Heel pain information and causes are crucial for understanding this common ailment. It impacts daily life significantly, and various factors contribute to its development. Different types of heel pain exist, each with its own set of symptoms, including plantar fasciitis, heel spurs, and Achilles tendinitis. This comprehensive guide explores the underlying causes, diagnostic processes, and effective treatment options for each condition.
This article delves into the common causes of heel pain, ranging from anatomical issues like flat feet to lifestyle factors such as overuse and improper footwear. We’ll also discuss medical conditions that can contribute to heel pain, providing a clear picture of the various contributing elements. Understanding these factors is essential for effective diagnosis and treatment.
Introduction to Heel Pain
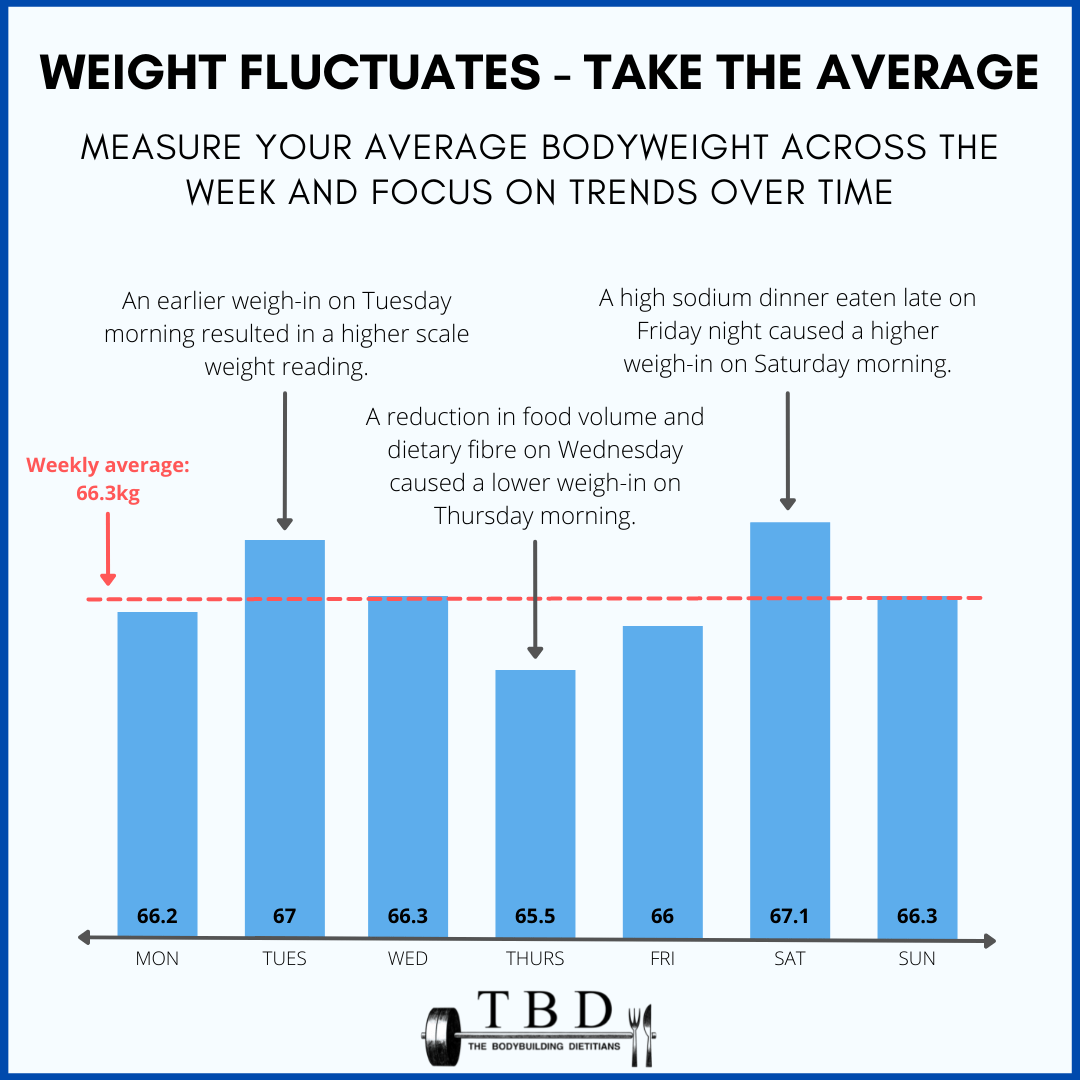
Heel pain is a common ailment affecting individuals of all ages and activity levels. It can significantly impact daily life, from simple activities like walking to more strenuous exercises. Understanding the different types of heel pain and their causes is crucial for effective diagnosis and treatment. The discomfort can range from mild annoyance to debilitating pain, limiting mobility and overall well-being.Heel pain often stems from overuse, improper footwear, or underlying medical conditions.
