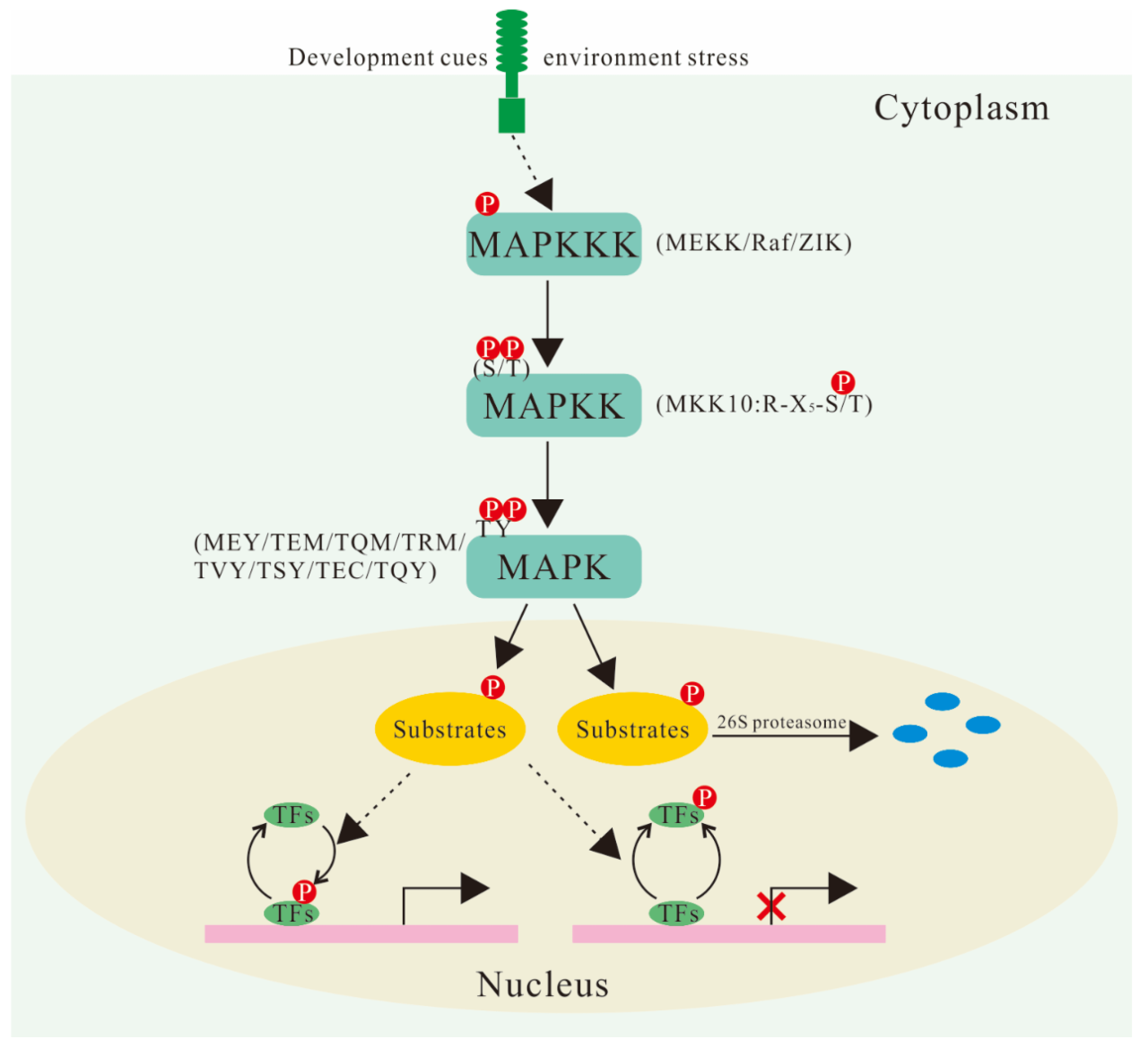
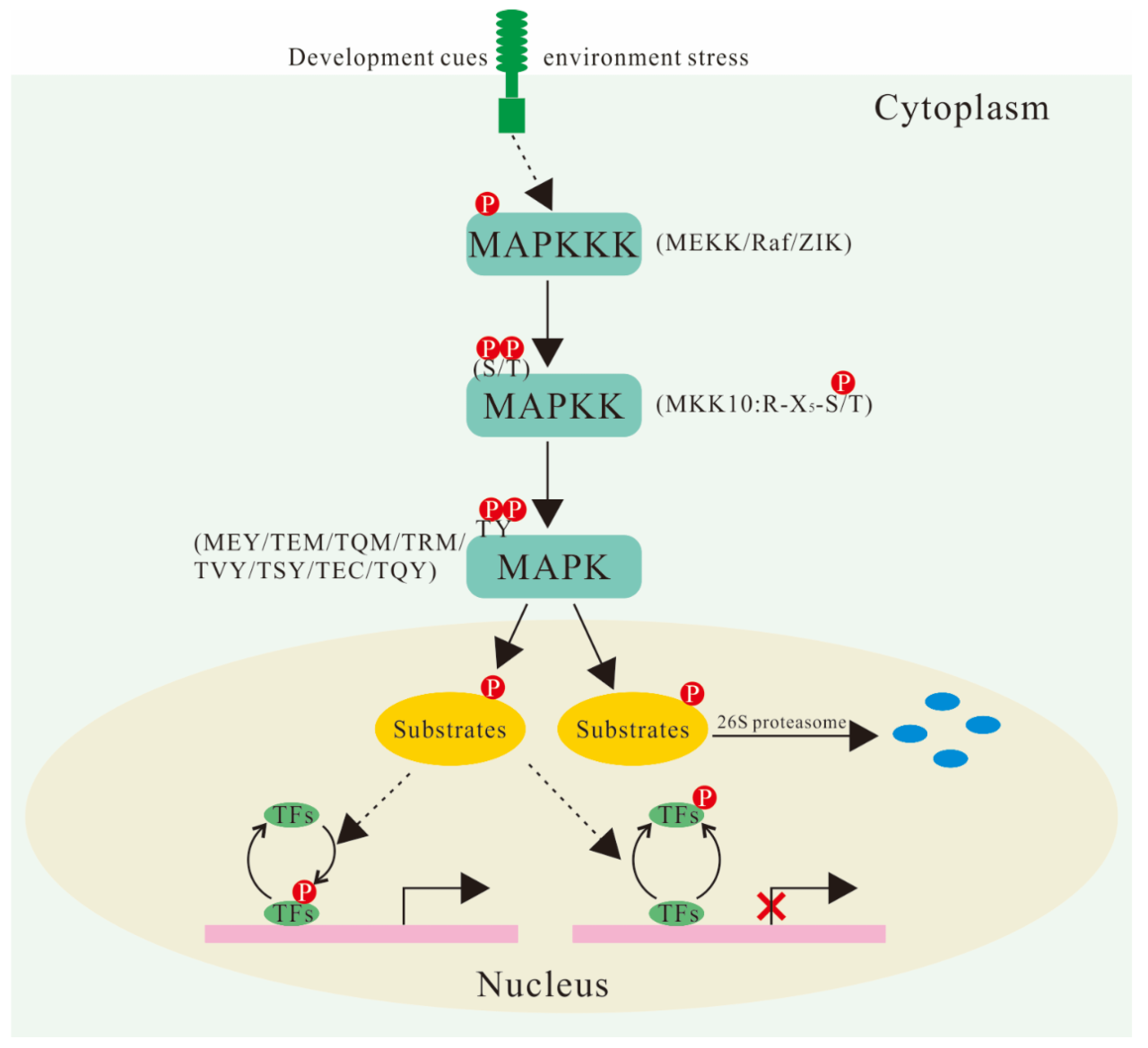
Home remedies for dry scalp offer a natural approach to combating this common scalp issue. From the simple act of incorporating moisturizing ingredients into your routine to creating soothing scalp masks, these methods can provide relief and promote healthy scalp hydration. This guide delves into the causes, ingredients, recipes, application, precautions, and examples related to treating dry scalp naturally.
Understanding the root causes of dry scalp is crucial for effective treatment. Environmental factors, lifestyle choices, and even underlying medical conditions can contribute to dryness. This exploration will cover a range of potential triggers and provide insights into how to identify and address them.
Understanding Dry Scalp: Home Remedies For Dry Scalp
A dry scalp, a common condition affecting people of all ages, is more than just a feeling of tightness or flakiness. It can lead to discomfort, itchiness, and even damage to the scalp’s protective barrier. Understanding the underlying causes and symptoms is crucial for effective management and treatment.Dry scalp is characterized by a lack of sufficient sebum production, the natural oil produced by the scalp.
