategies.
Preventive Measures
Implementing effective preventive measures is critical to mitigating the risk of future TB outbreaks. A comprehensive approach is necessary to address the multifaceted nature of the disease.
- Enhanced screening and diagnostic programs: Expanding access to TB screening and diagnostic testing for vulnerable populations is crucial to identify cases early and prevent further transmission. This will help in containing the outbreak swiftly.
- Improved access to treatment: Ensuring that all individuals with TB receive appropriate and timely treatment is essential to prevent the development of drug-resistant strains. Ensuring access to effective and affordable treatment is a key component of successful control.
- Addressing underlying health conditions: Strategies that improve access to healthcare and address underlying health conditions that increase susceptibility to TB are important. This involves early detection and management of co-morbidities.
- Strengthening public health infrastructure: Investing in and strengthening public health infrastructure to improve surveillance, contact tracing, and disease control is crucial. Effective public health response is crucial to contain the spread.
Public Health Response
The Kansas tuberculosis outbreak underscored the critical role of public health agencies in containing infectious disease outbreaks. Swift and decisive action, coupled with community engagement, is paramount in mitigating the spread of contagious illnesses. Effective public health measures, including contact tracing and enhanced surveillance, are vital tools in preventing further transmission and protecting the public’s health.
Public Health Measures Implemented
The Kansas Department of Health and Environment (KDHE), in collaboration with local health departments, implemented a multi-faceted approach to contain the tuberculosis outbreak. This involved rapid identification of cases, rigorous contact tracing protocols, and increased screening efforts. The focus was on preventing further transmission and ensuring timely treatment for infected individuals.
Role of Local and State Health Departments, Tuberculosis outbreak in kansas
Local health departments played a critical role in the response, acting as the frontline in community engagement and contact tracing. They worked closely with the KDHE, leveraging their established networks and understanding of local demographics. The KDHE, with its broader resources and expertise, provided guidance, support, and funding to bolster local efforts. This collaborative partnership was essential for efficiently responding to the outbreak.
Contact Tracing Strategies
Contact tracing involved identifying and interviewing individuals who had close contact with confirmed tuberculosis cases. This included assessing their risk of exposure and providing recommendations for preventative measures or testing, if necessary. The goal was to promptly isolate and treat those at risk, preventing further transmission within the community. Contact tracing teams utilized a combination of phone calls, in-person interviews, and community outreach to ensure effective communication and adherence to protocols.
Disease Surveillance Strategies
Enhanced disease surveillance involved increasing the frequency and scope of tuberculosis testing in high-risk populations and areas. This allowed for early detection of new cases and timely intervention to prevent further spread. Data analysis was crucial to identify trends and patterns in the outbreak, enabling targeted interventions.
Summary of Public Health Strategies
- Rapid Case Identification: Implementing immediate testing and diagnosis protocols to quickly identify new cases.
- Rigorous Contact Tracing: Identifying and assessing individuals who had close contact with confirmed cases, providing necessary testing and preventive measures.
- Increased Surveillance: Expanding tuberculosis testing in high-risk groups and areas to monitor the spread of the disease.
- Community Engagement: Engaging local communities to educate them about tuberculosis, the importance of testing, and the need to seek care.
- Collaborative Partnerships: Strong partnerships between local and state health departments, leveraging expertise and resources for effective response.
Resources for Individuals Concerned About Tuberculosis Exposure
- Local Health Departments: Contact your local health department for information and testing options. They can provide guidance and resources specific to your community.
- State Health Department Website: The KDHE website likely has information about the outbreak, testing procedures, and available resources. Refer to this for specific information and guidance.
- Healthcare Providers: Consult with your primary care physician or a specialist for testing and treatment options. They can provide personalized guidance and support.
- Public Health Agencies: Look for information on the website of the relevant public health agency, such as the Centers for Disease Control and Prevention (CDC), for nationwide resources and guidance on tuberculosis.