Identifying the specific cause is essential for choosing the right course of action. This guide explores the common types of heel pain, their characteristic symptoms, and potential contributing factors.
Types of Heel Pain
Different types of heel pain have varying causes and symptoms. This section provides a breakdown of the most prevalent conditions.
Ever wondered about heel pain? It’s often caused by plantar fasciitis, or other issues like stress fractures. But did you know that the heat from a sauna might actually play a role in recovery? Choosing the right timing for sauna use before or after your workout can significantly impact your recovery. Understanding the best time to use a sauna is key for managing conditions like heel pain.
Check out this helpful guide on sauna before or after workout to learn more about how sauna use can affect your workout and overall health. In the end, proper care and understanding the causes of heel pain are crucial for effective management.
| Type of Heel Pain | Symptoms | Possible Causes |
|---|---|---|
| Plantar Fasciitis | Heel pain, especially in the morning, stiffness, pain that worsens with activity. The pain is often described as a sharp, stabbing sensation, commonly located near the heel. | Overuse, flat feet, tight calf muscles, improper footwear, and prolonged standing or walking are among the most common contributors. Individuals with high arches or those who engage in activities that place repetitive stress on the plantar fascia are also at increased risk. |
| Heel Spurs | Heel pain, sometimes accompanied by a bony growth on the heel. This growth, called a spur, is often not painful in itself but can irritate the surrounding tissues, leading to pain. The pain may be dull and persistent, or it may be sharp and localized. | Plantar fasciitis is a frequent precursor to heel spurs. Overuse, improper footwear, and biomechanical issues, such as flat feet or high arches, can contribute to the development of heel spurs. Individuals with certain medical conditions, like arthritis, may also be more susceptible. |
| Achilles Tendinitis | Pain and stiffness along the back of the heel and Achilles tendon, often worse after activity. The pain may be described as a burning or aching sensation. It may also feel like a tenderness or tightness around the tendon. | Overuse from running or jumping, improper stretching routines, and ill-fitting or worn-out footwear can all contribute to Achilles tendinitis. Tight calf muscles can also put excessive strain on the tendon. Certain medical conditions or underlying health issues may also play a role. |
Understanding the Symptoms
Recognizing the symptoms associated with each type of heel pain can help in early diagnosis and appropriate treatment. A thorough understanding of these symptoms allows for quicker intervention and prevents potential long-term complications.
- Plantar Fasciitis: Morning stiffness and pain that increases with activity are characteristic. Pain is frequently located near the heel and often described as sharp or stabbing.
- Heel Spurs: Heel pain is the most common symptom, sometimes accompanied by a bony growth on the heel. The pain might be dull and persistent or sharp and localized, depending on the individual case.
- Achilles Tendinitis: Pain and stiffness along the back of the heel and Achilles tendon are key indicators. The pain often worsens after activity, such as running or jumping.
Causes of Heel Pain

Heel pain can be a debilitating condition, significantly impacting daily activities. Understanding the various factors that contribute to this discomfort is crucial for effective diagnosis and treatment. Knowing the root cause empowers individuals to take proactive steps towards alleviating pain and restoring mobility.Heel pain isn’t a single entity; rather, it’s a symptom of underlying issues. These problems range from simple lifestyle choices to more complex medical conditions.
This section delves into the diverse causes of heel pain, highlighting the importance of proper footwear and comparing the common culprits like plantar fasciitis, heel spurs, and Achilles tendinitis.
