8 tips for diabetic retinopathy prevention are crucial for maintaining eye health and overall well-being. This guide dives into actionable strategies to protect your vision, starting with understanding the critical link between diabetes and potential eye complications. Preventing diabetic retinopathy is a proactive approach to safeguarding your sight, and the following eight tips will equip you with the knowledge and tools to do so.
Diabetic retinopathy is a serious eye disease that can develop in people with diabetes. Early detection and proactive prevention strategies are key to maintaining good vision. This guide provides a comprehensive overview of eight practical steps that can significantly reduce your risk. These steps range from managing blood sugar levels to maintaining healthy lifestyle choices.
Introduction to Diabetic Retinopathy Prevention
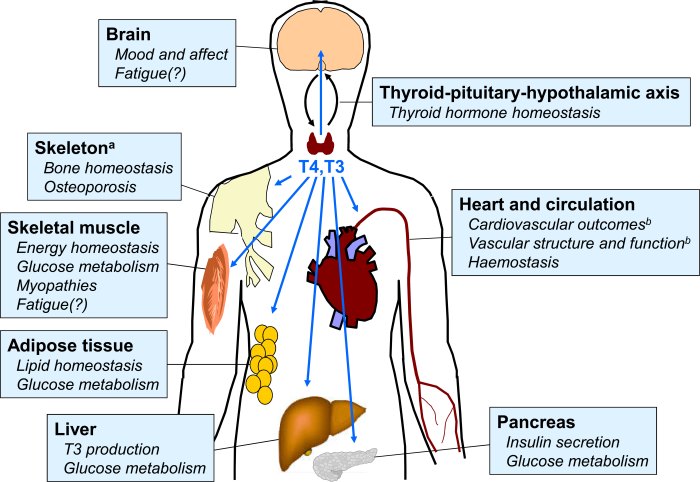
Diabetic retinopathy is a serious eye complication that can arise from diabetes. It’s a condition where the blood vessels in the retina, the light-sensitive tissue lining the back of the eye, become damaged. This damage can lead to vision loss, ranging from mild blurring to complete blindness if left untreated. Understanding the link between diabetes and eye health, and proactively taking steps to prevent diabetic retinopathy, is crucial for maintaining good vision throughout life.Diabetes affects the delicate blood vessels throughout the body, including those in the eyes.
High blood sugar levels over time can weaken and damage these vessels, causing them to leak fluid or bleed into the retina. This process, if not addressed, can lead to vision problems and potentially permanent vision loss. Early detection and proactive prevention strategies are vital for preserving sight in individuals with diabetes.
Importance of Early Detection and Prevention
Early detection of diabetic retinopathy is paramount. Catching the condition in its early stages allows for timely intervention and management, often preventing severe vision loss. Proactive prevention strategies, focusing on managing blood sugar levels and maintaining overall health, are critical in minimizing the risk of developing the condition in the first place. The potential consequences of untreated diabetic retinopathy are significant, including blurred vision, floaters, reduced visual acuity, and eventually, blindness.
Potential Consequences of Untreated Diabetic Retinopathy
Untreated diabetic retinopathy can have a profound impact on a person’s quality of life. Blurred vision, making everyday tasks challenging, is an early sign. Floaters, or small, dark spots that seem to drift in the field of vision, are another early indicator. Reduced visual acuity can progressively limit a person’s ability to perform tasks like reading or driving.
Ultimately, severe cases can lead to blindness, significantly impacting a person’s independence and overall well-being. Imagine the struggles of navigating daily life without the ability to see clearly, or the loss of loved ones’ faces.
Overview of 8 Tips for Prevention
These 8 tips are designed to help individuals with diabetes proactively manage their eye health and reduce the risk of developing diabetic retinopathy. By incorporating these practices into their daily routine, individuals can significantly lower their chances of experiencing vision loss.
