Wrist pain causes symptoms and treatments is a common complaint, affecting people of all ages. Understanding the various causes, symptoms, and available treatments can help you manage and potentially prevent wrist pain. This guide will delve into the complexities of wrist pain, exploring everything from overuse injuries to underlying medical conditions. We’ll cover everything from the initial symptoms to the different treatment options available, and even preventive measures you can take.
From sharp pains to dull aches, wrist pain can manifest in many ways. Different causes, from repetitive strain injuries to fractures, can lead to varying symptoms. This article aims to provide a comprehensive overview of wrist pain, covering the full spectrum of potential causes, symptoms, diagnoses, and treatments, to empower you to take control of your wrist health.
Introduction to Wrist Pain
Wrist pain is a common complaint affecting individuals of all ages and activity levels. It can range from mild discomfort to severe, debilitating agony, significantly impacting daily life. Understanding the various causes, types, and potential symptoms is crucial for effective self-management and seeking appropriate medical attention.Wrist pain arises from a multitude of factors, including repetitive strain, acute injuries, and underlying medical conditions.
The nature of the pain, its location, and associated symptoms can provide valuable clues to its origin and severity. Recognizing these nuances is essential for initiating an informed approach to diagnosis and treatment.
Common Causes of Wrist Pain
Understanding the root causes of wrist pain is essential for appropriate management. Common culprits include repetitive strain injuries from activities like typing, using a computer mouse, or playing certain sports. Acute injuries such as fractures, sprains, and dislocations are also potential sources of wrist pain. Underlying medical conditions like arthritis, carpal tunnel syndrome, and tendonitis can also lead to persistent wrist discomfort.
Identifying the specific cause often helps guide effective treatment strategies.
Types of Wrist Pain
Wrist pain manifests in diverse ways, with varying intensities and characteristics. This variability is a key aspect in determining the underlying cause. The type of pain, whether sharp, dull, or aching, provides valuable diagnostic information. Sharp pain often suggests a sudden injury, while dull or aching pain may indicate chronic conditions or overuse.
Categorizing Wrist Pain
The table below provides a comparative overview of different types of wrist pain, highlighting potential symptoms, durations, and possible underlying causes.
| Type of Pain | Symptoms | Duration | Possible Causes |
|---|---|---|---|
| Sharp, stabbing pain | Sudden onset, intense, localized to a specific area, potentially accompanied by swelling or bruising. | Acute (hours to days), often related to a specific incident. | Fractures, sprains, dislocations, tendon tears, acute inflammation. |
| Dull, aching pain | Gradual onset, persistent, often felt throughout the wrist, may be accompanied by stiffness. | Chronic (weeks to months), often associated with repetitive strain or underlying conditions. | Arthritis, carpal tunnel syndrome, tendonitis, bursitis, osteoarthritis, nerve compression. |
| Burning pain | A sensation of warmth and tingling, often radiating to the fingers. | Variable, could be acute or chronic depending on the underlying cause. | Nerve entrapment, carpal tunnel syndrome, diabetes-related neuropathy. |
Causes of Wrist Pain
Wrist pain can be a debilitating issue, affecting daily activities and quality of life. Understanding the potential causes is crucial for effective diagnosis and treatment. From simple overuse to more serious conditions, a range of factors can contribute to wrist discomfort.Repetitive strain injuries are a common culprit, particularly in occupations or hobbies requiring repetitive hand and wrist movements.
These injuries often develop gradually, with pain initially mild and increasing over time. Think of someone who spends hours typing on a keyboard or someone who frequently uses a power tool.
Common Causes of Wrist Pain
Wrist pain can stem from a variety of sources, making accurate diagnosis essential. Understanding the different causes, including injuries and underlying medical conditions, is crucial for proper treatment.
- Repetitive Strain Injuries (RSIs): These injuries, often linked to prolonged, repetitive motions, cause inflammation and pain in the wrist and surrounding tissues. Examples include carpal tunnel syndrome, tendonitis, and tenosynovitis. They are frequently seen in professions requiring repetitive hand and wrist movements, like assembly line work or computer use.