This oil plays a vital role in keeping the scalp and hair hydrated, preventing dryness, and protecting against environmental factors. When sebum production is insufficient, the scalp loses its natural moisture barrier, leading to various symptoms and potentially more serious conditions.
Causes of Dry Scalp
Dry scalp can stem from a multitude of factors, ranging from environmental influences to lifestyle choices and even underlying medical conditions. Identifying the root cause is often the first step in developing a personalized treatment plan.
Trying to combat a dry scalp? Home remedies are a great place to start, but sometimes, even the best home remedies can’t combat everything. While you’re focusing on your scalp health, it’s important to be aware of the potential for common infections that happen in the hospital, like those contracted during a stay. So, whether you’re opting for natural oils or other home remedies, remember to prioritize your overall health and well-being.
A healthy scalp is key to overall well-being!
- Environmental Factors: Harsh weather conditions, like extreme heat or cold, or dry indoor environments, can strip the scalp of its natural moisture. Prolonged exposure to these conditions can disrupt the scalp’s oil production, leading to dryness. Frequent use of harsh shampoos, which strip away natural oils, can also exacerbate dry scalp.
- Lifestyle Factors: Certain lifestyle choices, such as frequent use of hair dryers, especially at high heat settings, or the frequent use of harsh hair styling products, can contribute to dry scalp. Stress and poor diet can also impact the scalp’s overall health and oil production. Dehydration, for instance, can affect the body’s ability to produce sufficient sebum.
- Medical Conditions: In some cases, dry scalp can be a symptom of an underlying medical condition, such as an autoimmune disorder, eczema, or psoriasis. These conditions can disrupt the scalp’s natural oil production and lead to inflammation, which can exacerbate dryness. Hypothyroidism, for example, can sometimes lead to decreased sebum production.
Symptoms Beyond Dryness
Dry scalp often presents itself with more than just dryness. Other common symptoms can include itching, flaking, redness, and even scaling. These symptoms can vary in severity and can affect different individuals differently.
- Itching: The scalp’s natural moisture barrier being compromised often results in itching as the scalp tries to repair itself. This itching can range from mild discomfort to intense irritation. Scratching the scalp can worsen the condition and lead to further inflammation and damage.
- Flaking: Dryness on the scalp leads to the formation of flakes, often appearing as white or yellowish scales. These flakes can be visible on the scalp itself and can also fall onto the hair.
- Redness: The scalp’s inflammatory response to dryness often manifests as redness, which can range from subtle pinkness to more pronounced redness and inflammation. This redness can indicate irritation and inflammation that require attention.
Types of Dry Scalp Conditions
Different types of dry scalp conditions exist, each with its own set of characteristics. While the underlying mechanisms are similar, the specific symptoms and severity can vary considerably.
- Seborrheic Dermatitis: This condition is characterized by inflamed, red patches on the scalp, often accompanied by greasy scales and yellow-brown flakes. Seborrheic dermatitis is more common than other types of dry scalp and frequently involves the scalp’s sebaceous glands, which produce sebum. It is crucial to distinguish between seborrheic dermatitis and other dry scalp conditions, as the treatment approaches may differ.
- Eczema: Eczema can manifest on the scalp, leading to dryness, itching, and redness. The symptoms of scalp eczema can be similar to other dry scalp conditions but may also present with distinct characteristics, such as persistent inflammation and the potential for weeping or crusting.
Scalp Hydration and Overall Health
Adequate hydration of the scalp is essential for maintaining its overall health. The scalp, like the rest of the body, requires sufficient moisture to function properly. This moisture helps maintain the scalp’s natural protective barrier and prevents the development of various problems.
- Maintaining Moisture: The scalp’s moisture balance is directly related to the overall health of the hair. Adequate hydration ensures that the scalp’s protective barrier functions effectively, preventing moisture loss and maintaining a healthy scalp environment. This hydration is essential for hair growth and overall scalp health.
Home Remedy Ingredients

So, you’ve learned about the causes and characteristics of dry scalp, now let’s delve into the world of home remedies. Using natural ingredients from your kitchen can often provide a soothing and effective solution. However, it’s crucial to remember that these remedies are not always scientifically proven and individual results may vary. Always consult a dermatologist if your dry scalp persists or worsens.