Tips for Preventing Diabetic Retinopathy
| Tip | Category | Description |
|---|---|---|
| Maintain Optimal Blood Sugar Control | Lifestyle | Strict adherence to prescribed medication and a healthy diet can help maintain stable blood glucose levels. Regular blood sugar monitoring is crucial for early detection and timely intervention. |
| Regular Eye Exams | Medical Care | Routine eye exams are essential for early detection of any changes in the retina. Early diagnosis allows for timely treatment and potentially prevents vision loss. |
| Healthy Diet | Lifestyle | A balanced diet rich in fruits, vegetables, and whole grains, coupled with a limited intake of processed foods and sugary drinks, is crucial for maintaining overall health and controlling blood sugar. |
| Regular Exercise | Lifestyle | Physical activity helps manage weight, control blood sugar levels, and improve overall cardiovascular health, all of which are vital for protecting eye health. |
| Manage Blood Pressure | Medical Care | High blood pressure can exacerbate damage to blood vessels, increasing the risk of diabetic retinopathy. Maintaining healthy blood pressure levels is crucial. |
| Manage Cholesterol Levels | Medical Care | High cholesterol can contribute to the hardening of arteries, potentially impacting blood flow to the retina. Managing cholesterol levels is important for overall health and eye health. |
| Quit Smoking | Lifestyle | Smoking damages blood vessels throughout the body, including those in the eyes. Quitting smoking significantly reduces the risk of developing diabetic retinopathy. |
| Stress Management | Lifestyle | Chronic stress can negatively impact blood sugar control. Employing stress-reducing techniques, such as meditation or yoga, can improve overall health and eye health. |
Blood Sugar Control
Maintaining stable blood sugar levels is paramount in preventing diabetic retinopathy. High blood sugar damages the tiny blood vessels in the retina, leading to swelling, leakage, and ultimately, vision impairment. Consistent efforts to manage blood sugar levels are crucial for preserving vision and overall health.Blood sugar management isn’t a one-size-fits-all approach. It requires understanding your body’s response to food and medication, and adapting your lifestyle to achieve and maintain healthy blood glucose levels.
A combination of dietary choices, regular exercise, and medication (when prescribed) plays a vital role in this process. Consistency is key; a single instance of uncontrolled blood sugar can have detrimental effects.
Strategies for Stable Blood Glucose Levels
Maintaining consistent blood glucose levels involves a multifaceted approach. This includes dietary adjustments, regular exercise, and medication adherence. A balanced diet rich in fruits, vegetables, and whole grains, coupled with controlled portion sizes, helps regulate blood sugar influx. Regular physical activity improves insulin sensitivity, further aiding in blood glucose control. Medication, if prescribed, should be taken as directed by your healthcare provider.
Importance of Regular Blood Sugar Monitoring
Regular blood sugar monitoring is an essential tool in managing diabetes and preventing retinopathy. It provides real-time insights into how your body responds to various factors, allowing for proactive adjustments in your treatment plan. By tracking blood sugar levels throughout the day, you gain a comprehensive understanding of patterns and triggers, enabling you to make informed choices about your lifestyle.
Blood Sugar Monitoring Methods
Regular blood sugar monitoring provides crucial data for managing blood sugar levels effectively. Different methods offer varying levels of convenience and detail.
| Method | Frequency Recommendation | Benefits | Considerations |
|---|---|---|---|
| Finger-prick blood glucose meter | 1-4 times daily, or as directed by a healthcare professional. | Provides immediate, precise readings. Allows for adjustments to diet and medication based on real-time data. | Can be inconvenient. Requires patient self-monitoring. |
| Continuous Glucose Monitor (CGM) | 24/7 monitoring, typically calibrated with finger-prick testing. | Provides a continuous record of blood sugar levels. Alerts for high or low readings. Helpful in identifying patterns. | More expensive than finger-prick meters. May require more frequent calibration. |
| Self-Monitoring of Blood Glucose (SMBG) | As recommended by a healthcare professional. | Allows for immediate and precise blood sugar readings. Provides a tangible understanding of how your body reacts to various situations. | Requires dedicated time and attention. Can be inconvenient for those with busy schedules. |
| Urine glucose test | Less frequent than finger-prick testing. | Provides an overall assessment of blood sugar levels. | Less accurate than finger-prick testing. Doesn’t show immediate or fluctuating levels. |
HbA1c Levels and Retinopathy Risk
Hemoglobin A1c (HbA1c) reflects average blood sugar levels over a period of approximately three months. High HbA1c levels indicate a higher risk of developing diabetic retinopathy. For example, a patient with consistently high HbA1c levels (e.g., above 8%) is more susceptible to retinopathy compared to a patient with HbA1c levels consistently below 7%. Maintaining HbA1c levels within the target range, as determined by your healthcare provider, is critical for preventing and managing retinopathy.