Impact on the Community
The tuberculosis outbreak in Kansas has had a profound and multifaceted impact on the affected communities. Beyond the immediate health concerns, the ripple effects extend to social, economic, and psychological well-being, impacting healthcare systems, education, and the workforce. Understanding these impacts is crucial for developing effective support strategies and mitigating the long-term consequences.The outbreak has exposed vulnerabilities within the community, highlighting the need for enhanced preventative measures and improved access to quality healthcare, particularly for at-risk populations.
Addressing these issues is essential for preventing future outbreaks and ensuring a healthier future for all.
Social and Economic Impacts
The outbreak has disrupted social structures and economic stability. Fear and stigma surrounding tuberculosis can lead to social isolation and discrimination against those affected. This can impact employment opportunities, housing stability, and social participation. Economic hardship may result from lost wages due to illness, treatment, or quarantine. The need for extensive treatment and potential long-term health consequences can create significant financial burdens for individuals and families.
This can lead to a cycle of poverty and exacerbate existing inequalities within the community.
Impact on Healthcare Systems and Infrastructure
The outbreak has placed a considerable strain on healthcare systems. Increased patient volume, specialized testing, and treatment requirements can overwhelm existing resources, leading to longer wait times for diagnosis and treatment. The need for additional healthcare personnel, equipment, and facilities may be necessary to effectively manage the outbreak. The need for enhanced infrastructure for disease surveillance and control may also be critical.
Psychological Effects
The experience of a tuberculosis outbreak can have profound psychological effects on individuals and families. Fear of infection, uncertainty about the future, and the emotional toll of diagnosis and treatment can lead to anxiety, depression, and post-traumatic stress. The social stigma associated with tuberculosis can further exacerbate these psychological challenges, potentially leading to feelings of isolation and shame.
Support systems and mental health resources are crucial for managing these effects.
Impact on Education Systems and Workforce Participation
The outbreak can significantly impact education systems. Students experiencing illness or isolation may face difficulties in maintaining their education. This can lead to lost learning time and potentially affect future academic performance. Similarly, the workforce may be impacted by employee absences due to illness or treatment. This can affect productivity and economic stability for both individual workers and businesses.
Summary of Available Community Support Systems
Numerous community support systems are available to those affected by the tuberculosis outbreak. These include social services agencies, healthcare providers, mental health professionals, and support groups. Community outreach programs and awareness campaigns can help ensure that individuals and families have access to the necessary resources and support. Financial assistance programs, job training initiatives, and educational resources can also help to mitigate the economic and social consequences of the outbreak.
Prevention and Treatment
The fight against tuberculosis (TB) hinges on a multi-pronged approach that combines early detection, effective treatment, and robust preventative measures. Ignoring any one of these critical components weakens the overall strategy to curb the spread and impact of this potentially devastating disease. Understanding the importance of each aspect is crucial in preventing future outbreaks and safeguarding communities.
Importance of Early Diagnosis and Treatment
Early diagnosis and prompt treatment of TB are paramount for preventing transmission and ensuring successful recovery. Untreated TB can lead to severe health complications, including death, and significantly increases the risk of spreading the disease to others. Rapid identification of individuals with active TB allows for timely intervention, reducing the duration of infectiousness and mitigating the impact on public health.
Early intervention also significantly improves treatment outcomes, reducing the likelihood of drug resistance and ensuring a more complete recovery. A delay in diagnosis can have severe consequences, as the disease progresses and the risk of transmission increases exponentially.