Common Kitchen Ingredients
Many common kitchen ingredients are touted for their moisturizing and soothing properties. These ingredients can be easily incorporated into your hair care routine, offering a potentially affordable and accessible solution.
- Olive Oil: Olive oil is a popular choice for its moisturizing qualities. Its rich fatty acid content helps to hydrate the scalp and restore moisture balance. Many people report positive experiences with olive oil, finding it to be an effective remedy for dry scalp.
- Coconut Oil: Similar to olive oil, coconut oil is another popular choice for its moisturizing benefits. Its saturated fatty acids are known to penetrate the scalp and hair, effectively locking in moisture. Some users find coconut oil to be particularly beneficial for managing dry scalp, although individual experiences may differ.
- Aloe Vera: Aloe vera gel, derived from the aloe vera plant, is renowned for its soothing and moisturizing properties. The gel can help calm irritated scalps and provide hydration, potentially relieving dryness and itchiness. Anecdotal evidence suggests that aloe vera can be a helpful addition to a dry scalp regimen.
- Yogurt: Yogurt, particularly plain yogurt, is often used for its lactic acid content. This acid can help exfoliate the scalp, removing dead skin cells that can contribute to dryness. The moisturizing properties of yogurt can also help soothe the scalp and provide hydration. While not widely studied, some individuals report improved scalp health using yogurt.
Effectiveness Comparison
Unfortunately, rigorous scientific studies directly comparing the effectiveness of different home remedies for dry scalp are limited. While anecdotal evidence suggests positive results for many, more controlled research is needed to establish conclusive findings. The effectiveness of any home remedy often depends on individual factors like scalp type and the severity of the dryness.
Potential Risks and Side Effects
While generally considered safe, some home remedies might cause allergic reactions or other side effects in susceptible individuals. For example, some people may experience skin irritation or an allergic reaction to certain ingredients, particularly if they have pre-existing skin conditions. Always perform a patch test before applying any home remedy to a larger area of the scalp.
Ingredients to Avoid
Certain ingredients should be avoided when creating home remedies for dry scalp, especially if you have sensitive skin. These include ingredients known to trigger allergic reactions or cause irritation.
- Harsh Chemicals: Avoid using strong chemicals or harsh detergents, as these can strip the scalp of its natural oils, worsening dryness.
- Fragrances: Fragrances in certain products can be irritating to sensitive skin, potentially leading to an allergic reaction or inflammation on the scalp.
- Strong Essential Oils: While some essential oils have purported benefits, using high concentrations of strong essential oils on the scalp without proper dilution can cause irritation or allergic reactions. Always dilute essential oils with a carrier oil before topical application.
Ingredient Properties Table
This table summarizes the properties of common home remedy ingredients for dry scalp.
Home Remedy Recipes

Discovering effective home remedies for dry scalp can be a rewarding journey. By understanding the root causes of your dry scalp and employing natural ingredients, you can create personalized solutions to soothe and nourish your scalp. These recipes provide a variety of options to address different dryness levels and potential underlying conditions.
Home Remedy Recipes for Dry Scalp, Home remedies for dry scalp
A variety of natural ingredients can effectively moisturize and nourish the scalp, alleviating dryness and itchiness. These recipes are designed to be easily prepared and applied at home, providing a cost-effective and convenient approach to scalp care.