HbA1c levels provide a long-term perspective on blood glucose control, offering a valuable indicator of retinopathy risk.
Healthy Diet for Prevention

A healthy diet is paramount in managing diabetes and preventing complications, including diabetic retinopathy. Proper nutrition plays a vital role in maintaining healthy blood sugar levels, reducing oxidative stress, and supporting overall eye health. A balanced diet rich in specific nutrients can significantly lower the risk of developing or progressing retinopathy.
Significance of a Balanced Diet
A well-balanced diet, tailored to the specific needs of individuals with diabetes, is crucial for preventing diabetic retinopathy. This dietary approach not only helps manage blood sugar levels but also supports overall eye health. By providing the essential nutrients, vitamins, and antioxidants, a balanced diet can protect the delicate tissues of the eyes, reducing the risk of damage.
This preventive measure can help maintain good vision and delay or even prevent the progression of retinopathy.
Essential Nutrients for Eye Health
Several nutrients are vital for maintaining healthy eyes. These include vitamins like A, C, and E, as well as minerals like zinc. These nutrients contribute to the overall health and function of the eye’s tissues, reducing the risk of damage from oxidative stress. Antioxidants are particularly important for protecting the delicate structures within the eye from free radical damage.
Role of Antioxidants in Protecting the Eyes
Antioxidants neutralize free radicals, unstable molecules that can damage cells and tissues, including those in the eyes. This damage is a significant contributor to the development and progression of diabetic retinopathy. Dietary antioxidants, such as vitamins C and E, beta-carotene, and zinc, can effectively combat this oxidative stress. By consuming foods rich in these antioxidants, individuals can protect their eyes from damage.
Dietary Recommendations for Diabetics
For individuals with diabetes, dietary recommendations should prioritize whole, unprocessed foods. These foods are rich in essential nutrients, vitamins, and minerals necessary for overall health, including eye health. Limiting processed foods, sugary drinks, and excessive saturated fats is equally important. A balanced diet that incorporates fruits, vegetables, lean proteins, and whole grains is key to maintaining optimal blood sugar control and protecting the eyes.
Healthy Food Choices for Eye Health
A diet rich in fruits, vegetables, and whole grains provides essential vitamins, minerals, and antioxidants, supporting eye health.
| Food Choice | Nutrient Content | Impact on Eye Health | Specific Benefits |
|---|---|---|---|
| Leafy Green Vegetables (Spinach, Kale) | Vitamins A, C, K; Minerals like lutein and zeaxanthin | Supports retina health, reduces oxidative stress | Protects against macular degeneration and cataracts. |
| Berries (Blueberries, Strawberries) | Antioxidants (vitamin C, anthocyanins) | Neutralizes free radicals, protects against damage | Improves blood flow to the eyes, supports retinal health. |
| Fatty Fish (Salmon, Tuna) | Omega-3 fatty acids | Supports healthy blood vessels, reduces inflammation | Contributes to overall eye health, potentially slowing the progression of retinopathy. |
| Citrus Fruits (Oranges, Grapefruit) | Vitamin C | Powerful antioxidant, protects against damage | Supports collagen production, vital for eye tissues. |
| Nuts and Seeds (Almonds, Walnuts) | Vitamin E, healthy fats | Powerful antioxidant, protects against oxidative stress | Supports cell membrane health, reducing inflammation in the eyes. |
Regular Exercise and Physical Activity: 8 Tips For Diabetic Retinopathy Prevention
Staying active is crucial for managing diabetes and protecting your eyes. Regular exercise helps regulate blood sugar levels, improves cardiovascular health, and reduces the risk of developing diabetic retinopathy. A consistent exercise routine can be a powerful tool in your diabetes management arsenal.Maintaining a healthy weight and lowering blood sugar levels are significant benefits of physical activity. Exercise also strengthens blood vessels, reducing the risk of damage and complications, including diabetic retinopathy.