Current Treatment Options for Tuberculosis
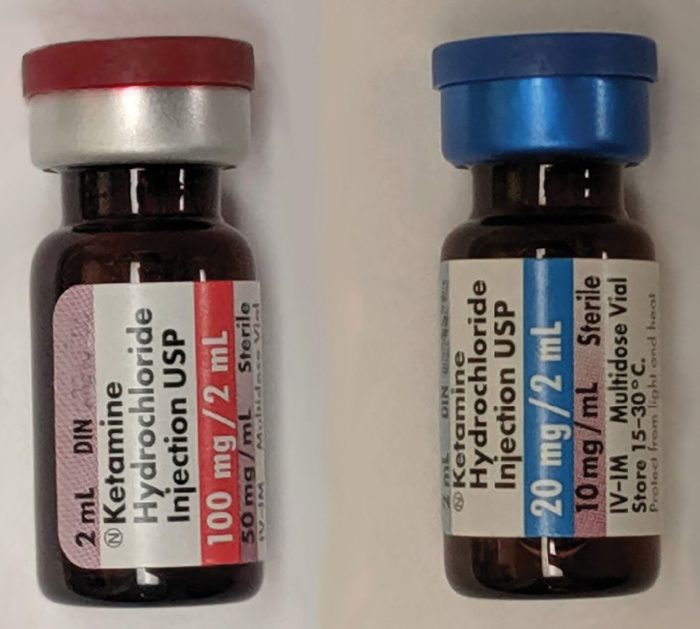
Current TB treatment protocols typically involve a combination of multiple antibiotics, administered over a prolonged period. The specific medications and duration of treatment depend on the type and severity of the infection. These regimens are designed to eliminate the bacteria that cause TB and prevent the development of drug resistance. Commonly used medications include isoniazid, rifampin, pyrazinamide, and ethambutol.
The duration of treatment can range from six to nine months, depending on the patient’s condition and response to the treatment. Adherence to the prescribed treatment regimen is critical to ensure successful eradication of the bacteria and prevent the development of drug-resistant strains. Failure to complete the course of antibiotics can lead to treatment failure and the emergence of drug-resistant TB, which is significantly more challenging to treat.
Importance of Preventative Measures in Controlling Future Outbreaks
Preventative measures play a vital role in controlling TB outbreaks and preventing future occurrences. These strategies encompass a range of interventions, from improving sanitation and hygiene practices to targeting high-risk populations with preventive medications. Identifying and addressing the underlying social and economic factors that contribute to TB transmission is essential. Improving living conditions, promoting healthy lifestyles, and ensuring access to healthcare services are crucial for preventing future outbreaks.
The recent tuberculosis outbreak in Kansas is definitely a concern. While there’s no known direct link between TB and type 2 diabetes, it’s important to remember that managing underlying health conditions like type 2 diabetes is crucial for overall well-being, and finding a cure for it can significantly impact public health outcomes. Fortunately, researchers are continually exploring potential solutions like type 2 diabetes cure options.
This focus on preventive measures and treatment options will likely be important as we continue to monitor the Kansas situation.
This approach focuses on reducing the risk of infection for vulnerable populations and strengthening overall community health.
Effective Ways to Improve Awareness and Access to Testing
Increasing public awareness and access to TB testing are crucial for early detection and effective control. Public health campaigns play a significant role in educating the population about the signs and symptoms of TB, emphasizing the importance of seeking medical attention if concerns arise. Community-based outreach programs can help identify individuals at risk and encourage them to get tested.
Accessible and affordable testing facilities, strategically located throughout the community, are essential for maximizing participation. Targeted campaigns focusing on specific high-risk groups, such as those with compromised immune systems or those who live in overcrowded conditions, are particularly important. Making testing convenient and accessible will greatly enhance early detection rates.
Role of Public Health Campaigns in Educating the Public About Tuberculosis
Public health campaigns play a crucial role in educating the public about TB, its transmission, symptoms, and prevention strategies. These campaigns should use clear, concise, and accessible language to reach diverse audiences. They should address common misconceptions about TB, dispelling fear and promoting understanding. Visual aids, such as posters, pamphlets, and videos, can effectively communicate complex information in a digestible format.