| Recipe | Ingredients | Preparation | Application |
|---|---|---|---|
| Coconut Oil Treatment | 1 tablespoon coconut oil, 1 teaspoon honey | Melt coconut oil in a small bowl over simmering water or in the microwave. Mix in honey. | Apply a small amount of the mixture to your scalp, focusing on dry areas. Gently massage into the scalp for 2-3 minutes. Cover with a shower cap and leave on for 30 minutes. Rinse thoroughly with lukewarm water and a mild shampoo. |
| Aloe Vera and Yogurt Mask | 1/2 cup plain yogurt, 1 tablespoon aloe vera gel | Combine yogurt and aloe vera gel in a small bowl. Mix well until smooth. | Apply the mixture to your scalp, avoiding the hair. Massage gently into the scalp for 5 minutes. Cover with a shower cap and leave on for 15-20 minutes. Rinse thoroughly with lukewarm water and a mild shampoo. |
| Olive Oil and Lemon Juice Rinse | 2 tablespoons olive oil, 1 tablespoon lemon juice | Warm olive oil gently in a small bowl. Add lemon juice and mix well. | Apply the mixture to your scalp and hair, ensuring even distribution. Gently massage into the scalp for 2-3 minutes. Leave it on for 15 minutes, then rinse thoroughly with lukewarm water and a mild shampoo. Be cautious, as lemon juice can lighten hair color. |
| Apple Cider Vinegar Rinse | 1/4 cup apple cider vinegar, 1 cup water | Mix apple cider vinegar with water in a bowl. | Pour the mixture over your scalp after shampooing. Gently massage into the scalp for 1-2 minutes. Rinse thoroughly with lukewarm water. ACV can be drying, so use it sparingly and monitor for reactions. |
| Avocado and Olive Oil Hair Mask | 1/4 avocado, 1 tablespoon olive oil | Mash the avocado and mix it with the olive oil until smooth. | Apply the mixture to your scalp and hair, focusing on dry areas. Gently massage into the scalp for 5 minutes. Leave on for 30 minutes. Rinse thoroughly with lukewarm water and a mild shampoo. |
Important Considerations
Always test any new home remedy on a small, inconspicuous area of your scalp first to check for any allergic reactions. If you experience any irritation or discomfort, discontinue use immediately. Consistency is key to achieving positive results.
Applying Home Remedies
Getting rid of a dry scalp often requires a consistent approach. Applying home remedies correctly is key to achieving noticeable results. This section details the optimal frequency, various application methods, potential pitfalls to avoid, and safe storage practices. Understanding these aspects will help you maximize the effectiveness of your chosen remedies and minimize any potential issues.
Optimal Frequency for Application
The frequency of applying home remedies depends on the severity of your dry scalp and the specific remedy. Generally, applying remedies 1-2 times per week is a good starting point. This allows your scalp to absorb the ingredients effectively without causing irritation or over-drying. For more intense treatments, such as those involving oil applications, a less frequent application schedule may be more suitable.
If you experience significant improvement, you can adjust the frequency accordingly. Listen to your scalp and adjust the schedule as needed.
Application Methods
Different remedies require different application methods for optimal results. Massage, rinsing, and topical application are common approaches.
- Massage: A gentle scalp massage can help to distribute the remedy evenly and stimulate blood circulation. This can enhance the absorption of beneficial ingredients. Use a circular motion with your fingertips or a soft-bristled brush. Avoid using excessive pressure, which could irritate the scalp.
- Rinsing: Some remedies involve rinsing the mixture from the hair. This is typically done after the remedy has been applied and left on for a specific duration. Thorough rinsing is essential to avoid buildup and potential irritation.
- Topical Application: Many remedies are applied directly to the scalp. This may involve applying the mixture with your fingertips or using a cotton ball or cloth. Ensure even distribution to maximize the remedy’s effect.
Potential Mistakes to Avoid
Several mistakes can hinder the effectiveness of home remedies and even lead to scalp irritation.
- Using harsh ingredients: Avoid remedies containing ingredients that are known to be harsh or irritating. Always research the ingredients before using them.
- Over-applying: Applying too much of a remedy can be counterproductive and may cause irritation or buildup.
- Ignoring scalp sensitivity: If you notice any signs of irritation, discontinue use immediately. Your scalp may react differently to various remedies.
- Skipping patch testing: Always perform a patch test on a small area of the scalp before applying the remedy to the entire scalp. This helps to identify any potential allergic reactions.
Storing Home Remedies Safely
Proper storage is crucial to maintain the potency and safety of your home remedies.
- Refrigeration: Some remedies, particularly those containing ingredients that can spoil easily, should be stored in the refrigerator. This helps maintain their quality.
- Dark, cool place: Store remedies in a cool, dark place away from direct sunlight to preserve their effectiveness.
- Airtight containers: Use airtight containers to prevent the remedies from absorbing odors or moisture from the environment.
- Labeling: Label each container with the remedy’s name, ingredients, and date of preparation. This helps maintain clarity and traceability.
Importance of Patch Testing
Before applying any home remedy to your entire scalp, a patch test is essential. This preliminary test helps to identify potential allergic reactions or irritations that might arise from the remedy. Apply a small amount of the remedy to a discreet area of the scalp, such as behind the ear, and monitor it for 24-48 hours. Look for any signs of redness, swelling, itching, or other adverse reactions.