This proactive approach significantly contributes to overall eye health and well-being.
Benefits of Exercise for Blood Sugar Control
Exercise increases insulin sensitivity, meaning your body utilizes insulin more effectively to lower blood glucose levels. This effect can last for several hours after exercise, making it a valuable tool for managing blood sugar fluctuations. Consistent physical activity also promotes weight management, which is another critical factor in controlling blood sugar. Studies have shown that even moderate exercise can make a substantial difference in blood sugar control for people with diabetes.
Types of Exercises Suitable for Diabetics
A wide variety of exercises are beneficial for people with diabetes. Aerobic activities, such as brisk walking, swimming, cycling, and dancing, are excellent choices. Strength training exercises, like lifting weights or using resistance bands, are also important for building muscle mass. Yoga and tai chi can improve balance and flexibility, and are great low-impact options. The key is finding activities you enjoy and can sustain over time.
Recommended Frequency and Duration of Exercise
The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity per week, or 75 minutes of vigorous-intensity aerobic activity, along with strength training exercises at least twice a week. These guidelines are general recommendations and should be adapted based on individual needs and abilities. It’s crucial to start slowly and gradually increase the intensity and duration of your workouts.
Consulting with a healthcare professional is essential to develop a personalized exercise plan that suits your specific needs and medical condition.
Relationship Between Physical Activity and Diabetic Retinopathy Risk
Regular exercise plays a vital role in reducing the risk of diabetic retinopathy. By improving blood sugar control and overall cardiovascular health, exercise helps protect the delicate blood vessels in the eyes. Reduced blood pressure and improved blood flow also contribute to decreased risk. In fact, research consistently shows a strong correlation between increased physical activity and a lower risk of developing or progressing diabetic retinopathy.
Following 8 tips for diabetic retinopathy prevention is crucial. Maintaining a healthy red blood cell rbc count red blood cell rbc count is a key component of overall well-being, and can indirectly impact the health of your eyes. This, in turn, supports the overall success of those 8 prevention tips, keeping your eyes healthy and reducing the risk of diabetic retinopathy.
This is a testament to the profound impact of exercise on eye health in the context of diabetes management.
Exercise Types, Benefits, and Precautions
| Exercise Type | Benefits | Precautions | Example Activities |
|---|---|---|---|
| Aerobic Exercise | Improves cardiovascular health, lowers blood sugar, and boosts insulin sensitivity. | Consult with your doctor before starting any vigorous aerobic exercise, especially if you have pre-existing heart conditions. Start slowly and gradually increase intensity. | Brisk walking, jogging, swimming, cycling, dancing |
| Strength Training | Builds muscle mass, improves metabolism, and enhances blood sugar control. | Proper form is crucial to avoid injuries. Start with lighter weights and gradually increase the load. Consult with a physical therapist or certified personal trainer to learn proper techniques. | Lifting weights, using resistance bands, bodyweight exercises |
| Yoga and Tai Chi | Improves balance, flexibility, and stress management, which can positively impact blood sugar control. | Listen to your body and modify poses as needed. Consult a qualified instructor to learn proper techniques. | Yoga classes, tai chi classes |
| Walking | A low-impact, accessible exercise that can be easily incorporated into daily life. Excellent for improving cardiovascular health and managing blood sugar. | Ensure you maintain a comfortable pace. Monitor your blood sugar levels before, during, and after walking. Listen to your body. | Walking around your neighborhood, brisk walking on a treadmill. |
Healthy Blood Pressure Management
High blood pressure, or hypertension, is a significant risk factor for developing diabetic retinopathy. It damages the tiny blood vessels in the retina, the light-sensitive tissue at the back of the eye. This damage can lead to blurred vision, vision loss, and even blindness over time. Effectively managing blood pressure is crucial for preventing and slowing the progression of diabetic retinopathy.