- Sprains and Fractures: Wrist sprains occur when ligaments in the wrist are stretched or torn, often due to sudden twisting or impact. Fractures involve a break in one or more of the wrist bones, typically caused by a fall or direct blow. The severity of the injury determines the level of pain and disability.
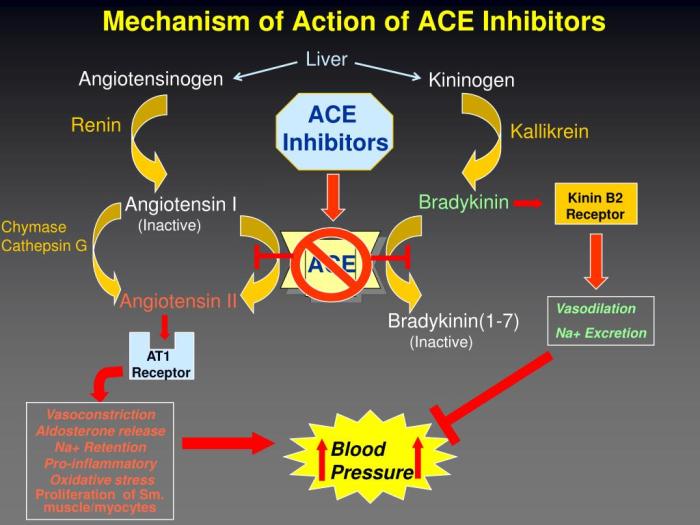
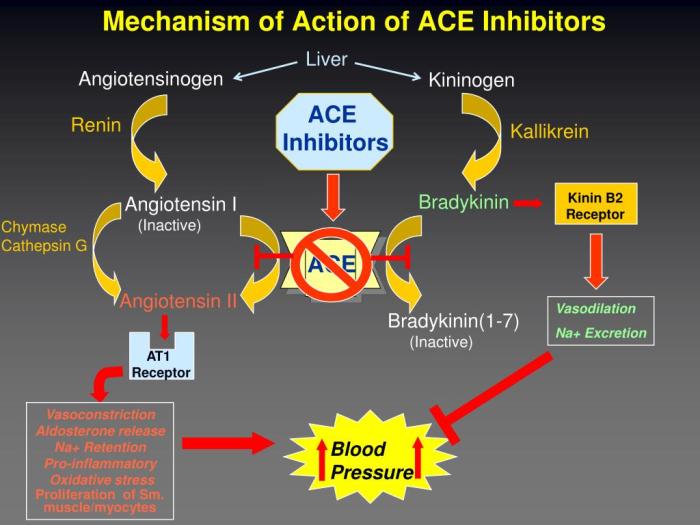
- Underlying Medical Conditions: Certain medical conditions can contribute to wrist pain, such as arthritis, carpal tunnel syndrome, and rheumatoid arthritis. Arthritis involves inflammation of the joints, causing pain, stiffness, and swelling. Carpal tunnel syndrome results from compression of the median nerve in the wrist, often causing numbness and tingling in the hand and fingers. Rheumatoid arthritis is an autoimmune disorder causing chronic inflammation of the joints, leading to significant wrist pain.
Wrist Pain in Different Age Groups
The causes of wrist pain can vary depending on the age group. Children and adolescents might experience growth-related issues or repetitive strain injuries from sports activities. Adults often face occupational hazards or injuries from falls or accidents. Older adults might experience arthritis or osteoporosis, which can increase the risk of fractures.
- Children and Adolescents: Wrist pain in this age group could be due to growth spurts, repetitive stress from sports, or overuse injuries. For example, a young tennis player might develop wrist pain from repetitive backhand motions.
- Adults: Wrist pain in adults is often linked to repetitive strain injuries from work or hobbies, falls, or car accidents. Examples include office workers developing carpal tunnel syndrome or construction workers sustaining fractures from workplace accidents.