Foot Structure
The anatomy of your foot plays a critical role in heel pain. Variations in foot structure can predispose individuals to stress and strain on the supporting tissues of the heel. Conditions like flat feet, where the arch collapses, or high arches, where the arch is abnormally elevated, can alter the distribution of weight, leading to increased pressure and irritation.
Bunions, characterized by a bony bump on the joint of the big toe, and hammertoes, where the toes are bent abnormally, can also contribute to heel pain by affecting the overall biomechanics of the foot.
Lifestyle Factors
Certain lifestyle choices significantly impact heel health. Overuse, particularly from excessive running or repetitive activities, can lead to inflammation and micro-tears in the tissues surrounding the heel. A lack of proper stretching and warm-up routines can also weaken the supporting muscles and ligaments, making them more susceptible to injury. Obesity increases the overall stress on the heel and related structures, while prolonged standing puts continuous pressure on the plantar fascia and other foot tissues.
Heel pain can be a real drag, right? Understanding the causes is key to finding relief. Sometimes, it’s not just about your feet; your diet might play a role. Are you getting enough fiber? Consider checking out 4 signs you re not eating enough fiber for some insights.
A balanced diet, rich in fiber, can help with overall health, including potentially reducing inflammation that can contribute to heel pain. So, digging into heel pain information and causes might just involve looking beyond your feet.
These factors all contribute to the development of heel pain.
Improper Footwear
Ill-fitting or inappropriate footwear is a significant contributor to heel pain. Shoes lacking proper arch support can lead to overpronation (rolling inward) or supination (rolling outward) of the foot, placing excessive strain on the plantar fascia and other structures. High heels, while fashionable, can alter the foot’s natural alignment, causing an unnatural distribution of weight, and increasing the risk of heel pain.
Choosing shoes that adequately support the foot’s natural movement is vital for preventing heel pain.
Medical Conditions
Various medical conditions can contribute to heel pain. Arthritis, encompassing various inflammatory joint conditions, can affect the joints in the foot and ankle, leading to pain and stiffness. Nerve entrapment, where a nerve is compressed, can cause pain radiating to the heel area. Inflammatory diseases, such as rheumatoid arthritis or gout, can also manifest as heel pain.
These conditions often require medical intervention for proper diagnosis and treatment.
Heel pain can stem from various issues, like plantar fasciitis or bone spurs. Understanding the causes is key to finding relief. Sometimes, dietary choices can affect other health concerns, like diverticulitis. For example, learning which foods to avoid with diverticulitis can significantly impact your well-being. foods to avoid with diverticulitis can help you make informed decisions about your diet.
Ultimately, consulting a doctor is crucial for accurate diagnosis and personalized treatment plans for heel pain.
Comparison of Common Heel Pain Causes
| Cause Category | Possible Causes | Impact on Heel Pain ||—|—|—|| Foot Structure | Flat feet, high arches, bunions, hammertoes | Increased stress on the plantar fascia, Achilles tendon, and other foot structures. || Lifestyle Factors | Overuse, lack of stretching, obesity, prolonged standing | Increased strain and inflammation on the heel. || Medical Conditions | Arthritis, nerve entrapment, inflammatory diseases | Can cause persistent or recurring heel pain.
|
Plantar Fasciitis, Heel Spurs, and Achilles Tendinitis
Plantar fasciitis involves inflammation of the plantar fascia, a thick band of tissue running along the bottom of the foot. Heel spurs, bony growths on the heel bone, are often associated with plantar fasciitis but are not always the primary cause of pain. Achilles tendinitis involves inflammation of the Achilles tendon, the thick tendon connecting the calf muscles to the heel.
While these conditions share a common location, their underlying causes and treatment approaches differ. For instance, plantar fasciitis often results from overuse or improper footwear, whereas Achilles tendinitis can be caused by sudden increases in activity levels. A thorough assessment by a healthcare professional is essential to pinpoint the specific cause of heel pain.
Diagnosis and Treatment Options: Heel Pain Information And Causes
Heel pain can be a debilitating condition, significantly impacting daily activities. Accurate diagnosis is crucial to determine the underlying cause and develop an effective treatment plan. Understanding the diagnostic process and available treatment options empowers individuals to manage their heel pain effectively.Identifying the specific cause of heel pain often involves a multi-step process. Physicians employ various diagnostic methods to pinpoint the source of the discomfort.