The Correlation Between High Blood Pressure and Diabetic Retinopathy
High blood pressure puts extra strain on the blood vessels throughout the body, including those in the retina. This strain can lead to damage, leakage, and narrowing of these delicate blood vessels. Over time, this damage can result in the formation of abnormal blood vessels (neovascularization) and scarring in the retina. These complications are directly associated with the development and progression of diabetic retinopathy.
Patients with diabetes and high blood pressure are at an increased risk of developing severe forms of retinopathy, requiring more aggressive treatment.
Strategies for Managing Blood Pressure
Effective blood pressure management involves a multifaceted approach that combines lifestyle changes and, when necessary, medication. A cornerstone of this approach is adhering to a healthy diet low in sodium and saturated fats. Regular physical activity, such as brisk walking, swimming, or cycling, helps lower blood pressure and improve overall health. Stress management techniques, such as meditation, yoga, or deep breathing exercises, can also play a significant role.
Limiting alcohol intake and avoiding smoking are equally important.
Importance of Regular Blood Pressure Checks
Regular blood pressure monitoring is essential for detecting and managing high blood pressure early. Early detection allows for timely intervention and helps prevent the development of diabetic retinopathy. The frequency of checks should be determined by your healthcare provider based on your individual risk factors and the severity of your diabetes. Frequent monitoring allows for adjustments to treatment plans, if needed.
Consistent tracking enables healthcare providers to identify trends and ensure optimal blood pressure control.
Blood Pressure Monitoring Methods, Target Ranges, and Consequences of Uncontrolled Blood Pressure
| Monitoring Method | Target Range (mmHg) | Consequences of Uncontrolled Blood Pressure | Additional Notes |
|---|---|---|---|
| Home Blood Pressure Monitoring | Systolic <130, Diastolic <80 | Increased risk of heart attack, stroke, kidney failure, and vision loss. Damage to blood vessels in the retina is a major concern. | Requires proper technique and consistent use for accurate readings. |
| Clinic Blood Pressure Monitoring | Systolic <130, Diastolic <80 | High blood pressure can lead to complications such as heart failure, stroke, and kidney disease, along with diabetic retinopathy. | Usually conducted by trained healthcare professionals in a controlled environment. |
| 24-Hour Ambulatory Blood Pressure Monitoring | Systolic <125, Diastolic <75 | Chronic elevated blood pressure is a major risk factor for cardiovascular diseases and can exacerbate the complications of diabetes, including retinopathy. | Provides a comprehensive assessment of blood pressure fluctuations throughout the day and night. |
| Blood Pressure Cuff Measurements (in clinical setting) | Systolic <130, Diastolic <80 | Uncontrolled hypertension can cause significant damage to blood vessels throughout the body, leading to organ damage, including in the eyes. | Provides a snapshot of blood pressure at a specific point in time. |
Link Between Blood Pressure Medication and Retinopathy Risk
The appropriate blood pressure medication, prescribed by a doctor, is crucial for controlling blood pressure without increasing the risk of diabetic retinopathy. Careful consideration of the individual patient’s medical history and overall health is essential. Some medications may have potential side effects, and the choice of medication should be tailored to minimize these risks while effectively managing blood pressure.
It is important to adhere to the prescribed medication regimen and communicate any concerns to your healthcare provider.
Taking care of your eyes is crucial, especially if you have diabetes. Eight tips for preventing diabetic retinopathy are a great starting point, but sometimes other health concerns can overshadow the importance of proactive eye care. For example, understanding the progression of time to castration resistant prostate cancer and its related challenges can make it difficult to prioritize other health issues.
However, these eight tips for preventing diabetic retinopathy are still important to maintain good overall health and well-being.
Healthy Cholesterol Management
Maintaining healthy cholesterol levels is crucial for overall cardiovascular health, and it plays a significant role in preventing diabetic complications. High cholesterol can contribute to the narrowing of blood vessels, reducing blood flow to vital organs, including the retina. This is particularly important for individuals with diabetes, as they are at higher risk for developing cardiovascular diseases and diabetic retinopathy.
Understanding the connection between cholesterol and retinopathy is essential for effective prevention strategies.High cholesterol, particularly high levels of low-density lipoprotein (LDL) cholesterol, can contribute to the development of diabetic retinopathy. This is because the buildup of plaque in blood vessels, a direct consequence of high cholesterol, restricts blood flow to the delicate blood vessels in the retina. Over time, this reduced blood flow can lead to damage and potentially impair the function of the retinal cells.