- Older Adults: Wrist pain in older adults might be related to arthritis, osteoporosis, or fractures. Osteoporosis weakens bones, increasing the risk of fractures with even minor falls.
Symptoms and Potential Causes of Wrist Pain
A clear understanding of symptoms and their potential causes can aid in diagnosis.
| Symptoms | Potential Causes |
|---|---|
| Pain, tenderness, or swelling in the wrist | Sprains, fractures, arthritis, tendonitis |
| Numbness or tingling in the hand and fingers | Carpal tunnel syndrome, nerve compression |
| Stiffness or limited range of motion | Arthritis, tendonitis, fractures |
| Weakness in the hand or wrist | Nerve damage, fractures |
| Clicking or popping sounds in the wrist | Joint instability, tendon problems |
Symptoms of Wrist Pain

Wrist pain can be a frustrating experience, often making simple tasks feel challenging. Understanding the various symptoms associated with wrist pain is crucial for identifying the underlying cause and seeking appropriate treatment. Different causes of wrist pain can manifest with different symptoms, making a careful assessment essential. Knowing what to look for can significantly aid in determining the nature of the problem.Recognizing the symptoms of wrist pain is vital for effective diagnosis and treatment.
The location, intensity, and accompanying sensations of the pain can provide valuable clues to the potential cause. Furthermore, understanding how symptoms vary based on the cause of the pain is key to getting the right care.
Common Symptoms
Wrist pain can present in numerous ways, ranging from mild discomfort to severe agony. Common symptoms include pain, swelling, stiffness, numbness, and tingling. These symptoms can vary in intensity and duration, depending on the underlying cause.
Wrist pain can stem from various things, like overuse or injury. Understanding the causes, symptoms, and treatments is key. Sometimes, pain under the left rib cage might be related to similar underlying issues, as well. For more on that, check out this helpful article about pain under left rib cage. Ultimately, proper diagnosis and treatment for wrist pain often requires a visit to a doctor, especially if the pain persists or worsens.
- Pain: This is a frequent symptom, often described as a dull ache, sharp stabbing sensation, or a burning feeling. The pain can be localized to a specific area of the wrist or radiate to other parts of the hand or arm. The intensity of the pain can range from mild to severe, influencing daily activities.
- Swelling: Inflammation in the wrist joint often manifests as swelling, making the wrist appear larger than usual. This swelling can be accompanied by warmth and tenderness in the affected area. It can be a significant indicator of inflammation or injury.
- Stiffness: Reduced range of motion in the wrist is a common symptom. Stiffness can make simple movements, like bending or extending the wrist, difficult and painful. This can be a key indicator of conditions like arthritis.
- Numbness and Tingling: These sensations, often described as “pins and needles,” can occur in the wrist and radiating into the fingers. They frequently indicate nerve compression, such as carpal tunnel syndrome. The pattern of numbness and tingling can be helpful in diagnosing the specific nerve affected.
Location of Pain and Potential Causes
The precise location of the pain in the wrist can offer valuable insights into the potential cause. For instance, pain concentrated near the base of the thumb might suggest a problem with the thumb carpal bones or tendons. Conversely, pain on the outside of the wrist could point towards a problem with the wrist joint or associated ligaments.
Symptom Severity and Potential Causes
The severity of wrist pain symptoms can vary greatly. A mild ache might indicate a minor strain or overuse, while severe, sharp pain could signal a more serious condition like a fracture or dislocation.
Wrist pain can stem from various things, like overuse, injuries, or even arthritis. Understanding the causes and symptoms is key to finding the right treatment. Sometimes, a condition like rosacea, while primarily affecting the face, can manifest in unusual ways, such as with associated inflammation, which could potentially contribute to wrist pain. If you’re looking for options to manage rosacea, exploring different medication approaches can be helpful.