If you notice any signs of irritation, discontinue use and seek professional advice.
Application Method Comparison
Precautions and Considerations
Using home remedies for dry scalp can be a helpful approach, but it’s crucial to understand the potential risks and precautions involved. While many natural ingredients can soothe and moisturize, improper use or lack of consultation with a healthcare professional can exacerbate the problem. Always prioritize your well-being and safety.Proper guidance and understanding are essential to ensure home remedies are used effectively and safely.
Misusing or combining remedies with other medications can lead to unintended consequences. By recognizing potential triggers and understanding the differences between temporary and chronic conditions, you can better manage your dry scalp and make informed decisions about your treatment plan.
Consulting a Dermatologist
A dermatologist possesses specialized knowledge and expertise in diagnosing and treating various skin conditions, including dry scalp. Seeking professional advice is vital before starting any new treatment regimen, especially if the dryness is persistent or severe. They can accurately assess the cause of your dry scalp, rule out underlying medical conditions, and recommend the most suitable course of action, including home remedies if appropriate.
This proactive approach ensures the best possible outcome and prevents potential complications.
Ever tried soothing a dry scalp with some natural remedies? It’s amazing how many things you can do at home! Speaking of interesting bodily functions, have you ever wondered if your heart actually stops when you sneeze? Check out this fascinating article on does your heart stop when you sneeze to learn more about the science behind it.
Regardless of whether your heart pauses during a sneeze, a good home remedy for a dry scalp is using coconut oil as a mask, leaving it on for 20 minutes. It really works wonders!
Potential Interactions with Medications
Certain home remedies may interact with other medications you’re taking. For example, some essential oils, when applied topically, might react with certain medications, potentially affecting their absorption or efficacy. Always inform your doctor or pharmacist about any home remedies you plan to use, particularly if you are taking prescription medications. This communication is essential to avoid adverse reactions or complications.
Identifying Potential Triggers
Dry scalp can be triggered by a variety of factors. Understanding these triggers is crucial for managing the condition effectively. Some common culprits include harsh shampoos, excessive heat styling, environmental factors, and underlying medical conditions. Identifying and avoiding these triggers is a significant step in managing your dry scalp.
Managing Dry Scalp in Different Climates and Seasons
Different climates and seasons can influence the condition of your scalp. In dry climates, the scalp can become more susceptible to dryness. In contrast, humid environments can sometimes exacerbate the problem. Adjusting your skincare routine accordingly can help maintain scalp health throughout the year.
Temporary vs. Chronic Dry Scalp
Temporary dry scalp is often linked to environmental factors or changes in skincare routines. Symptoms typically resolve within a few weeks with appropriate care. Chronic dry scalp, however, persists despite treatment efforts and might indicate an underlying condition. In such cases, consulting a dermatologist is crucial to identify and address the root cause.
Finding the perfect home remedy for a dry scalp can be tricky, but often involves some simple ingredients you probably already have on hand. For example, applying a mixture of olive oil and honey can help soothe dryness. Interestingly, similar natural remedies are often used to relieve gas pains quickly, such as drinking chamomile tea or using peppermint oil.
Learning how to relieve gas pains fast can actually help with figuring out what natural remedies work best for your body, whether you’re looking to tackle a dry scalp or a variety of other minor ailments. So, if you’re looking for more ideas, check out this helpful guide on how to relieve gas pains fast for a broader understanding of natural remedies.
Ultimately, the best approach is to experiment and find what works best for your specific needs when dealing with dry scalp.
Potential Dry Scalp Triggers
Understanding the triggers behind your dry scalp can significantly improve your management strategy. A well-informed approach can empower you to make proactive decisions that address the root cause and lead to effective solutions.
| Trigger | Description | Impact |
|---|---|---|
| Harsh Shampoos | Shampoos containing sulfates or other harsh detergents can strip the scalp of its natural oils. | Increased dryness, irritation, and flaking. |
| Excessive Heat Styling | Frequent use of hot styling tools can damage the scalp’s protective barrier. | Increased dryness, irritation, and potential for hair damage. |
| Environmental Factors (e.g., dry air, cold weather) | Low humidity or extreme temperatures can dehydrate the scalp. | Increased dryness, flaking, and itching. |
| Underlying Medical Conditions | Certain medical conditions, such as eczema or psoriasis, can manifest as dry scalp. | Persistent dryness, scaling, and inflammation. |
| Certain Medications | Some medications can have a side effect of causing dry scalp. | Increased dryness and discomfort. |
Illustrative Examples
Home remedies for dry scalp can be effective, but their success depends on various factors. Understanding these factors, and the nuances of individual responses, helps us tailor approaches to maximize positive outcomes. Let’s examine some real-world scenarios to gain a clearer picture.