Furthermore, the inflammatory response triggered by high cholesterol can exacerbate the existing damage to the blood vessels in individuals with diabetes.
Importance of Regular Cholesterol Checks
Regular cholesterol checks are essential for individuals with diabetes. These checks allow healthcare professionals to monitor cholesterol levels and identify any potential risks early on. By identifying elevated cholesterol levels in a timely manner, preventative measures can be implemented to mitigate the potential harm to the retina and overall health. Early detection enables the initiation of lifestyle changes or medication, thus potentially slowing the progression of retinopathy.
Taking care of your eyes is crucial, especially if you have diabetes. 8 tips for diabetic retinopathy prevention are a great place to start, focusing on healthy habits like regular check-ups. While we’re on the subject of eye health, did you know that your visit to a dermatologist for atopic dermatitis can also offer valuable insights? For instance, your visit atopic dermatitis could shed light on the importance of managing skin conditions that often mirror similar systemic concerns.
Ultimately, understanding your body’s signals and implementing these 8 tips for diabetic retinopathy prevention are key to proactive well-being.
Connection Between High Cholesterol and Diabetic Retinopathy
High cholesterol levels are linked to an increased risk of diabetic retinopathy. The reduced blood flow caused by plaque buildup in the blood vessels of the retina can lead to damage and potentially impaired function of retinal cells. This impairment can manifest as blurred vision, vision loss, or other visual disturbances. Individuals with diabetes and high cholesterol are at a higher risk of experiencing more severe retinopathy.
Cholesterol-Lowering Medications and Retinopathy Risk
While cholesterol-lowering medications can effectively manage cholesterol levels, it’s crucial to understand their potential impact on retinopathy risk. These medications, such as statins, can have a positive impact on preventing cardiovascular disease, which, in turn, may help reduce the risk of diabetic retinopathy. However, individual responses to medications vary, and it’s essential to discuss any concerns about medication side effects with a healthcare professional.
Research suggests that these medications may help prevent or slow the progression of retinopathy by addressing the underlying cause, such as high cholesterol.
Cholesterol-Lowering Foods
A healthy diet rich in cholesterol-lowering foods can contribute to maintaining optimal cholesterol levels. These foods provide essential nutrients and can support overall health. The following table Artikels various cholesterol-lowering foods, their potential benefits, and precautions to consider.
| Food | Benefits | Precautions | Additional Notes |
|---|---|---|---|
| Oats | High in soluble fiber, which helps lower LDL cholesterol. | May cause digestive issues in some individuals. | Consider incorporating oats into your breakfast routine. |
| Fatty Fish (Salmon, Tuna) | Rich in omega-3 fatty acids, which help reduce triglycerides and raise HDL cholesterol. | May interact with certain medications. | Choose leaner cuts and limit portion sizes to manage calorie intake. |
| Fruits and Vegetables | Provide essential vitamins, minerals, and fiber, contributing to overall health. | May contain small amounts of cholesterol, but in insignificant amounts. | Aim for a variety of colorful fruits and vegetables. |
| Legumes | High in fiber, helping lower LDL cholesterol. | May cause digestive discomfort in some individuals. | Include legumes in your diet as part of a balanced meal plan. |
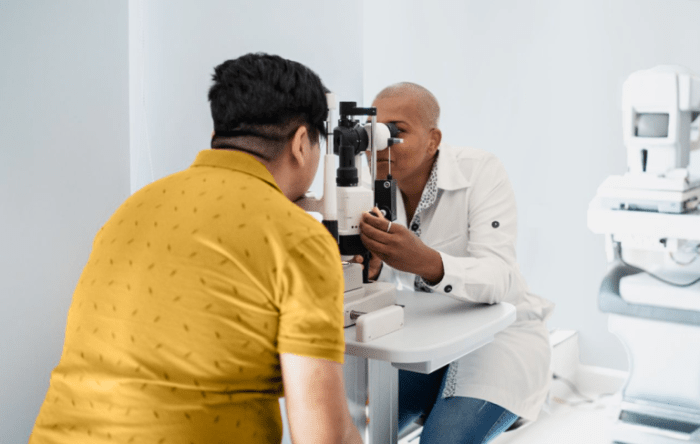
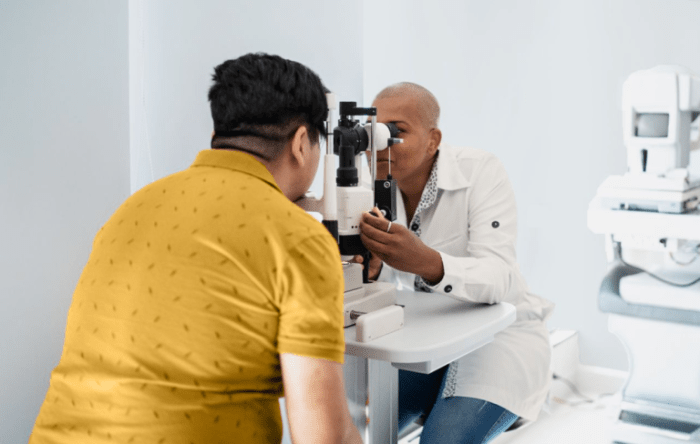
Regular Eye Exams
Regular eye exams are crucial for people with diabetes, as they can detect diabetic retinopathy early. Early detection significantly improves the chances of preventing vision loss and managing the condition effectively. Proactive eye care is a cornerstone of managing diabetes and preserving sight.Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye.