For example, checking out rosacea medication what are my options might provide some valuable insights. Ultimately, consulting a doctor is crucial for diagnosing the specific cause of your wrist pain and developing a personalized treatment plan.
| Symptom | Potential Causes | Severity Level |
|---|---|---|
| Mild aching pain | Overuse, strain, tendinitis | Low |
| Severe sharp pain, accompanied by swelling | Fracture, dislocation, severe sprain | High |
| Numbness and tingling in fingers | Carpal tunnel syndrome, nerve compression | Variable |
| Stiffness, limited range of motion | Arthritis, joint inflammation | Variable |
Diagnosing Wrist Pain: Wrist Pain Causes Symptoms And Treatments
Figuring out the source of wrist pain involves a systematic approach. It’s crucial to accurately pinpoint the underlying cause to develop an effective treatment plan. This process often combines a thorough medical history, a physical examination, and potentially various diagnostic tests.The diagnostic journey begins with understanding the patient’s complete medical history. This includes past injuries, existing medical conditions, and any recent activities that might have contributed to the pain.
Understanding the timeline of the pain, its location, and any associated symptoms can provide vital clues.
Medical History Assessment
A detailed medical history is essential to understanding the context of the wrist pain. Factors such as previous wrist injuries, repetitive strain, underlying medical conditions (like arthritis or osteoporosis), and medications taken can influence the diagnosis. The duration of the pain, its frequency, and any aggravating or relieving factors should also be meticulously documented.
Physical Examination
A comprehensive physical examination is a fundamental part of the diagnostic process. The physician will evaluate the range of motion in the wrist, assess for tenderness or swelling, and examine the surrounding tissues for any signs of inflammation or deformity. Palpation, or feeling with the hands, is often employed to identify specific areas of pain and potential sources of the discomfort.
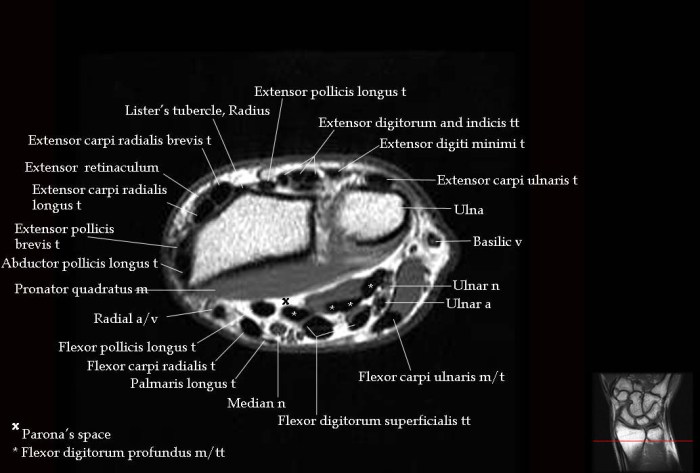
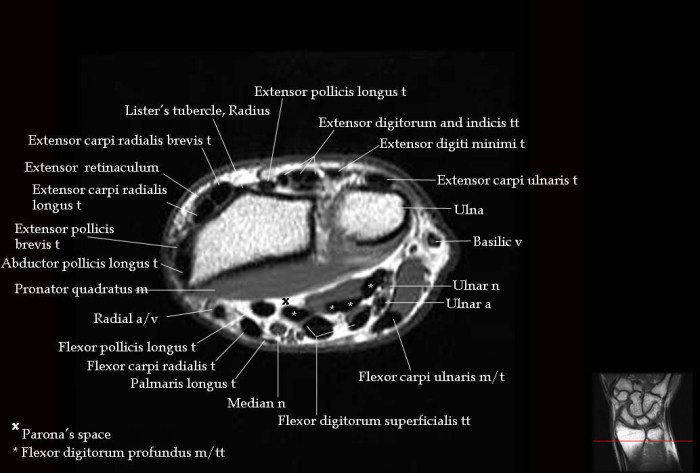
Diagnostic Imaging
Imaging techniques provide visual representations of the wrist’s internal structures, aiding in the identification of potential issues.