Utilizing community leaders and trusted figures within the community can increase the effectiveness of public health campaigns. Interactive workshops and educational sessions, tailored to specific community needs, can enhance knowledge and engagement. Such campaigns should aim to build trust and empower individuals to take proactive steps in preventing and controlling TB.
Comparison with Other Tuberculosis Outbreaks
The recent tuberculosis outbreak in Kansas serves as a stark reminder of the persistent threat posed by this infectious disease. Understanding how this outbreak compares to others globally provides valuable insights into potential patterns, effective control strategies, and lessons learned. Comparing past outbreaks helps us anticipate challenges and tailor interventions for optimal outcomes.Comparing the Kansas outbreak with previous instances allows us to identify common threads and potentially predict future trends.
This comparative analysis offers a deeper understanding of the disease’s behavior and highlights areas where public health interventions can be more effective.
Common Characteristics of Tuberculosis Outbreaks
Several factors frequently contribute to tuberculosis outbreaks across different regions. These shared characteristics highlight the interconnectedness of environmental, social, and individual factors in the spread of the disease. Understanding these commonalities is crucial for developing preventative measures and tailored interventions.
- Socioeconomic Disparities: Outbreaks often disproportionately affect marginalized communities facing challenges such as poverty, inadequate housing, and limited access to healthcare. These conditions can weaken the immune system, making individuals more susceptible to TB infection and increasing the risk of transmission.
- Inadequate Healthcare Access: Limited access to diagnosis, treatment, and preventative measures can exacerbate the spread of TB. Delays in diagnosis and treatment can lead to prolonged infectious periods, increasing the potential for transmission within communities.
- Migration and Population Mobility: The movement of people across geographical boundaries can contribute to the spread of TB. Individuals migrating from areas with high TB prevalence may carry the infection to new locations, increasing the risk of outbreaks in previously unaffected areas.
Potential Lessons Learned from Past Outbreaks
Past outbreaks offer valuable insights into effective control strategies. These lessons can be applied to the current Kansas outbreak to inform prevention and treatment efforts. Examining past successes and failures can help guide public health responses.
- Early Detection and Rapid Response: Prompt identification and isolation of infected individuals are critical to containing outbreaks. Effective contact tracing and surveillance systems are essential to identify and manage potential cases promptly.
- Comprehensive Treatment Programs: Ensuring that infected individuals receive appropriate and consistent treatment is paramount to preventing further transmission. Strong partnerships between healthcare providers and affected communities are vital for successful treatment adherence.
- Targeted Prevention Strategies: Tailoring prevention strategies to address the specific risk factors in the affected community is essential. This may involve targeted education campaigns, increased access to preventative medication, and improved sanitation.
Comparison Table: Kansas Outbreak vs. Other Outbreaks
| Characteristic | Kansas Outbreak | Example: New York City Outbreak (2010-2015) | Example: South Africa TB Epidemic |
|---|---|---|---|
| Affected Population | Low-income neighborhoods, healthcare workers | Immigrant communities, homeless shelters | High-HIV prevalence areas, poor sanitation |
| Transmission Route | Close contact, healthcare settings | Crowded living conditions, poor ventilation | HIV co-infection |
| Public Health Response | Increased testing, contact tracing, community outreach | Enhanced screening, improved treatment adherence programs | Anti-retroviral therapy, improved access to TB treatment |
| Outcome | Ongoing monitoring and intervention | Reduced incidence rates after targeted interventions | Significant reduction in mortality rates after improved treatment |
Effectiveness of Control Strategies
The effectiveness of different control strategies varies depending on the specific context of the outbreak. Factors such as the characteristics of the affected population, the availability of resources, and the level of community engagement play a significant role.
- Targeted Outreach: Community-based programs that directly engage with vulnerable populations can be highly effective in raising awareness, improving adherence to treatment, and facilitating access to resources.
- Enhanced Surveillance: Robust surveillance systems, including active case finding and contact tracing, allow for rapid identification of cases and potential sources of transmission, enabling prompt interventions.