If left untreated, it can lead to vision impairment or blindness. Early detection through routine eye exams allows for timely intervention and treatment, often preventing serious vision loss.
Significance of Routine Eye Exams
Early detection of diabetic retinopathy is paramount in preventing vision loss. Regular eye exams, specifically designed for diabetics, allow ophthalmologists to identify any changes in the retina, even before noticeable symptoms appear. This proactive approach is vital in preserving vision and maintaining overall eye health.
Types of Eye Exams Recommended for Diabetics
Diabetics require specialized eye exams that go beyond routine vision screenings. Comprehensive dilated eye exams are essential. During these exams, eye drops are used to dilate the pupils, allowing the ophthalmologist to thoroughly examine the retina and the blood vessels within. This detailed view is critical in detecting any signs of retinopathy, such as microaneurysms, hemorrhages, or neovascularization.
Additional tests, such as optical coherence tomography (OCT), may be employed to obtain a more detailed three-dimensional view of the retina.
Frequency of Eye Exams for Diabetics
The frequency of eye exams for diabetics varies depending on the stage of diabetes and the presence or absence of retinopathy. Individuals with newly diagnosed diabetes or those with no signs of retinopathy may need eye exams every year. However, those with pre-existing retinopathy or a history of poor blood sugar control may require more frequent exams, potentially every 3-6 months, to monitor the progression of the condition.
A healthcare professional can determine the appropriate frequency based on individual needs.
Role of Early Detection in Preventing Vision Loss
Early detection of diabetic retinopathy is crucial to slowing or halting its progression. Treatment options, such as laser surgery or injections, can be employed to manage the condition effectively when caught early. These interventions can significantly reduce the risk of vision loss and improve the overall quality of life for individuals with diabetes.
Summary of Eye Exam Types
| Exam Type | Frequency | Importance in Detecting Retinopathy | Example |
|---|---|---|---|
| Comprehensive Dilated Eye Exam | Annually (or more frequently if needed) | Allows visualization of the retina and blood vessels for early detection of changes like microaneurysms and hemorrhages. | Ophthalmologist examines the retina under magnification, checking for abnormalities. |
| Optical Coherence Tomography (OCT) | As needed, especially if diabetic retinopathy is suspected. | Provides a detailed, three-dimensional image of the retina, enabling precise evaluation of retinal thickness and blood vessel health. | OCT scans can detect subtle changes that may not be apparent in a regular dilated exam. |
| Fundus Photography | Part of the dilated eye exam | Captures images of the retina, which can be compared to previous images to monitor changes over time. | Images of the retina are documented for comparison during future visits. |
| Visual Acuity Test | Part of the dilated eye exam | Assesses the clarity of vision, providing a measure of the overall health of the eye and potential impact of retinopathy. | Evaluates the sharpness of vision, and any changes. |
Avoiding Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption are detrimental habits that significantly impact overall health, including eye health. These habits can exacerbate existing conditions like diabetes and increase the risk of developing complications, particularly in the delicate structures of the eyes. Understanding the negative effects of these habits on diabetic retinopathy prevention is crucial for managing the condition effectively.Smoking, in particular, damages blood vessels throughout the body, including those in the eyes.