- X-rays: X-rays are commonly used to detect fractures, dislocations, or other bone abnormalities. They provide a two-dimensional view of the bones, highlighting any signs of damage or misalignment. For instance, a fractured radius might show up as a break in the bone on an X-ray.
- Magnetic Resonance Imaging (MRI): MRI scans offer a detailed view of soft tissues, including ligaments, tendons, and cartilage. They are particularly useful for identifying soft tissue injuries, such as tears or inflammation in these structures. A torn ligament in the wrist might be clearly visible on an MRI.
- Computed Tomography (CT) Scans: CT scans provide detailed cross-sectional images of the wrist, which can be beneficial in identifying complex fractures or bone lesions that might not be apparent on X-rays alone. They can also help evaluate the extent of damage in cases of severe trauma.
Diagnostic Tests
Beyond imaging, specific tests can help determine the precise nature of the wrist pain.
Wrist pain can stem from various issues, like repetitive strain or arthritis. Understanding the causes and symptoms is key to finding the right treatment. Sometimes, pain radiating from the shoulder, like in a slap tear of the shoulder , can mimic wrist pain. Proper diagnosis is crucial, and a doctor can help determine the underlying cause and recommend appropriate therapies to alleviate wrist pain.
- Blood Tests: Blood tests can be useful in ruling out conditions such as infections or inflammatory diseases that can manifest as wrist pain. Elevated inflammatory markers, for example, could indicate an underlying inflammatory condition.
- Nerve Conduction Studies: These studies evaluate the function of nerves in the wrist. They are helpful in identifying nerve compression or damage, which can cause pain and numbness in the wrist and hand. A nerve compression syndrome, like carpal tunnel syndrome, might be indicated by abnormal nerve conduction study results.
Diagnostic Summary, Wrist pain causes symptoms and treatments
The effectiveness of different diagnostic methods varies depending on the suspected cause of the wrist pain.
| Diagnostic Method | Effectiveness in Identifying Wrist Pain Causes |
|---|---|
| Medical History | High, providing crucial context and potential clues. |
| Physical Examination | High, allowing for direct assessment of the wrist’s condition. |
| X-rays | High for bone-related issues (fractures, dislocations). |
| MRI | High for soft tissue injuries (ligaments, tendons, cartilage). |
| CT Scans | High for complex bone injuries and trauma assessment. |
| Blood Tests | Moderate, helpful in ruling out systemic conditions. |
| Nerve Conduction Studies | High for nerve-related issues (e.g., carpal tunnel syndrome). |
Treatments for Wrist Pain
Dealing with wrist pain can be frustrating, impacting daily activities and overall well-being. Fortunately, various treatment options are available, ranging from simple home remedies to more involved surgical procedures. Understanding these options can help you make informed decisions about managing your wrist pain effectively.Effective wrist pain management often involves a combination of approaches. Conservative treatments, which prioritize non-surgical methods, are frequently the first line of defense.
These methods, including pain relievers and physical therapy, aim to alleviate symptoms and improve function without resorting to surgery. In some cases, however, surgical intervention may be necessary to address underlying structural issues or persistent pain.
Conservative Treatments
Conservative treatments for wrist pain emphasize non-surgical approaches. These methods aim to reduce pain, improve function, and promote healing. Common conservative options include pain relievers, physical therapy, and other non-surgical treatments.
- Pain Relievers: Over-the-counter pain relievers like ibuprofen or naproxen can help reduce inflammation and pain. Acetaminophen can also be effective in managing pain, although it doesn’t address inflammation. However, it’s crucial to follow dosage instructions carefully and consult a doctor if pain persists or worsens. For instance, a patient experiencing chronic wrist pain might benefit from long-term use of low-dose ibuprofen, but careful monitoring is essential to prevent potential side effects like stomach upset or kidney problems.
- Physical Therapy: Physical therapy plays a vital role in restoring wrist function and strength. Exercises and stretches prescribed by a physical therapist can improve range of motion, reduce stiffness, and strengthen the supporting muscles around the wrist. A tailored rehabilitation program, for example, might involve specific exercises for carpal tunnel syndrome to improve nerve function and reduce pressure on the median nerve.