A Successful Home Remedy Scenario
Sarah, a 28-year-old woman, experienced persistent dry scalp, characterized by flaking and itching. She tried several commercial products without significant improvement. Inspired by online recommendations, she began using a mixture of coconut oil and aloe vera gel, massaging it into her scalp twice a week. Within a month, Sarah observed a noticeable reduction in flaking and itching.
The coconut oil’s moisturizing properties likely replenished the scalp’s natural oils, while the aloe vera’s soothing qualities calmed the irritation. The consistency of the mixture allowed for easy application and ensured thorough scalp penetration.
A Home Remedy That Didn’t Work
John, a 35-year-old man, tried a home remedy consisting of olive oil and honey. Despite applying it regularly, his dry scalp persisted. In this case, the remedy likely failed due to the combination’s incompatibility with his scalp type. Olive oil, while moisturizing, might have been too heavy for his scalp, potentially blocking pores and hindering natural oil production.
Alternatively, the honey might have exacerbated existing sensitivities.
Reasons for Success and Failure
The success or failure of a home remedy hinges on several key factors:
- Scalp type: Different scalp types react differently to various ingredients. Some might benefit from heavier oils, while others might find them clogging pores. Understanding one’s scalp type is crucial.
- Ingredient compatibility: Some ingredients, like honey or certain essential oils, can trigger allergic reactions or irritate sensitive scalps. A careful assessment of ingredient compatibility is essential.
- Consistency of application: Regular application is crucial for home remedies to work effectively. Irregular use can lead to inconsistent results or no improvement at all.
- Underlying conditions: Underlying medical conditions like seborrheic dermatitis can sometimes mimic dry scalp. In such cases, home remedies might not be sufficient and professional medical advice is necessary.
Hypothetical Case Study: Emily’s Dry Scalp Routine
Emily, a 20-year-old student with a dry scalp, experiences mild flaking and occasional itching. She can incorporate the following home remedy routine:
- Weekly Treatment: A mixture of 1 tablespoon of jojoba oil and 1 teaspoon of apple cider vinegar, massaged into the scalp for 10 minutes before shampooing. Jojoba oil’s similarity to scalp oils and apple cider vinegar’s mild exfoliating properties are expected to be beneficial.
- Daily Moisturizing: A small amount of shea butter can be applied to the scalp after shampooing to seal in moisture. This helps to lock in the hydration provided by the weekly treatment.
- Avoiding Irritants: Emily should avoid harsh shampoos and excessive heat styling, which can further dry out her scalp.
Illustrative Example: Making a Jojoba Oil and Apple Cider Vinegar Treatment
This recipe demonstrates the process of creating a home remedy for dry scalp using jojoba oil and apple cider vinegar.
| Step | Action |
|---|---|
| 1 | Gather ingredients: 1 tablespoon of jojoba oil and 1 teaspoon of apple cider vinegar. |
| 2 | Combine the ingredients in a small, clean container. |
| 3 | Mix gently until the ingredients are fully combined. |
| 4 | Apply the mixture to the scalp, avoiding the eyes. |
| 5 | Massage the mixture into the scalp for 10 minutes. |
| 6 | Rinse thoroughly with lukewarm water. |
| 7 | Follow with your regular shampoo. |
Ultimate Conclusion
In conclusion, embracing home remedies for dry scalp can be a valuable step towards achieving a healthier, more hydrated scalp. By understanding the causes, exploring various recipes, and carefully applying the remedies, you can take proactive steps to alleviate dryness and maintain a balanced scalp environment. Remember to consult a dermatologist for personalized advice, especially if the dryness persists or worsens.














![Differences between Dandruff and dry scalp [Explained] - Medical Darpan Dandruff vs dry scalp](https://healthandstyleplus.com/wp-content/uploads/2025/06/Dry-scalp-vs-dandruff-comparisson-1.jpg)