This damage can lead to impaired blood flow and oxygen delivery, increasing the risk of complications like diabetic retinopathy. Excessive alcohol consumption further complicates matters by disrupting blood sugar control, adding another layer of risk to eye health. By avoiding these habits, individuals with diabetes can significantly reduce the likelihood of developing or worsening diabetic retinopathy.
Harmful Effects of Smoking on Eye Health
Smoking constricts blood vessels, reducing blood flow to the retina and optic nerve. This reduced oxygen supply can lead to damage and impaired function in these crucial eye structures. Nicotine in cigarettes also contributes to oxidative stress, which further damages the delicate tissues in the eye, potentially accelerating the progression of eye diseases. Smoking is a known risk factor for age-related macular degeneration, cataracts, and glaucoma, all of which can impact vision.
Link Between Smoking and Diabetic Retinopathy, 8 tips for diabetic retinopathy prevention
Smoking worsens the already compromised blood vessels in the eyes of individuals with diabetes. The combination of diabetes-induced vascular damage and the further constriction caused by smoking significantly increases the risk of developing diabetic retinopathy and its severe complications. Research has shown a strong correlation between smoking and the progression of diabetic retinopathy, highlighting the importance of quitting smoking for those with diabetes.
Impact of Excessive Alcohol Consumption on Blood Sugar Control and Eye Health
Excessive alcohol consumption disrupts the body’s natural blood sugar regulation mechanisms. This disruption can lead to unpredictable fluctuations in blood sugar levels, making it harder to maintain optimal levels. Chronic alcohol use can also contribute to nutrient deficiencies, which can negatively impact overall health, including eye health. The combination of these factors can increase the risk of diabetic retinopathy.
In some cases, alcohol use can trigger acute episodes of elevated blood sugar, placing additional stress on the eyes.
Importance of Avoiding Smoking and Excessive Alcohol for Preventing Retinopathy
Maintaining a healthy lifestyle is crucial for preventing the progression of diabetic retinopathy. Avoiding smoking and excessive alcohol consumption are vital components of this strategy. Quitting smoking and limiting alcohol intake can significantly reduce the risk of developing or worsening diabetic retinopathy. This proactive approach to lifestyle management can help preserve vision and overall health.
Summary Table: Negative Impacts of Smoking and Excessive Alcohol
| Habit | Impact on Eye Health | Impact on Blood Sugar Control | Overall Effect on Retinopathy Prevention |
|---|---|---|---|
| Smoking | Reduced blood flow to retina and optic nerve, oxidative stress, increased risk of age-related macular degeneration, cataracts, and glaucoma. | Smoking can indirectly affect blood sugar control by potentially increasing insulin resistance and making blood sugar management more challenging. | Smoking significantly increases the risk of developing or worsening diabetic retinopathy. |
| Excessive Alcohol Consumption | Disrupts blood sugar control, potentially contributing to acute episodes of elevated blood sugar, increasing stress on the eyes. | Disrupts blood sugar regulation, potentially leading to unpredictable fluctuations in blood sugar levels, making it harder to maintain optimal blood sugar levels. | Excessive alcohol consumption can increase the risk of developing or worsening diabetic retinopathy by affecting blood sugar control and eye health. |
Last Point
In conclusion, preventing diabetic retinopathy is a journey that requires commitment to a holistic approach. By incorporating these eight tips into your daily routine, you can significantly reduce your risk of developing this sight-threatening condition. Remember, proactive care is crucial in preserving your vision for years to come. Understanding the link between diabetes management and eye health is the first step towards a brighter future.