- Other Non-Surgical Treatments: Other non-surgical treatments might include wrist splints or braces to immobilize the wrist and reduce strain. Rest is often crucial, allowing the injured tissues to heal properly. For instance, a wrist fracture may require a period of immobilization in a cast, followed by a physical therapy regimen to regain full range of motion and strength.
Surgical Treatments
Surgical intervention for wrist pain is considered when conservative treatments fail to provide adequate relief. Specific surgical procedures depend on the underlying cause of the pain.
- Surgical Procedures: Procedures for wrist pain can vary greatly, depending on the specific condition. Examples include carpal tunnel release surgery, which involves cutting the transverse carpal ligament to relieve pressure on the median nerve. Other procedures might involve addressing fractures, arthritis, or tendon tears. The decision to proceed with surgery is made on a case-by-case basis, considering factors such as the severity of the condition, the patient’s overall health, and the potential risks and benefits.
- Indications and Recovery Times: Surgery is typically recommended when pain is severe, persistent, and unresponsive to other treatments. Recovery times vary significantly depending on the specific procedure and the individual patient. For instance, a carpal tunnel release surgery typically involves a few days of recovery, with the ability to return to light activities within a week, but full recovery might take several months.
It’s crucial to follow post-operative instructions diligently to promote healing and prevent complications.
Alternative Therapies
Alternative therapies, such as acupuncture, massage therapy, and yoga, can complement conventional treatments. While these therapies might provide pain relief for some individuals, their effectiveness is not always supported by rigorous scientific evidence.
- Alternative Therapies for Wrist Pain Relief: While not a substitute for conventional medical care, some individuals find relief from wrist pain through alternative therapies. Acupuncture, for example, involves inserting thin needles into specific points on the body to stimulate energy flow. Massage therapy can help relax muscles and reduce tension. Yoga, with its focus on posture and flexibility, can contribute to improved wrist function and reduced pain.
However, it’s essential to discuss alternative therapies with your doctor to ensure they don’t interfere with your primary treatment plan.
Comparison of Treatment Options
| Treatment Option | Effectiveness | Potential Side Effects | Recovery Time |
|---|---|---|---|
| Pain Relievers | Moderate to High (depending on the cause) | Stomach upset, kidney problems (with prolonged use) | Immediate |
| Physical Therapy | High | Muscle soreness, minor discomfort during exercises | Variable (weeks to months) |
| Surgical Procedures | High (for specific conditions) | Infection, nerve damage, stiffness | Variable (weeks to months) |
| Alternative Therapies | Variable (limited scientific evidence) | Potential for adverse interactions with other medications | Variable (depends on the therapy) |
Prevention of Wrist Pain
Wrist pain, while often temporary, can significantly impact daily life. Understanding the factors that contribute to wrist pain and implementing preventive measures can significantly reduce the risk of developing these issues. Proactive strategies can prevent future problems and ensure continued comfort and functionality.Proper posture and ergonomic practices play a crucial role in preventing wrist pain. Maintaining a neutral wrist position during activities like typing, using a mouse, or holding a phone minimizes strain on the wrist joints.
Consistent awareness of posture, especially during prolonged tasks, is vital.
Proper Posture and Ergonomic Practices
Maintaining a neutral wrist position is essential to prevent strain. Avoid bending your wrists excessively when typing or using a mouse. Ensure your keyboard and mouse are at a comfortable height and distance to avoid awkward wrist positions. Using ergonomic tools, such as adjustable keyboards and wrist rests, can further support a healthy posture. Proper seating posture also influences wrist positioning.
Keep your elbows at a 90-degree angle and your wrists aligned with your forearms. These practices are key to preventing repetitive strain injuries (RSI).