This careful evaluation helps guide the most appropriate treatment strategy.
Diagnostic Methods
A thorough physical examination is the initial step in diagnosing heel pain. This includes palpating the affected area to identify tender points, assessing range of motion, and checking for any visible deformities or inflammation. The physician will also inquire about the patient’s medical history, including any prior injuries, activities, and any medications.Further diagnostic tools might include imaging studies.
X-rays can reveal bone spurs, fractures, or other bony abnormalities. Other imaging techniques like MRIs or ultrasounds can provide detailed images of soft tissues, helping to identify problems with the plantar fascia, tendons, or ligaments. These imaging techniques offer a detailed view of the soft tissue structures, providing valuable insights into the cause of heel pain.
Conservative Treatment Options
Conservative treatment approaches are often the first line of defense in managing heel pain. These methods aim to alleviate symptoms without resorting to surgery. They focus on reducing inflammation, promoting healing, and improving flexibility.
- Stretching Exercises: Regular stretching exercises are crucial for maintaining flexibility and reducing tension in the plantar fascia. Examples include heel cord stretches and calf stretches, which help to increase the elasticity of the tissues around the heel. Proper stretching techniques, combined with regular routines, can improve the overall condition.
- Ice Packs: Applying ice packs to the affected area can help reduce inflammation and pain. The application of cold therapy is a simple yet effective method to address pain and discomfort.
- Rest: Allowing the affected area to rest is essential for healing. Avoiding activities that exacerbate pain is critical in the healing process. Resting the heel allows the body to focus its resources on repairing the injured tissues.
- Over-the-counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. However, it is essential to follow the dosage instructions carefully. These medications can provide temporary relief, allowing the body to heal effectively.
- Physical Therapy: Physical therapists can provide tailored exercises and treatments to address the specific cause of heel pain. They can design individualized stretching and strengthening programs, helping to improve flexibility and stability in the foot and ankle.
- Orthotics: Custom or over-the-counter orthotics can provide support and cushioning for the foot, reducing stress on the plantar fascia. Properly fitted orthotics can help to reduce pressure points, providing comfort and preventing further injury.
Surgical Options
In cases where conservative treatments fail to provide adequate relief, surgical intervention may be considered. Surgery is typically reserved for severe cases of heel pain that have not responded to other therapies.
- Plantar Fasciotomy: This surgical procedure involves releasing the tight plantar fascia. This can alleviate pressure and pain, but carries the risk of complications like nerve damage and potential recurrence of the condition. It is crucial to weigh the benefits against the potential risks in making this decision.
Summary Table
| Diagnostic Tools | Conservative Treatments | Surgical Options |
|---|---|---|
| Physical examination, X-rays, and imaging studies. | Stretching exercises, ice packs, rest, and over-the-counter pain relievers, physical therapy, and orthotics. | Surgery for severe cases, such as plantar fasciotomy. |
Prevention Strategies
Preventing heel pain often involves proactive measures to strengthen supportive structures and avoid strain. A combination of appropriate footwear, tailored exercises, and mindful foot care can significantly reduce the risk of recurrence. Understanding these preventative strategies can empower individuals to maintain healthy feet and minimize the discomfort associated with heel pain.Effective prevention hinges on understanding the root causes of heel pain and implementing lifestyle adjustments.
By adopting these strategies, individuals can actively manage their risk and maintain a pain-free existence.
Footwear Selection
Choosing appropriate footwear is crucial for preventing heel pain. Proper support and cushioning are vital for absorbing impact and distributing pressure evenly across the foot. Look for shoes with supportive arches, good cushioning, and a firm heel counter. Avoid high heels, especially for prolonged periods, as they can strain the heel and surrounding tissues. Consider orthotics or inserts for additional support if needed.
Replace worn-out shoes regularly as their support and cushioning properties diminish over time.