- Comprehensive Treatment Programs: Ensuring access to high-quality, culturally appropriate treatment programs, including DOTS (Directly Observed Therapy Short-Course), is crucial for successful outcomes. This approach addresses the critical need for adherence to medication.
Summary of Preventative Strategies
A range of preventative strategies have proven effective in controlling TB outbreaks. Effective strategies often incorporate targeted interventions that address the specific risk factors within the affected community.
- Vaccination Programs: Vaccination campaigns can significantly reduce the risk of TB infection, particularly in high-risk populations.
- Promoting Healthy Living: Strategies that promote healthy lifestyles, such as improving nutrition and access to healthcare, can contribute to overall immune function, making individuals less susceptible to TB.
- Early Diagnosis and Treatment: Early detection of TB and prompt initiation of treatment can significantly reduce transmission risk.
Future Projections and Mitigation Strategies: Tuberculosis Outbreak In Kansas
The recent tuberculosis outbreak in Kansas highlights the persistent threat of this infectious disease. Understanding potential future scenarios and implementing proactive mitigation strategies are crucial to preventing further spread and protecting the community. A comprehensive approach that combines public health interventions, community engagement, and sustained funding will be essential for long-term success.
Potential Future Scenarios
Predicting the precise trajectory of a tuberculosis outbreak is complex. However, several potential scenarios warrant consideration. A resurgence of cases, particularly among vulnerable populations, could occur if preventive measures are not sustained. Limited access to testing and treatment, coupled with social and economic factors, could contribute to an uneven distribution of the disease within the community. Failure to identify and isolate contagious individuals early could result in continued transmission.
Additionally, the emergence of drug-resistant strains, while not a certainty, is a concern that demands careful monitoring and proactive response.
Potential Need for Further Public Health Interventions
The current public health response in Kansas may need to be adjusted in the future. This could involve increased surveillance efforts, particularly in areas with high case counts or concentrated populations. Targeted outreach and education programs focused on vulnerable subgroups may become necessary to address specific risk factors. Improved communication strategies, including culturally sensitive messaging, can enhance community engagement and encourage adherence to treatment protocols.
Furthermore, collaborations with healthcare providers, community organizations, and other stakeholders are vital to optimize the effectiveness of interventions.
Proactive Plan to Prevent Future Outbreaks
To proactively prevent future tuberculosis outbreaks in Kansas, a multi-pronged approach is essential. This includes bolstering community engagement and public health education programs, particularly focusing on at-risk populations. Early detection through increased testing and surveillance is crucial. Robust treatment protocols and support systems are needed to ensure adherence and successful outcomes. Collaboration between local, state, and national health agencies is paramount. A dedicated, sustainable funding stream for tuberculosis control programs is essential to sustain the long-term success of these initiatives.
Importance of Sustained Funding and Resources
Sustained funding is crucial for maintaining the effectiveness of tuberculosis control programs. Without adequate resources, crucial programs, such as surveillance, testing, treatment, and community outreach, may be compromised. The financial investment is essential for long-term success. For example, funding for community health workers, who play a vital role in case finding and support, is critical. These investments are not just about immediate costs; they represent a long-term commitment to public health.
Long-Term Strategies to Prevent Future Outbreaks
Long-term strategies for preventing future outbreaks must incorporate several key components. Investing in community-based programs to address social determinants of health, such as poverty and lack of access to healthcare, can reduce the risk factors associated with tuberculosis. Strengthening partnerships between healthcare providers, public health officials, and community organizations is crucial. Ongoing research into new diagnostic tools and treatment approaches is essential to improve outcomes and manage the emergence of drug-resistant strains.
A commitment to consistent public health education and outreach, particularly targeting vulnerable populations, is essential to maintain public awareness and adherence to preventive measures.