Importance of Taking Breaks During Repetitive Tasks
Extended periods of repetitive motions can lead to wrist pain. Regular breaks during these tasks are crucial for allowing the muscles and tendons to recover. These breaks should involve gentle wrist stretches and movements to improve blood circulation and reduce stiffness. A short, 5-10 minute break every hour can dramatically decrease the likelihood of developing wrist pain.
Maintaining a Healthy Weight
Maintaining a healthy weight is a crucial aspect of overall health, including wrist health. Excessive weight can put additional stress on the joints, including the wrists. A balanced diet and regular exercise contribute to maintaining a healthy weight, thus reducing the risk of wrist pain.
Using Appropriate Equipment and Tools
Using appropriate equipment and tools is paramount in preventing wrist pain. Ensure that your tools and equipment are properly sized and designed for the task at hand. Tools that are too small or too large can force awkward wrist positions, increasing the risk of injury. Using appropriate tools reduces the strain on your wrists and minimizes the risk of pain.
Practical Tips for Preventing Wrist Pain in Daily Activities
Implementing these practical tips in your daily activities can significantly reduce the risk of wrist pain:
- Use wrist supports during prolonged activities like typing or writing. This provides extra cushioning and support, reducing strain.
- When lifting heavy objects, use your legs and core muscles instead of relying solely on your wrists. This distributes the load evenly, preventing wrist strain.
- Avoid twisting your wrists excessively during tasks like opening jars or tightening screws. Use proper techniques to avoid unnecessary wrist movement.
- Gradually increase the duration and intensity of activities that strain your wrists. This allows your muscles and tendons to adapt, preventing sudden injuries.
- Consider using ergonomic keyboards and mice to promote proper posture and reduce wrist strain during prolonged computer use.
Wrist Pain in Specific Populations
Wrist pain isn’t just a universal experience; its presentation and underlying causes can vary significantly depending on the individual’s age and developmental stage. Understanding these age-related differences is crucial for accurate diagnosis and effective treatment. This section delves into the specific considerations for wrist pain in children, adolescents, and older adults, highlighting common conditions and the impact of age on the healing process.
Wrist Pain in Children
Children’s wrists are still developing, making them susceptible to different types of injuries than adults. Growth spurts, repetitive activities, and falls can all contribute to wrist pain in children. Understanding the developmental stage is vital for proper diagnosis and treatment.
- Growth Plates: Children’s bones have growth plates, areas of cartilage that are weaker than the surrounding bone. These growth plates are susceptible to fractures, particularly in younger children. These fractures, often called “growth plate fractures” or “epiphyseal fractures,” can cause significant pain and require careful management to avoid long-term complications.
- Repetitive Strain Injuries: Activities like playing sports or engaging in repetitive hand movements, such as drawing or writing, can lead to wrist pain in children, particularly in those with poor posture or repetitive hand movements.
- Infections: Infections can sometimes affect the wrist, causing pain and swelling. This is less common than other causes, but it’s crucial to consider in cases where other symptoms, such as fever, are present.
Wrist Pain in Adolescents
Adolescents experience rapid physical changes that can impact wrist health. The combination of growth spurts, increased physical activity, and participation in sports can contribute to a higher risk of wrist injuries.
- Sports Injuries: Participation in sports, particularly those involving forceful wrist movements, can lead to sprains, strains, and fractures. Examples include tennis, basketball, and gymnastics.
- Carpal Tunnel Syndrome: While less common in adolescents compared to adults, carpal tunnel syndrome can occur, especially in those with repetitive hand movements or underlying medical conditions.
- Juvenile Rheumatoid Arthritis: This inflammatory condition can affect the wrist, causing pain, swelling, and stiffness. It’s crucial to recognize these symptoms early for appropriate management.
Wrist Pain in Older Adults
Wrist pain in older adults can stem from a variety of factors, including age-related changes in the joints, underlying medical conditions, and the cumulative effects of a lifetime of activity.
- Osteoarthritis: This degenerative joint disease is a common cause of wrist pain in older adults, characterized by the breakdown of cartilage within the joint.