Exercise Regimen
Consistent exercise can strengthen foot muscles and improve flexibility, which reduces stress on the heels. Incorporating exercises that target the calf muscles, plantar fascia, and intrinsic foot muscles is essential. These exercises enhance stability and support, reducing the risk of heel pain. A regular stretching routine is also critical for maintaining flexibility and preventing muscle tightness.
Stretching and Warm-up Routines
Proper stretching and warm-up routines are fundamental for preventing heel pain. Before engaging in any physical activity, warm up the calf muscles and the plantar fascia. Stretching helps improve flexibility and reduces the risk of injury. Static stretches, held for 15-30 seconds, are effective in increasing flexibility and preventing heel pain. Examples include calf stretches against a wall and plantar fascia stretches.
Strengthening Foot Muscles
Strengthening the intrinsic foot muscles, crucial for foot support and stability, is important. These muscles are often neglected, but they play a vital role in preventing heel pain. Exercises like toe raises, marble pickups, and towel curls can effectively strengthen these muscles. A gradual progression of exercises, starting with lighter weights or resistance, is key to avoiding injury.
Consistency in these exercises is essential for long-term benefit.
Illustrative Images and Visual Aids

Visual aids play a crucial role in understanding and addressing heel pain. Visual representations of healthy foot structures, various orthotics, stretching techniques, and suitable footwear provide a clear picture of the issues and solutions involved. This section will detail these visual aids, focusing on the anatomical differences, applications, and preventive measures.
Healthy Foot Structure vs. Foot with Plantar Fasciitis
Understanding the normal anatomy of the foot is essential for recognizing abnormalities associated with heel pain. A healthy foot exhibits a strong, well-aligned plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone (calcaneus) to the toes. This fascia supports the arch of the foot, absorbing shock and distributing weight evenly.
Images illustrating this healthy structure would contrast with an image of a foot exhibiting plantar fasciitis. The latter image would show inflammation and/or thickening of the plantar fascia, often accompanied by tenderness and pain around the heel. This visual comparison highlights the critical role of the plantar fascia and the structural changes that occur in the presence of plantar fasciitis.
Orthotic Types and Applications
Various orthotics are designed to address different foot issues. Images illustrating these orthotics would clearly show the different types and their application. For example, a supportive arch support would be shown in an image with an overlay highlighting its location on the foot. An image depicting a custom-molded orthotic could show the process of molding the orthotic to fit the individual’s foot, ensuring a personalized fit.
Different orthotics are designed for different types of foot conditions, such as overpronation or flat feet, or to support specific activities. Images would demonstrate how each orthotic type aligns with the specific foot condition, alleviating pain and providing stability.
Stretching Techniques for Calf Muscles and Plantar Fascia, Heel pain information and causes
Effective stretching is vital in managing heel pain. Images showcasing proper stretching techniques for the calf muscles and plantar fascia are crucial for understanding the correct form and range of motion. These images should demonstrate different stretching postures, focusing on the correct positioning of the foot and leg. For example, a picture would show a person performing a calf stretch, ensuring the heel is pressed firmly against the ground, while the other leg is straight behind them.
Images demonstrating the stretch would clearly show the proper alignment and muscle engagement for a safe and effective stretch. Likewise, images showing plantar fascia stretches would demonstrate the correct way to stretch the plantar fascia to prevent tightening and pain.
Footwear for Heel Pain Prevention
Appropriate footwear plays a significant role in preventing heel pain. Images demonstrating different types of footwear suitable for heel pain prevention are essential for educating individuals on the right choices. These images would showcase supportive shoes with adequate arch support, cushioning, and a firm heel counter. Images would illustrate the differences between various shoe styles, such as running shoes, walking shoes, and sandals, highlighting their suitability for different activities and the impact they have on heel health.
Images could also show shoes with insufficient support or poor cushioning, highlighting how these choices may contribute to heel pain.
Ultimate Conclusion
In conclusion, heel pain information and causes highlight the importance of understanding the root of the problem. Whether it’s poor footwear, overuse, or an underlying medical condition, addressing the cause is key to effective treatment and prevention. By understanding the various types of heel pain, their symptoms, and possible causes, individuals can take proactive steps toward alleviating discomfort and maintaining a healthy lifestyle.
Remember to consult a healthcare professional for personalized advice.