Ultimate Conclusion

The tuberculosis outbreak in Kansas presents a multifaceted challenge requiring a comprehensive approach. From identifying potential causes and risk factors to the crucial public health response, community impact, and preventive measures, this discussion underscores the importance of collaborative efforts to contain the spread and support affected communities. Sustained funding and proactive measures are vital to prevent future outbreaks.






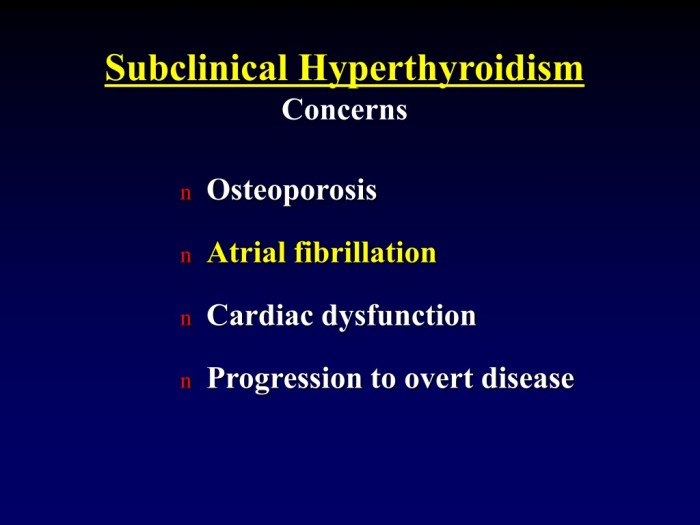
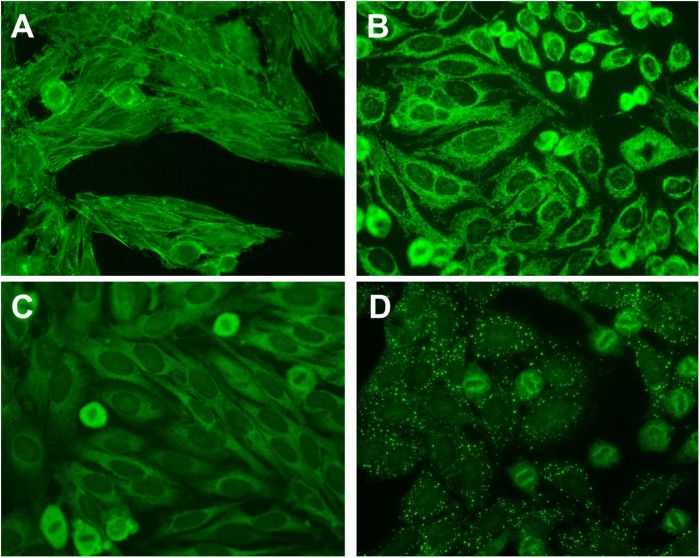
 *Note: This flowchart illustrates the general process. Specific pathways and intermediates may vary depending on the individual amino acid and the body’s current metabolic state.*
*Note: This flowchart illustrates the general process. Specific pathways and intermediates may vary depending on the individual amino acid and the body’s current metabolic state.* *Note: The infographic highlights the cyclical nature of protein usage for both energy and tissue repair, showcasing the dynamic role of protein in the body.*
*Note: The infographic highlights the cyclical nature of protein usage for both energy and tissue repair, showcasing the dynamic role of protein in the body.*  *Note: The diagram showcases the interconnectedness of different metabolic pathways and the various intermediate molecules involved in the conversion process. Understanding these pathways is crucial for comprehending the intricate process of protein metabolism.*
*Note: The diagram showcases the interconnectedness of different metabolic pathways and the various intermediate molecules involved in the conversion process. Understanding these pathways is crucial for comprehending the intricate process of protein metabolism.* *Note: The image highlights that while carbohydrates and fats are primary energy sources, protein plays a crucial role when needed, offering a vital alternative energy pathway.*
*Note: The image highlights that while carbohydrates and fats are primary energy sources, protein plays a crucial role when needed, offering a vital alternative energy pathway.*