- Rheumatoid Arthritis: This autoimmune condition can affect the wrist, leading to chronic inflammation, pain, and stiffness. It’s crucial to recognize the symptoms early to prevent joint damage.
- Fractures: Falls are more common in older adults, increasing the risk of wrist fractures. The healing process can be slower in this population, requiring careful monitoring.
Impact of Age on Healing
The healing process varies significantly based on age. Children generally have a faster healing rate than adults. In older adults, factors such as decreased bone density and reduced blood flow can prolong the healing time and increase the risk of complications.
Common Causes of Wrist Pain in Different Age Groups
| Age Group | Common Causes |
|---|---|
| Children (0-12) | Growth plate fractures, repetitive strain injuries, infections |
| Adolescents (13-19) | Sports injuries, carpal tunnel syndrome, juvenile rheumatoid arthritis |
| Older Adults (60+) | Osteoarthritis, rheumatoid arthritis, fractures, cumulative trauma |
When to Seek Medical Attention
Wrist pain, while often manageable with home remedies and rest, can sometimes signal a more serious underlying issue. Knowing when to seek immediate medical attention is crucial for preventing complications and ensuring proper diagnosis and treatment. Ignoring persistent or severe wrist pain could delay necessary care, potentially leading to long-term problems.Understanding the potential severity of wrist pain and recognizing the symptoms that require immediate medical attention can save time and potentially prevent complications.
This section details the crucial situations where prompt medical intervention is necessary.
Urgent Medical Attention Required for Wrist Pain
Early intervention is vital for conditions that might otherwise lead to long-term disability or require complex procedures. Prompt diagnosis and treatment are essential for optimal outcomes.
- Severe or persistent pain that significantly limits movement and daily activities.
- Wrist pain accompanied by numbness or tingling in the hand or fingers.
- Pain that develops suddenly and intensely, particularly if associated with trauma like a fall or impact.
- Pain that worsens progressively over time, especially if accompanied by swelling, redness, or warmth.
- Wrist pain accompanied by fever, chills, or other systemic symptoms, such as nausea or vomiting.
- Swelling or deformity in the wrist, especially if accompanied by pain or restricted movement.
- Inability to move the wrist or fingers, or a significant decrease in strength.
- Visible deformity or dislocation of the wrist joint.
- Symptoms that suggest infection, such as redness, warmth, pus discharge, or fever.
Symptoms Requiring Immediate Medical Attention
Recognizing the specific symptoms that warrant immediate medical attention is critical for timely diagnosis and treatment. Prompt intervention can prevent long-term problems and complications.
| Symptom | Description | Possible Underlying Condition |
|---|---|---|
| Severe, sudden pain | Intense, immediate pain, often associated with trauma | Fracture, dislocation, ligament tear |
| Numbness or tingling | Loss of sensation in the hand or fingers | Nerve compression, fracture |
| Significant swelling | Excessive swelling, redness, warmth around the wrist | Fracture, inflammation, infection |
| Inability to move the wrist | Complete or partial loss of wrist movement | Fracture, dislocation, nerve damage |
| Visible deformity | Change in the shape or alignment of the wrist | Fracture, dislocation |
Signs of a Potential Serious Condition
Recognizing signs that indicate a potential serious condition, such as infections or fractures, is critical for prompt medical intervention. Early diagnosis can lead to better treatment outcomes and reduce the risk of long-term complications.
“Persistent wrist pain, especially if accompanied by other concerning symptoms, should always be evaluated by a medical professional.”
Prompt medical attention is vital for serious conditions. Examples include infections, nerve damage, or vascular problems.
Conclusive Thoughts
In conclusion, wrist pain causes symptoms and treatments are diverse and multifaceted. Whether your pain is acute or chronic, understanding the potential causes, recognizing the symptoms, and exploring the various treatment options is key to effective management. Remember, early diagnosis and appropriate treatment are crucial for a swift recovery and prevention of long-term issues. Always consult with a healthcare professional for personalized advice and guidance.